1. Background
Low back pain (LBP) is one of the most common and costly musculoskeletal pain syndromes in today's societies, which almost over 80% of the people are affected by this disease in industrial and nonindustrial countries (1, 2). Low back pain is the most common cause of activity limitation in people younger than 45 years and the fourth leading cause among 45-64 years old people (3). This phenomenon can disable the people from personal and social activities for 23 days a year (3). Previous studies attest to the high frequency of back pain in the society (3). In 1994, 52% of the nurses in the hospitals in Belgium complained of musculoskeletal disorders associated with their work which lasted more than 12 hours a day and the main cause of these disorders was LBP (4). Because of the detrimental effects of LBP on individuals' activities in the areas such as socioeconomic, work-related or psychological, therapeutic strategies have been emphasized on the prevention and reduction of LBP. Despite different viewpoints about LBP, there is an agreement among authorities that the mechanical stress in lumbar spine is created due to disordered forces in surrounding joints or abnormality in movement patterns in related joints.
Today, the majority of the researchers believe that changes in movement patterns in lumbar-pelvic muscles is one of the important mechanisms for development of the LBP (4, 5). Therefore, great importance has been recently attached to the assessment and treatment of movement patterns (5, 6). Balanced motor system is resulted from the coordinated activity of synergist and antagonist muscles.
According to this point of view, long-term faulty postures, poor movement habits and repetitive movements will change characteristics of muscle tissue (7). So that, in stabilizing muscular system, sufficient stability is not acquired for creating desired movement and it will lead to global muscular system imbalance. Eventually, this places the specific mechanical stress and strain on various structures of the body (7).
Several studies have demonstrated changes in patterns or strategies of lumbar-pelvic synergistic muscle recruitment and also changes in a lumbar-pelvic motion in patients with LBP during various tasks and limb movements (8-13). Recently, considerable interest has been placed on the coordinated activity between stabilizer and mobilizer synergistic muscles; likewise, the aim of the rehabilitation programs is the modification of altered movement patterns to prevent and reduce LBP in individuals (14-16).
Janda was one of the first clinical researchers that evaluated quality and control of the movement patterns and measured muscular activation patterns during various clinical tests in non-symptomatic and symptomatic subjects and provided the important information regarding chronic or recurrent musculoskeletal pain (4). According to Janda, the movement pattern analysis is more reliable than other factors such as pain when assessing functional pathology (4). Prone knee-flexion (PKF) is one of the clinical tests used as an assessment method and treatment for movement patterns, assessing the function of trunk muscles and coordination of muscles and determining muscle imbalance in lumbar-pelvic region (7, 17, 18).
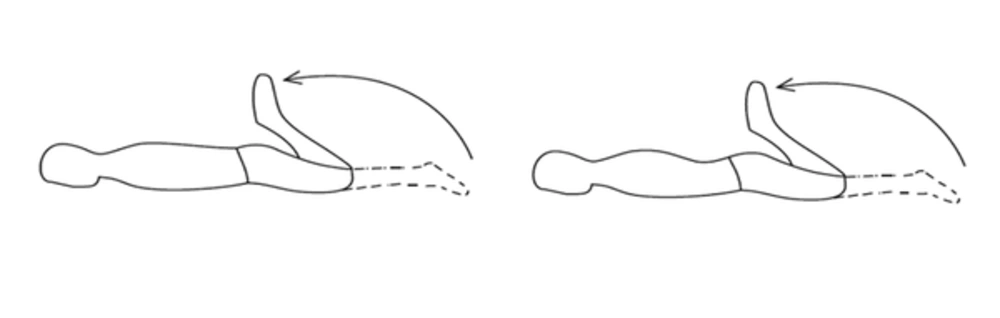
According to Figure 1 in a PKF test, at first the local stabilizing lumbar-pelvic muscle contraction provides sufficient stability in a lumbar-pelvic region and then prime-mover muscles in thigh and knee can create flexion in the knee. However, the stabilization action of muscles counteracts the effect of the prime-mover muscles on joints. However, when a mechanism of faulty joint-stabilization exists, rectus femoris is stiffer than the abdominals and the anterior supporting structures of the lumbar spine, resists knee flexion and produces compensatory motion, including an exaggerated anterior pelvic tilt with lumbar extension. This compensatory motion occurs long before the muscle reached the end of its range, which in turn may develop mechanical pain in lumbar-pelvic region (7, 17, 18).
The existing concern in this area is to see whether there is a considerable change in lumbar lordosis during the PKF test among healthy individuals to compare with LBP patients in the future. However, it remained unclear that even without any pain and discomfort, global muscular system dysfunctions including length-associated change related to muscle function, imbalance in recruitment between synergistic or antagonistic muscles or even direction dependent relative stiffness and flexibility can lead to considerable changes in lumbar lordosis during PKF test in healthy individuals.
