1. Background
Abdominal surgery is commonlyperformed both electively, usually at least one day after hospitalization, and emergency, that is without prior preparation (1). Postoperative pain is considered as one of the most unfavorable complications experienced by patients who undergo surgery and it has been discussed for many years as a health care problem (2). Severe postoperative pains usually occurdue to large incisional surgeries in abdomen, chest, and orthopedics (3). Postoperative pain is an acute pain related to the area of the operation, patient's physiology and psychological situation and the degree of tissue manipulation and damage (4). Postoperative pain can cause adverse effects such as increased atelectasis, thromboembolism, myocardial ischemia, cardiac arrhythmias, water and electrolyte disturbances, urinary retention, intestinal ileus, psychological distress and serious physiologic effects that may result in potentially life-threatening postoperative complications (5, 6).
Poor control of pain could also cause prolonged hospitalization and higher medical costs for patients and insurance companies and may cause patients’ dissatisfaction; on the other hand, pain relief can lead to rapid intestinal peristalsic movements and accelerate oral intake (4). Thus, proper pain relief is a major concern of care providers in postoperative units.
There are various methods to relieve pain including pharmacological and non-pharmacological interventions. The most important and most common ways to relieve painis using analgesics in a variety of ways, including oral, intravenous, intramuscular, subcutaneous, subcutaneous continuous infusion, etc. Opioids are the most commonly used agents for postoperative pain management (6), and yet postoperative pain management is often limited by adverse effects of opioid. When used alone in large doses for an extensive period, opioid can lead to acute tolerance which further impairs pain control and, more seriously, respiratory and hemodynamic depression (7). Patient-controlled analgesia (PCA) addresses many of the safety and efficacy issues associated with opioid use in the postoperative period (6). PCA is a technic to deliver analgesia via a programmable pump: the patient himself chooses to self-administer a bolus dose; upon patient initiation of an activation button attached by a cord to the PCA pump, a small dose of opioid is delivered by an intravenous (IV) line to an indwelling catheter (8).
Different studies advocate PCA superior to conventional nurse-controlled analgesia with less risk for patients (9-11). However, findings are conflicting, Ballantyne in his meta-analysis found a strong patient preference for PCA over conventional analgesia, but disclosed no differences in analgesic consumption or length of postoperative hospital stay, and a small but statistically significant benefit upon pain intensity. Whereas.Walder’s review did not find a significant differences in pain intensity and pain relief between PCA and conventionally treated groups. Hudcovaet al. in their meta-analysis found better pain control, greater patient satisfaction, and higher amounts of opioid consumption in PCA group than in the control group (12).
2. Objectives
However,in spite of the importance of this subject and the fact that the majority of patients are suffering from postoperative pain, there are conflicting ideas about PCA in general, and a lack of study on patients' self-controlled analgesia in Iran specifically; therefore,the current study primarily aimedto compare the effects of PCA and the routine methods on the intensity of postoperative pain in abdominal surgeries.
3. Patients and Methods
The current study was performed in Amir-al-momenin Hospital (a non-educational hospital) in Ahvaz, Iran, in 2009 on patients who underwent elective abdominal surgery. It was a one-way blinded, placebo-controlled, interventional study and pain relief was evaluated between Patient-controlled Analgesia (PCA) technique and routine methods.
A total of 60 candidates for appendectomy and herniorrhaphy who met the inclusion criteria were selected purposefully. Then they were randomly divided into two groups based on their hospital file numbers being even or odd.
Inclusion criteria included: age range 18 to 68 years, willing to participate in the study, being able to speak in Farsi, without chronic painor chronic diseases, and BMI less than 30. Exclusion criteria included: positive history of liver and renal diseases, sensitivity to drugs, oral or parenteral addiction to opium, and positive history of psychological diseases. Written consent letters were obtained from all participants and they were ensured that their privacy would be preserved, there were no expenses for the patients, and that they were free to participatein the study. The study was approved by the Research Committee of Ethics in Ahvaz Jundishapur University of Medical Sciences.
