1. Introduction
Anomalous right ventricular muscle bundle (ARVMB) is a form of congenital subvalvular pulmonic obstruction (1). The muscle bundle can be single or multiple (1). This bundle can divide the right ventricle into two chambers and make double chamber right ventricle (DCRV) (2). The hypertrophied muscle band can make two chambers with a pressure gradient across (3). Transesophageal echocardiography (TEE) is a good diagnostic tool as it estimates resultant systolic pressure gradient within the ventricle (2). While DCRV causing right ventricular outflow obstruction is a rare finding in adults, it is usually diagnosed in childhood and is commonly associated with ventricular septal defect (VSD) (1). When ARVMB and VSD present simultaneously, it may be diagnosed as Tetralogy of Fallot or VSD with infundibular stenosis (1). Sometimes the space between anomalous muscles can be confused surgically with VSD (4). Moderator and anomalous muscle bundle is attached parietaly to the right ventricle anterior wall; however, the moderator band does not usually present as obstructive factor (4). Obstructive muscle should be resected in symptomatic adults as well as repairing any associated condition and symptomatic patients with gradient over than 40 mmHg should undergo surgery as well (5). In this report, we will discuss a case of anomalous muscle bundles causing subpulmonic stenosis and its surgical management.
2. Case Presentation
A 40-year-old man with a history of mild dyspnea on exertion since 10 years ago was referred to our cardiology clinic. His symptoms became worsen since last year. His physical examination revealed a loud murmur and referred to cardiologist for further work-up. On physical examination a grade IV/VII harsh systolic ejection murmur most prominent at the left lower sternal border, and a right ventricular heave were found. A 12 lead electrocardiogram showed normal sinus rhythm, right ventricular hypertrophy, and right axis deviation.
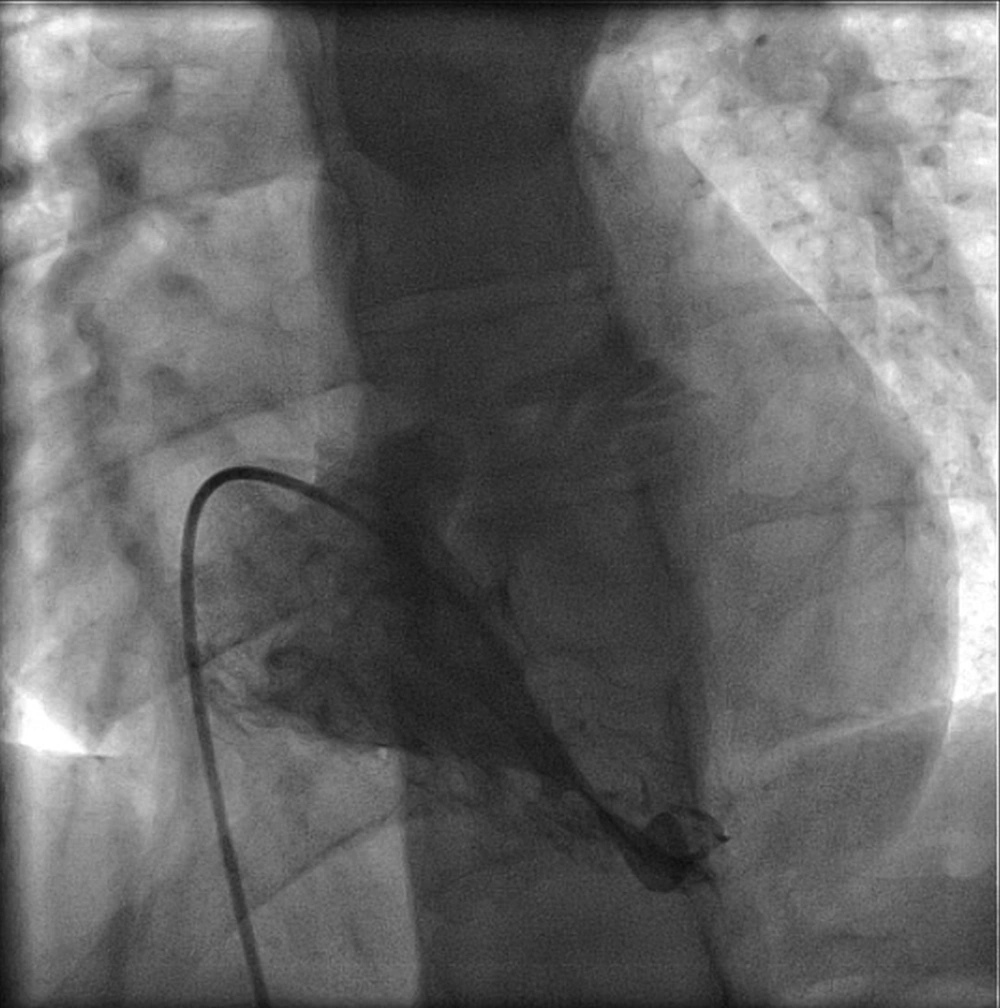
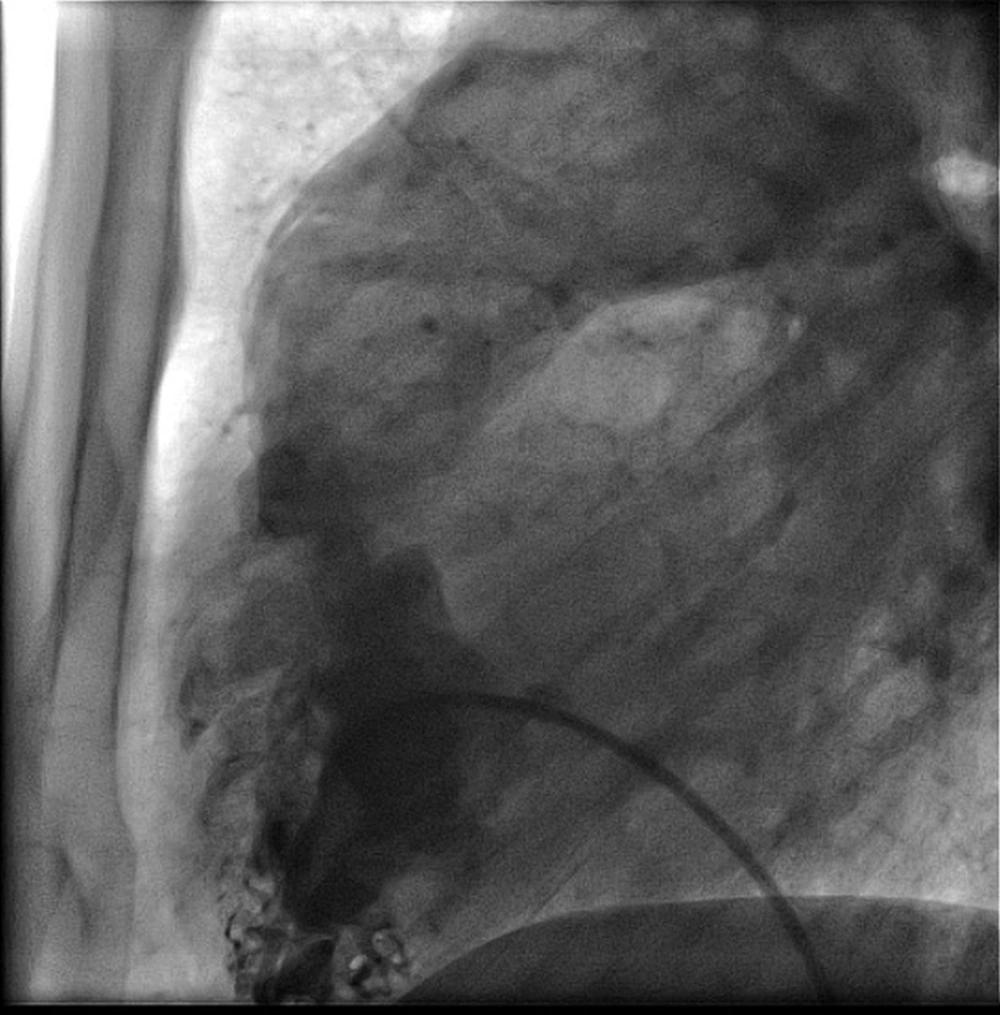
Transthoracic echocardiogram (TTE) showed normal left ventricular function and dimensions, a small perimembranous VSD with left-to-right shunt, moderate right ventricular hypertrophy (RVH), moderate right atrial enlargement (RAE), and mild tricuspid regurgitation (TR). The patient also underwent transesophageal echocardiography (TEE) that showed severe RAE, severe RVH, severe right ventricular outflow tract (RVOT) obstruction with excessive hypertrophy of the infundibulum, and right ventricular muscle bundles. There was a small restrictive perimembranous VSD measuring 3 mm and mild TR. There was also mild mitral valve and aortic valve regurgitation. A patent foramen ovale was also noted. Right cardiac catheterization demonstrated high right ventricular pressures of 100/25 mmHg compared to aortic pressure of 123/88 mmHg. On pullback across the RVOT, the pressure was 100 mmHg in the proximal chamber and 25 mmHg in the distal chamber with a 75 mmHg pressure gradient (Figures 1 and 2). There was no pressure gradient between the RVOT and the main pulmonary artery. The Qp:Qs ratio was 1.3. Right ventriculogram demonstrated RV subvalvular/infundibular stenosis secondary to RVH. Left cardiac catheterization was unremarkable.
