1. Background
TURP is the best surgical technique for treatment of clinically obstructive BPH (benign prostatic hyperplasia); it’s successful rate is about 85% - 90% (1). Regardless of this high competence, blood loss, contracture of bladder neck, trans urethral resection syndrome, urine incontinence, and retrograde ejaculation are the backwash of this surgical technique (2). Nowadays, a monopolar electrocautery machine, contemporary, is used for TURP. In this system, the electricity runs through the person’s body, from a positive electrode that is put on the resectoscope, towards the return sheet that is outed on the person’s leg. However, several maleffects such as warming of deeper tissue and provocation of nerves and muscles may happen (3). In bipolar system, for the reason of putting the positive and negative electrode on the same axis of resectoscope and applying high local electrical current, accompanied with less negative effects at distance axis (4).
The essential factor for TUR syndrome is excess absorption of hypotonic fluids (such as distilled water or glycine) that are used for irrigation during surgery. In recent years, with the purpose of reducing the complications of TURP, bipolar electrosurgical technologies have been applied. In this technique, normal saline is used for irrigation (5-7). There isn’t a solidarity regarding the effect of bipolar technique on pre and postoperative complications compared with usual monopolar technique. On the other hand, the impact of TURP, especially monopolar, on erectile function is disputable. Many studies investigated the influence of TURP (monopolar or bipolar) on erectile function (8). This is a prospective randomized study where it’s purpose is to compare the safety and efficacy of TURP in bipolar and monopolar methods within six months follow-up by attention to IPSS (international prostate symptom scale), IIEF-5 (international index of erectile function-5) score, catheterization time, rate of urethral stricture after surgery, and rate of reoperation.
2. Methods
2.1. Trial Design and Population
This randomized controlled study was a single-blinded study and was carried out among 94 patients who suffered from LUTS (lower urinary tract symptom) related to BPH. All patients were referred to the Golestan Hospital, Ahvaz, Iran, from January 2016 to April 2016. The Golestan Hospital is a governmental hospital, which is govern by Ahvaz Jundishapur University of Medical Sciences and has a urology department. We assessed the eligibility of 107 patients who referred to the hospital upon admission to the urology ward based on the following criteria:
We included patients with BPH (benign prostatic hyperplasia) without any previous procedures on prostate or urethra and patients with BPH without any history of urethral stricture and our exclusion criteria were existence of bladder stone, large bladder diverticula, and prostate cancer in the final pathology.
2.2. Interventions
All cases underwent bipolar or monopolar TURP, randomly (47 cases in each group). After obtaining a medical history from all cases, they were assessed preoperatively by use of IPSS, digital rectal exam, PSA, urine analysis and culture, function of kidney, and serum electrolytes. Furthermore, prostate size was measured by use of trans rectal ultrasonography and the sexual function was assessed by IIEF-5 questionnaire. All the patients with symptomatic BPH, who required surgery due to urine retention or previous failed medical treatment, were included in this study. The individuals with preceding urethral or prostatic manipulation, neurogenic bladder dysfunction, bladder stones, disorders of coagulation, and prostate malignancy were disallowed. A surgeon who was an expert in monopolar and bipolar TURP accomplished all of the procedures.
A Wolf generator (made in Germany) and an Olympus Lympus generator (made in Japan) were used for TURP in monopolar and bipolar technique, respectively. All procedures were done under spinal anaesthesia. Irrigation fluid for monopolar TURP was distilled water and for bipolar TURP was isotonic saline. A three way 24-F catheter was implanted at the end of operation. Irrigation with saline was continued until they were bleeding. In all cases, immediately after surgery serum electrolytes and haemoglobin levels were measured. Catheterization and hospitalization time, blood transfusion rate, and TUR syndrome, if happened, were charted after surgery. In addition, by use of IPSS (international prostate symptom scale) and IIEF-5 questionnaires, all patients were re-assessed at three and six months after their procedure and during this period, the necessity for reoperation and rate of urethral stricture happening were recorded.
2.3. Randomization and Blinding
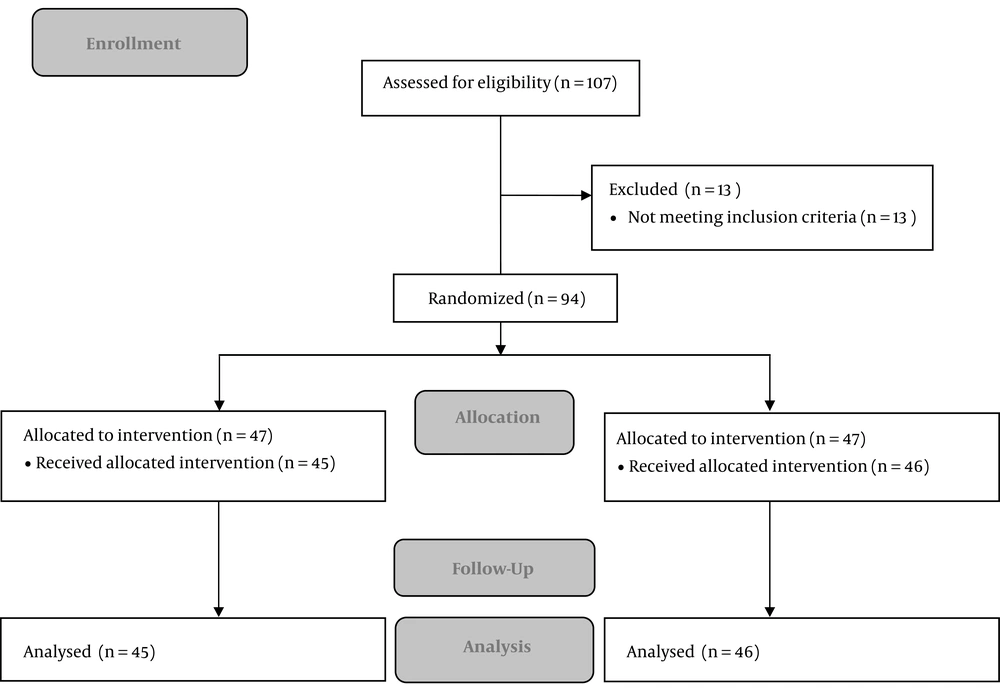
Participants were randomly allocated into two groups by using a computer-based randomization program (n = 47 in each group), which is illustrated in Figure 1. This was a single-blind study, in which participants were blinded, however, blinding of investigators could not be undertaken due to the nature of the interventions.