2. Objectives
The aim of this study was to investigate the changes in lumbar lordosis during the PKF test in healthy subjects.
3. Patients and Methods
3.1. Patients
This quasi-experimental study with repeated measurements was used to measure the changes in lumbar lordosis during the PKF test in healthy subjects. Subjects were recruited from a convenience sample of students and staff at the University of Social Welfare and Rehabilitation Sciences [N = 40, average age: 23.57 (SD = 10.61) years old, average height: 162.0 (SD = 7.0) cm, average weight: 55.62 (SD = 6.55) kg, body mass index (BMI): 21.05 (SD = 2.26) kg/m²]. Exclusion criteria used to select the subjects for participation were as follows: under 20 years of age, over 50 years of age, pregnancy, those who participate in programs to prepare for competitive sports (exercise more than 3 days a week), history of hip injury or trauma, history of lumbar spine surgeries, history of LBP which had prevented the performance of normal activities for at least one day in the previous three months, history of anterior knee pain, history of neuromuscular disorders, leg-length differences of more than 1 cm, shortness of knee flexors, unable to perform active PKF without any pain. Subjects were informed of research stages and they signed a consent form. The study and consent form were approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences.
3.2. Measurement Techniques
A standard flexible ruler was used to measure the size of lumbar lordosis. Its length and width was 61 and 2 centimeters, respectively. According to previous studies, a flexible ruler for measuring the lumbar lordosis is known as an instrument with high validity and reliability (19-21) and its linear correlation with a radiographic criterion has been 0.92 (22).
3.3. Procedure
To measure lumbar lordosis, at first all subjects of the study, lied in prone position and vertebral spinous process T12 and S2 were identified and marked by removable red labels with 6 mm diameter. Then, a flexible ruler was placed on vertebral spinous processes to determine lumbar lordosis. The obtained curve from the flexible ruler was drawn without any changes on a piece of paper. The subjects were asked to bend their knees in the prone position. Then, the above test was repeated once more. The dominant leg was chosen for investigation so as not to feel any pain during knee flexion.
To determine the degree of lumbar lordosis, we drew a line to connect two points which is equivalent T12 and S2. Then we chose the middle of this line and drew another line vertically and we called these lines L and H, respectively. Hence, according to the formula θ = 4 [Arc tg (2H/L)], lumbar lordosis was calculated (7, 19). Finally, the difference between two measurements was recorded according to the changes in lumbar lordosis.
3.4. Data Analysis
Statistical analysis was performed using SPSS version 16.0 (SPSS Inc., Chicago, IL). Kolmogrove-Smirnove test showed that variables have a normal distribution. Paired t-test was used to demonstrate the changes in lumbar lordosis before and after the PKF test in healthy subjects. A P value of less than 0.05 was considered statistically significant.
4. Results
The demographic data of the individuals are displayed in Table 1.
The lumbar lordosis before and after the PKF test is presented in Table 2. Results demonstrated that there was a statistically significant difference in lumbar lordosis between prone position and after the PKF test in healthy subjects (P = 0.000).
5. Discussion
The current study examined the changes in lumbar lordosis during the PKF test in healthy subjects. Results demonstrated that there was a statistically significant difference in lumbar lordosis between prone position and after the PKF test in healthy subjects.
The PKF test is one of the clinical tests used as a tool for evaluation and treatment of movement patterns and determining muscle stiffness in thigh and knee regions in the most clinics (7, 17, 18). If synergistic muscles of the lumbar-pelvic region function in a proper sequence of recruitment, sufficient stability is created to prevent the increase in lumbar lordosis during knee flexion and it causes normal movement pattern in lumbar-pelvic region and thus in this case there should be approximately 120 degrees of knee flexion without significant lumbar-pelvic motion (7, 13). However, in normal movement pattern, local stabilizer muscles contract first then global stabilizer as synergist to increase the stability in times of an extreme need. Whereas characteristics of abnormal movement patterns of recruitment are that the activity of global stabilizer muscles will increase significantly to compensate the deep local muscles dysfunction and decreased spinal stability (9, 23).
Sahrmann (1992, 2002) proposed the concept of "relative flexibility" or "relative stiffness" that has been linked to uncontrolled movement and pain and pathology by causing direction-related stress and strain during various functional movements in the patients with LBP (7). She suggested that if the rectus femoris is stiffer than abdominals and the anterior supporting structures of the lumbar spine, then during knee flexion, compensatory exaggerated anterior pelvic tilt with lumbar extension motion is observed (7).
The current study was carried out on healthy individuals. Hence, an increase in lumbar lordosis during the PKF test can indicate the lack of sufficient stiffness in the abdominal and anterior supporting structures of the lumbar spine. However, in this study stiffness in thigh and anterior supporting structures of the lumbar spine was not measured. Poor postural alignment and poor movement habits can contribute to the global muscular system imbalance and abnormal movement patterns that a vicious cycle is created (7, 17).