The patient underwent repair of the subpulmonic stenosis. Substantial RV muscle bundle resection was done through a right atrial approach with closure of the VSD and patch augmentation of the RVOT. The patent foramen ovale (PFO) was also closed. There were no operative or postoperative complications. A postoperative TEE demonstrated moderate RAE, moderate RVH, no RVOT obstruction, no VSD, and normal biventricular systolic function.
3. Discussion
DCRV is a congenital heart defect which is seen in 0.5% - 2% of congenital heart disease cases (2). The anomalous muscle bundle divides the ventricle into a low pressure outlet and high pressure inlet portion (2). There are various etiologies reported for the obstructive form of this disease. Increased blood flow among VSD causing supraventricular hypertrophy, hypertrophy of superior displaced moderator band, and septoparietal trabeculations in combination with acquired factors are 3 causal bases (5). While DCRV is mostly presented between 4 months to 20 years of age, our case was a 40-year-old adult (2). DCRV can be asymptomatic or as our case, presented with exertional dyspnea as the most prevalent presentation (2). Other presenting symptoms include angina, dizziness, and even syncope (6). These patients might have normal chest x-ray or even normal electrocardiograph if there is no significant ventricular shunt or significant obstruction (1). TTE and TEE are two simple diagnostic techniques. TEE is more capable than TTE in defining the details of DCRV, including the pressure gradient (2). Cardiac computed tomography, magnetic resonance imaging, and catheterization may also be required for complete characterization of this congenital heart anomaly in adults (7). While VSD is a common coexisted lesion, pulmonary valve stenosis, subaortic stenosis, Tetralogy of Fallot, double outlet right ventricle, and complete or corrected transposition of great vessels are other coexisting lesions (5). In addition to a restrictive perimembranous VSD, the reported case had RAE, mild TR, severe RAE, severe RVH, severe RVOT obstruction with excessive hypertrophy of the infundibulum, and right ventricular muscle bundles. Khoueiry et al. reported a 45-year-old female with persistent dyspnea on exertion for 2 years (3). Her TTE showed small VSD and colour Doppler TEE showed turbulence with high velocity jet in proximal portion of right ventricle as well as an abnormal muscle bundle separating in right ventricle (3). In magnetic resonance imaging, they confirmed a VSD lesion without significant shunt and double chamber right ventricle (3). Park et al. reported a case of asymptomatic isolated DCRV in adulthood (8). A turbulent flow jet with mosaic pattern was present and moderate tricuspid regurgitation, right ventricular dilatation and hypertrophy were found (8). TEE revealed an anomalous muscle bundle dividing right ventricle to two chambers (8). They did not find any shunt between right and left parts of the heart and confirmed their diagnosis with MRI (8).
DCRV has good survival and low long-term morbidity (9). As the obstruction in DCRV is progressive and can lead to heart failure, surgical treatment should be generally considered (5). Anomalous muscle resection can be made through a right ventriculotomy, right atriotomy or combined transatrial-transpulmonary approach (5). Ventriculotomy is rarely used and might be necessary in patients with severe right ventricular obstruction (5, 10). Long-term prognosis of intracardiac repair of DCVR is excellent (10). In conclusion, muscular subpulmonic stenosis is a rare condition in adult patients. Full echocardiographic examination of the right ventricle, including RVOT is essential for the diagnosis. Invasive diagnostic studies and CMR can further define the anatomy and pressure gradients to confirm diagnosis and guide therapeutic decisions. Surgical correction appears to be a successful strategy for management of this rare condition in adults.