1. Background
Although, an accurate statistic for stroke prevalence is not available in Iran, the stroke is the most common cause for patient’s hospitalization in neurology wards, and it is the third cause for patients’ mortality (1, 2). A review study showed a divergent and statistically significant trend in the stroke incidence rates over the past four decades. Therefore, in high-income countries 42% decrease was observed in stroke incidence and more than 100% increase in stroke incidence was found in low to middle income countries. From 2000 to 2008, the overall stroke incidence rates in low to middle income countries exceeded more than 20% (3). This phenomenon is an acute neurological injury, caused by disturbed blood supply to a part or some parts of the brain tissue, which occurs in ischemic and hemorrhagic forms. Depending on the location and the extent of brain injuries, these damages lead to the loss of brain normal functions and may create different types of speech and language disorders. These disorders include: cognitive problems, dysarthria, apraxia and aphasia (4). Aphasia is the most common speech disorder caused by a stroke. The studies showed that almost one third (23% to 33%) of the patients with stroke suffer from one kind of aphasia (5). The aphasia is caused by acquired damages to the brain parts that are responsible for linguistic functions and has symptoms such as: disorder in auditory perception, speech, naming, verbal repetition, reading and writing. These disorders are visible in a wide spectrum, from mild to severe (4, 6). Based on the clinical features of the speech and cognitive functions of the patients, the neurologists and speech therapists can determine the different types of aphasia. In Table 1, a summary of the reserved capabilities and speech-language disorders of aphasic patients are demonstrated (7).
| Type of Aphasia | Speech Criteria | ||
|---|---|---|---|
| Speech Fluency | Auditory Perception | Verbal Repetition | |
| Global | − | − | − |
| Broca | − | + | − |
| Wernicke | + | − | − |
| Conduction aphasia | + | + | − |
| Motor transcortical aphasia | − | + | + |
| Sensory transcortical aphasia | + | - | + |
Speech and Language Criteria to Determine Aphasia Type
The risk factors of the stroke can be divided into two categories: a series of some uncontrollable factors that include age, gender, race, genetics and family history (8-10). Naturally, these factors cannot be changed or controlled by the individuals in the society. But, by handling some other factors, the risk of stroke and its associated speech and linguistic disorders (aphasia) can be diminished. These factors are preventable, and they include: high blood pressure, diabetes, lack of exercise, smoking, elevated cholesterol, obesity, cardiovascular diseases, and drug and alcohol abuse (11, 12). Apart from these factors, other factors also seem to involve in the occurrence of stroke-induced aphasia.
The time and climatic features in the incidence of stroke and aphasia are among these factors, which were vastly studied in some countries (13-19). According to the statistical information in Italy, the incidence of stroke is lower during the summer and is higher in the fall than in the winter (20). But, in some regions of Australia, more stroke rate is reported in the summer than in the winter (21). In Finland, the rate of cerebral-vascular attacks in men is higher on Mondays than on Sundays (22) and also another study revealed that the peak of vascular attacks is in the early hours of the morning, and then the attacks’ rate reduces in the rest hours of the day (23). However, in some other studies, no significant differences were found between the mentioned variables (24, 25). Therefore, the discrepancy and incoherence between the results of these studies are obvious. In Iran, only one study is done on the effect of seasonal variation on the incidence of thrombotic strokes in Tehran. The results showed that the incidence of stroke is doubled in the winter compared to the summer (26).
2. Objectives
The current study aimed to survey the influences of the time variation in stroke-induced aphasia in Ahvaz for several reasons. The reasons include the differences in the results of the previous studies, lack of generalizability of the findings, lack of evidence on the time variation effect on the incidence of stroke and stroke-induced aphasia in different parts of Iran, and finally the basic information on the prevalence and causing factors of aphasia can be very helpful for speech therapists to design preventing approaches and rehabilitation priorities.