Pain rate was measured on the time of admission and also every six hours post operation for both the PCA and control groups. The analgesic pump contained 0.1 mg/kg of pethidinein 50 mL 0.9% normal saline, administeredin the PCA group. The pump infused 2 mL/hour serum containing analgesic according to physician's prescription. The PCA group were trained to press the infusion pumps button to get more drug if necessary (0.5 mL solution containing analgesic drug with every pressing) as soon as the pain started. Safety of the PCA system was considered as the pump was acting like a lock with locking interval of 15 minutes at each time to prevent excessive doses of the analgesic. The control group was trained to press alarm to call the attending nurses for administration of intramuscular analgesic drug (0.5 mg/kg pethidine) when they felt pain. Groups were blinded as microsites containing 100mL normal saline with no analgesic (placebo) in the control group, and some serum at the time of feeling pain in the control group were administered.
Pain severity was measured for each group by the visual analog scale (VAS) after enrolling all subjects and every six hours, the mean score of pain severity in both groups was and compared at different times. Vital signs and adverse effects of analgesic drugs were recorded in a checklist at the time of admission and then every six hours for both PCA and control groups.
In the current study, data collection tool contained four sections. First section included demographic data such as age, gender, marital status, education level, occupation and past medical history. The second section contained questions about recent operation, for example type and duration of the surgery, anesthesia method, medications, and dosage of analgesic used during anesthesia and recovery. The third section included questions about pain intensity based on VAS scale, vital signs, amount of analgesic drugs used, and their side effects such as nausea and drowsiness after admission. The fourth section included patients’ feedback to PCA and routine analgesic procedures.
In order to evaluate the pain and nausea intensity after surgery, postoperative pain visual analog scale was utilized. The pain considered mild, if between zero to 30 mm, moderate between 30 and 60 mm, and severe between 60 and 100 mm. In order to measure drowsiness, zero was considered none, number one was mild (sometimes drowsy), number two was moderate (often drowsy) and number three was considered severe (drowsy and hardly remain awake).
In order to assess the severityof nausea, it was considered mild if patients recorded zero to 30 mm, moderate between 30 and 60 mm, and severe between 60 and 100 mm. In order to evaluate the scientific validity of the questionnaire, content validity method was used. In the current study, visual analogy scale (VAS) was used to assess the pain and nausea severity. VAS has global validity and reliability and is applied in many studies. Version 16 of SPSS software was employed to assess the measured data for descriptive and analytical statistics. Descriptive statistics used to describe the variables included: frequency, percentage, means and standard deviation.
In order to analyze the data and homogeneity of the demographic variables, and also to evaluate the satisfaction and amount of analgesic taken in the two groups, chi-square and t-test with 95% of confidence intervals were used.
The Ethics Committee of Ahvaz Jundishapur University of Medical Sciences approved the study design (p/8/20/3114). Both the Purpose and method of the research were described for the participants, and informed consent to participate in the study was obtained from all of them.
4. Results
The mean age and weight of PCA and control groups were 42.3 ± 10.55 and 41.93 ± 11.57 years, and 70.87 ± 9.48 and 73.37 ± 10.38 kg, respectively. These results show that the two groups did not have any statistical differences regarding age, gender, marital status, education and occupation (P > 0.05)(Table 1). According to the chi-square test, no significant difference was observed between the two groups regarding past medical history such as previous surgeries and history of hospitalization, type of current surgery, and anesthesia method (P > 0.05). Also, there was no difference (P > 0.05) between the two groups regarding the age and weight (Table 1).
