1. Introduction
The brachial plexus is formed with integration of the anterior branches from C5 to T1, and sometimes C4 and T2 participate as well. In the axillary cavity of this network three nerves, which are medial, lateral, and posterior to the spinal cord, fall apart. They are in, outside, and behind the third part of the axillary artery, respectively. These cords are divided into several branches that innervate the upper limbs (1). Several variations of the nervous system have been reported. Knowledge of the existing variations in anatomy is very important for experts in anatomy, surgery, and radiology, as well as for medical diagnostics using computer imaging (2). For example, to prevent damage to nerves in the axilla during arm surgery, the surgeon should have precise knowledge of variations (3-5). Because of the rarity of the median nerve variations shown in this report, it is morphologically and clinically important.
2. Case Presentation
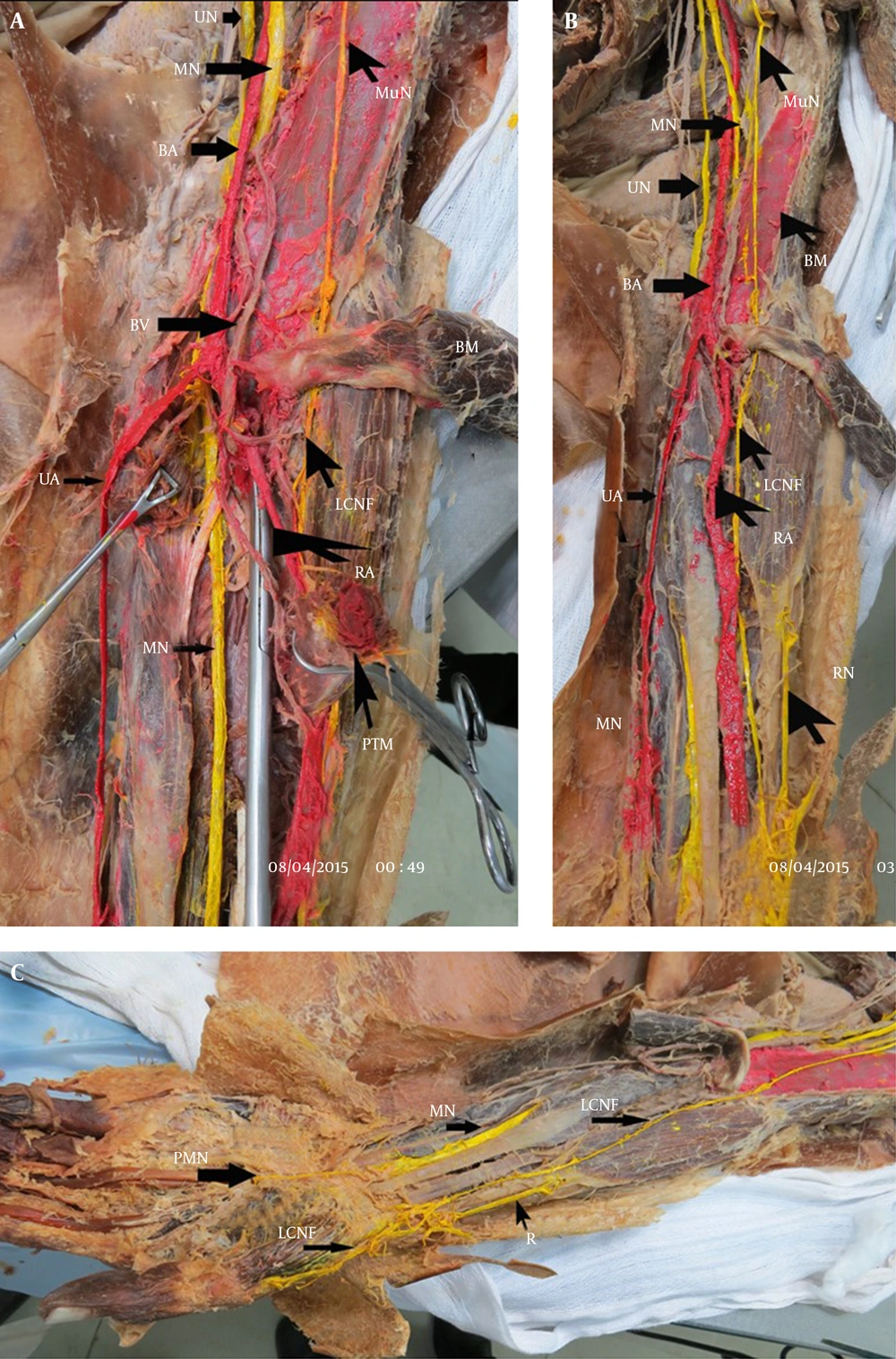
The variation was observed in the left upper limb anatomy of a 55-year-old cadaver dissected at Lorestan University of Medical Sciences, using cutting instructions from Cunningham. The median nerve, after its formation in the axilla hole, came from a different path passing through the arm area. It started initially in the brachial artery, and then passed posterior to the artery and outside of it, into the depth of the brachialis muscle. From there, it continued its path to the cubital fossa, left the brachialis muscle thickness of the posterior brachial artery, and moved inward to end up located inside of it. The musculocutaneous nerve, after separation from the lateral cord of the brachial plexus and piercing the coracobrachialis muscle, was located between the biceps and brachialis muscles, entered the forearm as a lateral cutaneous nerve, continued its path to the wrist, and finally entered into the posterolateral hand. Normally, the median nerve on the inside of the arm comes down vertically between the hole in the brachialis muscle and biceps in the arm. At the beginning of its path it is located outside of the brachial artery, in the middle of arm it passes from the front of the artery and continues inside. The musculocutaneous nerve pierces the deep fascia above the elbow and continues in the cutaneous external forearm (6).
3. Discussion
Some anatomical variations can be clinically valuable, and the variations in the median nerve presented here are important because of their anatomical position and the significant body of research on this area. In 1992 Le Minor described five relationships between the musculocutaneous and median nerve based on the coracobrachialis muscle. Subsequently, Venierators reported three other relationships between these two types of nerve and the aforementioned muscle. Hassanzadeh et al. observed that the lateral root of the median nerve in the lower half of arm attached to the medial root, and this nerve ran its natural path (7). In 1848 and 1854, John Struthers published studies about pressure on the median nerve from the armpit to the elbow. This research reported some studies about median nerve compression by a ligament and a spine in the supracondylar process area of the humerus (8). This spine condition is seen congenitally (4). In 1383, for the first time in Iran, Forough et al. reported a case of compression of the median nerve in the area of the supracondylar humerus.
In this study, the position of the median nerve was in the anterior of the third part of the axillary artery, with attachment of internal and external roots of the medial and lateral cords of the brachial plexus. Compare this with Hassanzadeh et al., who declared the commissure of internal and external root of median nerve as half of the lower arm (7). In this report the position of the formation of the nerve in the axillary cavity was completely natural, but the path of the nerve’s movement in the arm started in the brachial artery, passed through the posterior artery, and continued its path out of the depth of brachial muscle toward the cubital path. Finally, after leaving the muscle thickness it moved inwards from the brachial artery and was located inside of the arteries. The path of movement was not reported in the previous studies, and it seems that the variations mentioned in this study are very rare.
This report indicates that given the direction of the median nerve’s movement path in the depth of the brachialis muscle and its close proximity to the humeral shaft, the risk of nerve damage is high for fractures of the humerus, so surgeons should be aware of these anatomical variations to perform the appropriate treatment.