3. Patients and Methods
The current study was a retrospective, sectional, and descriptive survey conducted to compare the influence of time variation (seasons of the year, days of the week, and hours of the day) in the incidence of aphasia (receptive and expressive aphasia) in patients with stroke, who referred to the Ahvaz teaching hospitals and had medical records in 2011. This study was carried out in the full enumeration format and all the 1817 patients with cerebrovascular attacks (CVAs) were studied, using their records in the archive of the educational hospitals in Ahvaz. Neurologist and speech therapist experts reviewed the records of the patients in terms of clinical symptoms, stroke, and aphasia types. One of the limitations in the study was the deficiency in the medical records, due to which researchers could not classify the types of aphasia on the basis of explained six classes. To resolve this problem, based on the information in the patients’ records and the identification criteria, the types of patients’ aphasia were divided into two major categories of receptive aphasia and expressive aphasia (7). The receptive aphasia category includes the patients suffering from severe speech perception disorders, but with fewer problems in verbal fluency. Wernicke’s, global, and sensory trance-cortical aphasia are in this category. The patients with a good verbal comprehension but an impaired verbal fluency are put in the expressive aphasia category. The Broca, transitional, and motor trance-cortical aphasia are in this category. Another limitation of this study was the time of onset and development of aphasia according to contents of their medical records. That means the data related to stroke onset time, the referral time of the patient to the hospital, and eventually admission in the ward were documented based on the reports of the patient’s companions. All ethical issues were taken into account in the records reviews. By SPSS version 16, chi-square and frequency indicators were used to describe and analyze the data at a significance level of 0.95.
4. Results
From the reviewed 1817 cases, 725 patients were diagnosed with aphasia. In other words, in 39.9% of patients with cerebrovascular attack, one type of aphasia was diagnosed. The mean age in patients with aphasia was 60 ± 12 years. 70.2% of the patients with aphasia (509 subjects) were male, and 29.8% were female (216 subjects). This means that male to female ratio of aphasia in Ahvaz was approximately 2.3 to 1.
The highest incidence of the stroke and the resulting aphasia was in summer (38.2%), and the lowest incidence rate was in spring (15.7%). The frequency of stroke in autumn and winter were 25.5% and 20.6%, respectively (Table 2).
| Type of Aphasia | Seasonsa | Chi-Square | P Value | |||
|---|---|---|---|---|---|---|
| Spring | Summer | Autumn | Winter | |||
| Receptive | 31 (17.1) | 68 (37.6) | 46 (25.4) | 36 (19.9) | 7.705 | .022 |
| Expressive | 83 (15.3) | 209 (38.4) | 139 (25.5) | 113 (20.8) | 7.812 | .028 |
| Total | 114 (15.7) | 277 (38.2) | 185 (25.5) | 149 (20.6) | 8.961 | .032 |
The Frequency of the Receptive and Expressive Aphasia Resulting From Stroke on Each Season of the Year
As shown in Table 2, The statistical comparisons using chi square test revealed significant differences between incidence of stroke-induced aphasia types between the seasons as for receptive aphasia (P = 0.022), expressive aphasia (P = 0.028), and for total incidence of all aphasia types (P = 0.032).
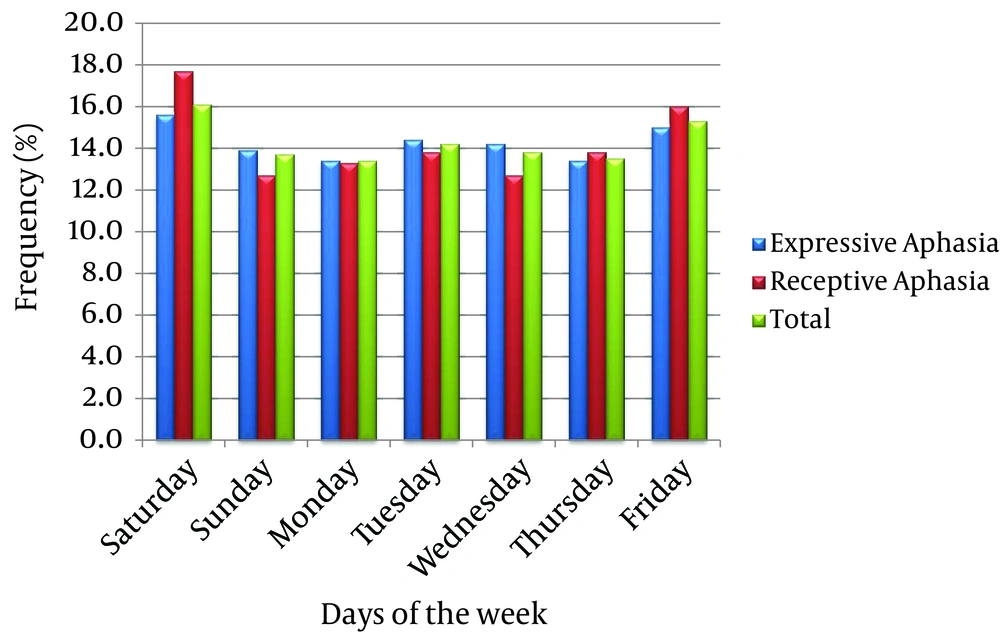
According to Figure 1, the highest incidence (16.1%) of cerebral-vascular accidents resulting in aphasia was on Saturdays (the first day of a week in Iran). After that the maximum incidence of attacks (15.3%) was on Fridays (weekend).