| Variables | Control Group, n = 30 | PCA Group, n = 30 | PValue |
|---|---|---|---|
| Age | 0.89 | ||
| < 30 | 7 (23.4) | 5 (16.7) | |
| 30-40 | 4 (13.3) | 6 (20) | |
| > 40 | 19 (63.3) | 19 (63.3) | |
| Gender | 0.77 | ||
| Male | 22 (73.3) | 21 (70) | |
| Female | 8 (26.7) | 9 (30) | |
| Marital status | 0.40 | ||
| Single | 6 (20) | 4 (13.8) | |
| Married | 24 (80) | 25 (86.2) | |
| Education | 0.52 | ||
| Primary | 16 (53.3) | 12 (40) | |
| High school | 2 (6.7) | 1 (3.3) | |
| Diploma | 6 (20) | 9 (30) | |
| University education | 6 (20) | 8 (26.7) | |
| Occupation | 0.46 | ||
| Self-employer | 15 (50) | 16 (53.3) | |
| Employed | 6 (20) | 7 (23.3) | |
| Housekeeper | 5 (16.7) | 6 (20) | |
| Retired | 4 (13.3%) | 1 (3.3%) | |
| Hospitalization history | 0.1 | ||
| No | 13 (43.3) | 7 (23.3) | |
| Once | 8 (26.7) | 12 (40) | |
| Two times | 6 (20) | 7 (23.3) | |
| More than two times | 3 (10) | 4 (13.3) | |
| History of surgery | 0.54 | ||
| No | 24 (80) | 22 (73.3) | |
| Once | 6 (20) | 7 (23.3) | |
| Two times | 0 (0) | 1 (3.3) | |
| Surgery type | 0.34 | ||
| Herniorrhaphy | 21 (70) | 23 (76.7) | |
| Appendectomy | 9 (30) | 7 (27.3) | |
| Anesthesia method | 0.34 | ||
| Spinal | 21 (70) | 23 (76.7) | |
| General | 9 (30) | 7 (27.3) |
a Values are presented as No. (%).
Based on independent t-test, there was no significant difference between the PCA and control groups regarding the mean of postoperative vital signs, and the six and 12 hours after surgery vital signs (P > 0.05), but significant difference was observed regarding systolic blood pressure 12 hours after surgery between the two groups (P = 0.03).
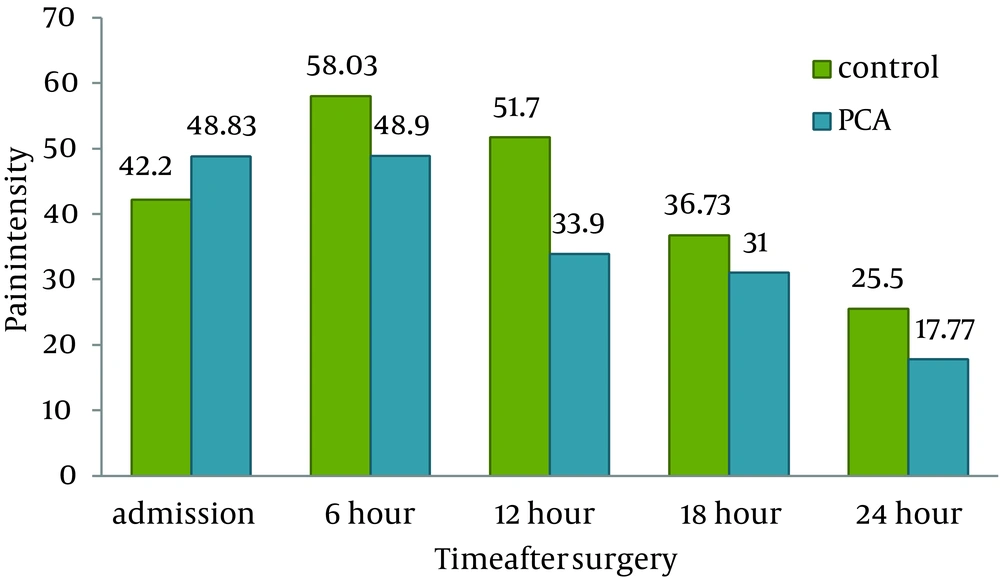
There was no significant difference between the two studied groups concerning post-operative pain 18 and 24 hours post-operation (P > 0.05). There were significant differences after six hours (P = 0.001) and 12 hours (P = 0.001), and also between entrance to the ward and 24 hours of post-operation (P = 0.001) between the PCA and control groups (Table 2).