Several studies have demonstrated that patients with chronic or recurrent pain use other strategies, which are different from common one's (24). In 2009, Scholtes et al. (24) found in their study that during the PKF and prone hip lateral rotation, people with LBP who played rotation-related sports demonstrated a greater maximal lumbar-pelvic rotation angle and earlier lumbar-pelvic rotation, compared to people without LBP, as the lumbar-pelvic region may move more frequently during the early ranges of lower limb movement in daily activities. The increased frequency of lumbar-pelvic motion may contribute to increase tissue stress in lumbar-pelvic region related to development or persistence of LBP; particularly if the lumbar-pelvic motion is in the same direction.
According to previous studies (23, 25-27), any changes in the activity of the deep stabilizer muscles of the abdomen and spine can be considered an important factor in lumbar-pelvic instability and altered movement pattern leading to developing back pain. In 2005, Cholewicki et al. (26) have considered delayed trunk muscle reflex response to sudden trunk loading appear to be a preexisting risk factor for LBP. In 1996, Hodges et al. (27) have demonstrated that delayed activity in local stabilizer muscles (e.g. transversus abdominis) that is created during limb movement, indicates a deficit of motor control and is hypothesized to result in inefficient muscular stabilization of the spine in patients with LBP.
Evidence has shown that the motor-control deficiency in local stability muscles (e.g. Transversus Abdominis (Tr) A) and chronic or recurrent pain syndromes in a lumbar-pelvic region have a mutual effect on each other and there is no strong evidence to indicate what is the cause and effect in patients with LBP (28). Hence, the local stability muscular system dysfunction appears to present only after developing pain and related pathology (17), whereas the current study was carried out on the sample of students and staff who had no proper life style and physical activity. Therefore, they were at risk of instability in the lumbar-pelvic region. It seems because of the inefficiency in stabilizing action of the muscles in lumbar-pelvic region and excessive flexibility of movement of the lumbar spine in the direction of extension, a compensatory lumbar extension motion was observed during the PKF in healthy subjects (7). However, there are more paths to pave to resolve the ambiguities available in this area.
Previous studies have demonstrated patterns of recruitment between one-joint (stabilizer) and multi-joint (mobilizer) synergists in non-symptomatic and symptomatic subjects during functional movements and various tasks (8-16). In this study, we did not measure the maximal amplitude of the electromyographic activity of the stabilizing and prime-mover muscles during the PKF to find the pattern of muscle recruitment. According to Sahrmann (7), the PKF test should be performed for patients with mechanical back pain , when the lumbar-pelvic region is stabilized manually or with other means (hollowing or bracing maneuver of abdominal), to minimize changes in lumbar lordosis and anterior pelvic tilt. Therefore, we can speculate that the amount of changes in lumbar lordosis during the PKF test is due to lumbar-pelvic instability and lack of sufficient stiffness in the abdominal and anterior supporting structure of lumbar spine in healthy subjects. Hence, to provide better stability and control in a lumbar-pelvic region, the appropriate therapeutic strategies (e.g. abdominal drawing-in maneuver (ADIM)) have been promoted as a preventive regimen (29). In the current study, It remained unclear whether these changes in lumbar lordosis during the PKF test in patients with LBP are greater than those of healthy individuals or not. This must be interpreted with caution as the current study did not involve a direct comparison with LBP patients. Further studies are needed to compare the changes in lumbar lordosis in the PKF test in subjects with and without LBP. Also, it is suggested that in future studies, the pattern of lumbar-pelvic synergistic muscle recruitment during the PKF test will be measured to determine whether the motor-control deficiency in deep local stability muscles exist or not in the LBP patients and even healthy individuals who are at risk of lumbar-pelvic instability and developing back pain in the future. Just like any other researches, the current study inevitably has limitations; one of these limitations was sample size.
One point should be considered with regard to generalizing of the present results is the sample population. In this study, only healthy subjects from University of Social Welfare and Rehabilitation Sciences were recruited and other healthy subjects were not included. Therefore, the results of this study may be more applicable to individuals from University of Social Welfare and Rehabilitation Sciences who constituted the participants and could not be extrapolated to others.
It is suggested that future researches have been focused on stabilizing exercises with emphasis on contraction of deep local stabilizing abdominal and spinal muscles (e.g. Tr. A or multifidus) and also stabilizing maneuvers of abdominal muscles (hollowing maneuver and bracing maneuver) in patients with and without LBP.
The results of this study demonstrate that the increase in lumbar lordosis during the PKF test in healthy individuals is due to lumbar-pelvic instability and lack of sufficient stiffness in the abdominal and anterior supporting structure of lumbar spine. This information is important for investigators using the PKF test as an evaluation tool of lumbar-pelvic movement patterns in the individuals with LBP and even healthy individuals who are at risk of instability in a lumbar-pelvic region and developing back pain in future.