The paired statistical comparisons with chi-square only showed significant differences between Saturdays and the other days of the week (P < 0.05). Therefore, except Saturdays, there was no significant difference between other days of the week regarding the incidence of stroke and aphasia in the patients in Ahvaz (P > 0.05).
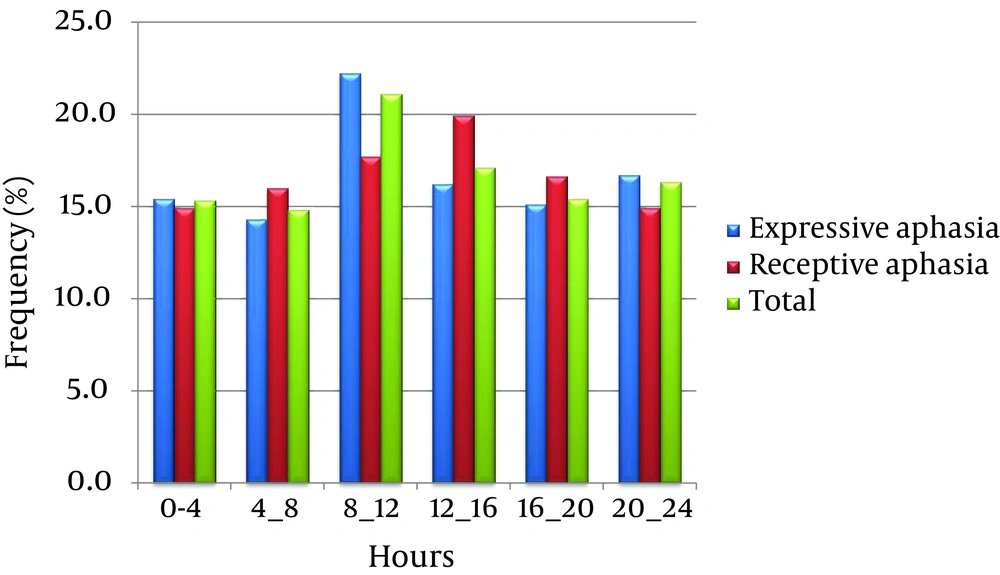
According to Figure 2, the highest incidence of stroke resulting in aphasia occurred from 8:00 AM to 4:00 PM with the attack’s peak between 8:00 AM to noon. Therefore, the 23.3% of the expressive aphasia and 17.7% of the receptive aphasia occurred from 8:00 AM to noon. 15.3%, 14.8%, 21.1%, 17.1%, 15.4%, and 16.3% of the recorded aphasia occurred between midnight to 4:00 AM, 4:00 AM to 8:00 AM, 8:00 AM to noon, noon to 4:00 PM, 4:00 PM to 8:00 PM and 8:00 PM to midnight, respectively.
Chi-square test showed a significant difference in the incidence of stroke-induced aphasia between 8:00 AM to noon and the rest hours of the day and night (P > 0.05). This difference was also observed between the afternoon hours (i.e. noon to 4:00 PM) and the other hours of the day (P > 0.05).
5. Discussion
Totally, 39.9% of the patients with stroke had one form of aphasia. According to the results of other studies in Iran, this percentage ranged from 23% to 33% (5, 7, 27) and it seems that aphasia had higher incidence in Ahvaz. The gender ratio of affected individuals with aphasia was 2.3:1 (males to females) in current study. In Hamadan, it was reported that 58.1% and 41.9% of the patients with aphasia were females and males respectively, so the gender ratio of aphasia was 1.39:1 (females to males) (5). In a study carried out in Tabriz, it was revealed that 45% of the subjects with aphasia were females and 55% were males, and that the gender ratio was 1.22:1 (males to females) (28). In Mashhad, it was reported that out of 160 subjects with aphasia, 59 ones were females and 47 were males, so the gender ratio of aphasia was 1.26:1 (females to males) (7).