| Time, h | Control Group | PCA Group | P Value |
|---|---|---|---|
| After admitting to the ward | 42.2 ± 16.94 | 48.83 ± 17.85 | 0.74 |
| 6 hours after operation | 58.03 ± 19.07 | 48.90 ± 10.63 | 0.001 |
| 12 hours after operation | 51.70 ± 20.47 | 33.90 ± 9.21 | 0.001 |
| 18 hours after operation | 36.73 ± 15.63 | 31 ± 12.07 | 0.38 |
| 24 hours after operation | 25.50 ± 9.68 | 17.77 ± 7.45 | 0.09 |
| From the time of admitting until 24 hours post operation | 42.83 ± 20.11 | 36.08 ± 16.72 | 0.001 |
a Values are presented as Mean ± SD.
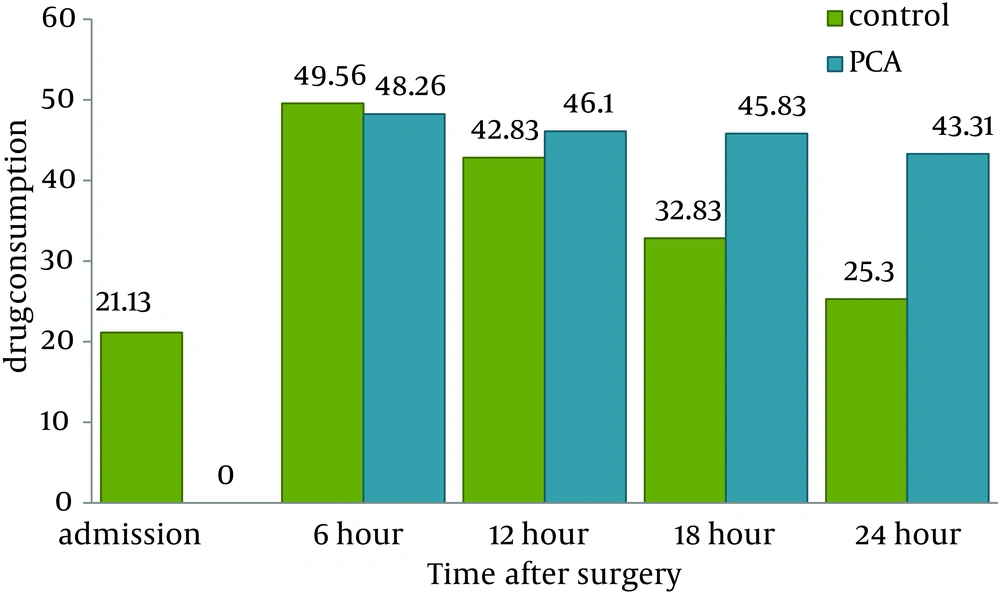
Based on the t-test results, a significant difference was observed concerning the drug dosage used at the time of entrance to the ward, 18, and 24 hours after surgery (P = 0.001), but there was no significant difference at six and 12 hours postoperative hospitalization of the medicine usage(P > 0.05). The t-test showed no significant difference (P = 0.001) concerning the patients’ average drug use from early hospitalization until 24 hours after surgery between groups (Table 3).
| Time of Drug Administration, h | Control Group, n = 30 | PCA Group, n = 30 | P Value |
|---|---|---|---|
| After admitting to the ward | 21.13 ± 18 | 0 ± 0.00 b | 0.0001 |
| 6 hours | 49.56 ± 17.82 | 48.26 ± 8.41 | 0.71 |
| 12 hours | 42.83 ± 20.06 | 46.10 ± 10.09 | 0.42 |
| 18 hours | 32.83 ± 27.57 | 45.83 ± 6.24 | 0.0001 |
| 24 hours | 25.30 ± 21.37 | 43.31 ± 5.95 | 0.0001 |
| From the time of admitting until 24 hours post operation | 173.56 ± 23.52 | 183.50 ± 19.73 | 0.001 |
a Values are presented as Mean ± SD.
bNone of the PCA group patients received analgesics at this point of time.
The current study assessed the side–effects of drug (pethidine) such as nausea and drowsiness on the patients in the PCA and control group. Based on the chi-square test results, no significant difference was observed regarding the time intervals including 6, 12, 18, and24 hours after surgery by considering the above mentioned parameters (P > 0.05).