In Ahvaz, summer (38.2%) and fall (25.5%) had the highest incidence of stroke-induced aphasia and statistically significant differences were observed between the seasons (P > 0.05). Inconsistent with the current study findings, the results of the study carried out in Tehran showed that the number of patients with thrombotic stroke in winter was nearly doubled in summer (26). As mentioned before, different patterns of incidence were reported for each geographical region in different studies. In some studies, no significant relationship was observed between the incidence of stroke and season of the year (24, 25), but in some countries, winter (29, 30) or summer (21, 31, 32) were introduced as the risk factor for stroke. However, a study in New Zealand found that strokes were less likely to occur during the summer and autumn than in the winter or spring (33). Researchers mentioned some reasons such as changes in blood pressure, viscosity, fibrinogen levels, the effect of the air pressure on blood circulation and the increase of infectious diseases in some seasons to justify these issues (30, 34, 35). There is evidence that lowering of blood pressure in the night either naturally or through the use of antihypertensive medications could cause ischaemic brain damage especially in the elderly patients with associated ischaemic heart disease and occlusive carotid disease (36). Despite these factors, it should be noted that effect of seasonal and weather variation on stroke incidence is still not entirely proved and systematic studies based on larger population samples are needed (34).
The current study found that the highest incidence of stroke-induced aphasia was observed on the first day of the week (Saturdays) than the other days of the week. The observed difference between incidence rate in Saturday and other days of the week was significant (P > 0.05). This finding was confirmed by the studies in other countries reporting that the first day of the week (Monday) was identified as the day with an increased risk of stroke (22, 37, 38). In a study conducted for the period of 11 years in Serbia, more ischemic stroke admissions were reported on weekdays than the weekends. However, contrary to the current study findings, this study reported minimum number of admissions on Sundays, and the maximum on Tuesdays and Wednesdays (39). Cultural and lifestyle issues such as excessive alcohol consumption on the weekend (20, 22, 23) and rashly beginning the first working day of the week with a lot of stress (20) were among reasons mentioned in similar studies. However, in some studies no significant difference was reported in the stroke incidence between the first days of the week and other days (24, 40).
The highest incidence of stroke-induced aphasia in Ahvaz occurred in the mornings from 8:00 AM to noon. In other words, 21.1% of all the cerebral-vascular accidents resulting in aphasia happened in this period. These findings were confirmed by other studies abroad (38, 41, 42). However, in the current study, another accident peak was also found from noon to 4:00 PM that included 17.1% of stroke-induced aphasia. It is still difficult to interpret and explain these findings but according to other studies, it largely reflects the impact of lifestyle on the incidence of cerebral vascular accidents. Stress and pressure of daily work in the morning and early afternoon are among the most influential factors in increasing the incidence of the stroke (23). In an interesting study in Egypt, the diurnal pattern of stroke was investigated one month before Ramadan and during Ramadan over two successive years 2007 and 2008. This study confirmed the findings from previous studies that the higher frequency of stroke onset time was from 6:00 AM to noon one month before Ramadan, whereas contrary to the previous studies, the frequency was higher from noon to 6:00 PM during Ramadan. They concluded that when fasting, the changes in food intake or sleep timings, affect the circadian rhythm and influence the onset time of acute coronary events (43).
It appears that in Ahvaz, the incidence of stroke-induced aphasia is affected by the time-calendar changes. The highest incidence of stroke-induced aphasia was observed in summer, on Saturdays from 8:00 AM to 4:00 PM with a peak incidence of 8:00 AM to noon. To diminish the incidence of stroke-induced aphasia, it is recommended to offer counseling for modification of the residents’ lifestyle in Ahvaz by mass media, scientific communities and therapeutic sanitary centers. It is obvious that by decreasing stroke incidence, stroke-induced aphasia would decrease. Since, the real mechanisms underlying the circadian variation of cardiovascular events are still uncertain, further studies are needed to better understand this issue in patients at risk, and this may help to develop future strategies of preventive therapies during high risk morning hours.