The mean of pain intensity in the PCA group was lower than that of the control group at 6, 12, 18 and 24 hours after surgery and this rate was just higher than that of the control group after admissionto the ward in the hospital (Figure 1).
The mean of analgesic drugs taken in the PCA group was lower than that of the control group after admission to the ward and six hours after surgery, but it was higher than that of the control group 12, 18 and 24 hours after abdominal surgery (Figure 2).
5. Discussion
In the current study Patient-controlled analgesia was compared with intramuscular injection analgesics to manage pain. The study results showed the effectiveness of the PCA method to decrease patients' pain intensity and dosage of analgesic consumption, compared with the routine method of pain relieving.
Bayar et al. compared postoperative pain, analgesic consumption, and treatment satisfaction between 16 patients treated with intravenous patient-controlled analgesia (IV-PCA) and 15 patients treated with intramuscular analgesics after laparoscopic ovarian cystectomy. They showed that the mean of pain intensity in the PCA group was higher than those of the control group patients administered intramuscular analgesic. Despite the higher pain scores obtained by the IV-PCA group, self-reported satisfaction rates were higher in this group. They concluded that, involvement of patients in their pain management might increase the awareness of pain, but it significantly improved their satisfaction with the control of postoperative pain. The results of the current study were not in line with those of Bayar et al. This discrepancy may be due to times of pain evaluation, gender differences, as in the current study most of the patients were male, and difference in the type of surgery in the two studies (13).
Results of the study by Vengadesh et al. in which 62 patients undergoing abdominal operations were randomly divided into the PCA and intramuscular (IM) groups, showed no significant difference regarding the severity of pain between the two intramuscular injection and PCA groups. The total morphine consumption of the PCA group was significantly lesser than that of the IM group at different intervals in the postoperative period. The PCA group had better pain relief compared to the IM group. Their findings are in line with those of the current study because of approximate similarity in the methodology, and surgery region in the two studies (12, 14, 15).
Thurlow et al. compared PCA and interval analgesia methods on labor pain relief. Similar to the current study findings, they observed significant difference between the PCA and intramuscular injection of analgesics in the intervention and control groups, as the pain scores were lower in the PCA group compared with those of the intramuscular injection group. They concluded that analgesic injection via PCA relieved the pain of laboring mothers better than the intramuscular analgesic injection (1, 16).
The current study observed a significant difference between the two studied groups regarding the dosage of drug taken by patients during postoperative time until 24 hours, which was similar to that of the study by Vengadesh. They compared the effects of PCA and conventional methods on pain relief and their findings presented that the mean of morphine dosage in the PCA group was lower than that of the patients with intramuscular injection. This result was not similar to that of the current study; it could be because of differences between the analgesic drug types and their dosages. Also, Vangadesh et al. did not observe significant difference between patients concerning drowsiness, breathing disorders, and nausea severity (14).
Everettet al. studied the rate of analgesic drugs dosage in the PCA and intramuscular injection groups in Australia. The results showed that the mean amount of medication within three days after operation in the PCA was higher than that of the intramuscular group (17).
Chang et al. studied the expenses of PCA and routine methods. Similar to the current study findings, a higher amount of analgesic was used in the PCA group, due to easier accessibility of analgesics in this method, and also due to worrying about the painfulness of the intramuscular injection in the control group (18).
In conclusion, the current study findings showed that Patient Controlled Analgesia (PCA) was superior to routine method in case of pain relief and patients’ satisfaction after the surgery. Therefore the PCA method can be recommended to decrease post-operative pain intensity.
The current study had strengths and weaknesses. Its strengths included being one- way blinded, with control group interventional method. The current study will improve clinical nurses' knowledge of pain management. Similar to the other studies, the current one also had limitations. Excluding the patients who could not speak Farsi and non-blinded researcher are limitations of the current study. To assess the effects of some other analgesics, it is recommended to conduct this method with the other conditions of pain, and compare this method with the newer methods of pain control.