2.4. Outcomes
The primary outcomes were urethral stricture and reoperation rate after surgery, which were assessed during six months follow-up. As secondary outcomes, we measured IPSS and IIEF-5 scores (baseline, three and six months after surgery), catheterization time, hospital stay, change in serum Na level, and rate of Hb loss.
2.5. Sample Size
The sample size was determined according to a similar previous study (9). The sample size, by considering attrition, was calculated as 47 in each group (Power: 80% and α: 5%).
2.6. Ethical Considerations
Informed written consents were obtained from all cases and this study was approved by the Ethical Committee of Ahvaz Jundishapur University of Medical Sciences in 2017 (Ref No. IR.AJUMS.REC.1396.181). The research manner obeyed the ethical clues of the 2008 Declaration of Helsinki, which has been registered at the Iranian Registry of Clinical Trials. The study received clinical trial code IRCT2017060234301N1 available at: www.irct.ir.
2.7. Statistical Analysis
By use of SPSS version 22 for Windows, the statistical assay of recorded data was done. Parametric Student’s t-tests was used for analysis performation and assessment of numerical changings with diagonal diversion were performed by use of Mann-Whitney U-tests.
3. Results
In the monopolar classification, 45 (96%) of 47 cases were followed for at least 6 months, and in the bipolar classification, 46 (98%) of 47 cases were followed for the same time. The patients who stopped following were similar in both classifications, numerically. The mean of prostate size, PSA, age, IPSS score, IIEF-5 scores, serum sodium levels, and haemoglobin concentration were alike in two groups, preoperatively (Table 1). Duration of hospitalization, catheterization time, and the IPSS and IIEF-5 scores, which were measured in three and six months beyond the surgery, are represented in Table 2.
| Preoperative Variables | Monopolar Group, N = 45 | Bipolar Group, N = 46 | P Value |
|---|---|---|---|
| Age, y | 67.5 (8.2) | 68.8 (8.8) | 0.48 |
| IPSS score | 22.50 (2.27) | 22.66 (3.07) | 0.77 |
| IIEF-5 score | 16.59 (5.8) | 15.22 (6.0) | 0.27 |
| PSA, ng/mL | 2.2 (0.8) | 2.1 (0.7) | 0.45 |
| Hb, mg/dL | 12.84 (0.98) | 12.8 (1.2) | 0.96 |
| Na, mg/dL | 140.2 (2.04) | 139.7 (1.52) | 0.20 |
| Prostate volume, gr | 52.6 (11.9) | 54.3 (11.1) | 0.48 |
Preoperative Demographic Characteristicsa
| Post Operative Variables | Monopolar Group, N = 45 | Bipolar Group, N = 46 | P Value |
|---|---|---|---|
| Na, mg/dL | 136.3 (2.05) | 138.2 (1.6) | < 0.001 |
| Hb, mg/dL | 11.31 (1.07) | 11.68 (1.19) | 0.131 |
| IPSS, 3 months after surgery | 8.26 (3.25) | 6.98 (3.8) | 0.088 |
| IPSS, 6 months after surgery | 6.56 (3.06) | 5.9 (3.6) | 0.337 |
| IIEF-5 score, 3 months after surgery | 18.8 (3.8) | 17.42 (5.42) | 0.163 |
| IIEF-5 score, 6 months after surgery | 19.8 (4.25) | 17.95 (5.7) | 0.084 |
| Catheterization time, day | 5.5 (1.4) | 1.9 (1.4) | < 0.001 |
| Hospital stay, day | 2.5 (0.6) | 1.5 (0.5) | < 0.001 |
Post Operative Demographic Characteristicsa
The necessity of blood transfusions was 13% (six patients) in monopolars and 4% (two patients) in bipolars. TUR syndrome didn’t happen in any cases of each group. Catheterization time was longer in monopolar patients. Length of hospitalization was clearly different among the groups and improvement of IPSS scores was comparable in 2 groups. Along six months follow-up, reoperation was required in one patient (2%) in the monopolar cases. In two (4%) cases of bipolar group and one (2%) cases of monopolar group, the urethra stricture happened.
Although, during the six months follow up, the IIEF-5 scores were slightly better in both groups, in comparison to the IIEF-5 scores of all cases, erectile dysfunction became better in 26 (28.6%), worsened in 16 (17.6%), and without any changes in 49 (53.8%). The changes were similar between the groups.
4. Discussion
Bipolar TURP is an impressive and secure technique that is correlated with a distinctly shorter catheterization time, shorter hospital stay, less decrement in the levels of serum sodium and is correspond with monopolar TURP regarding efficacy by attention to IPSS IIEF-5 scores.
The monopolar TURP is used for treatment of LUTS related to BPH, conventionally. However, this technique contains many perioperative and postoperative complications. In contrast with monopolar TURP, where hypotonic solution, such as distilled water or glycine, are used for irrigation; in bipolar TURP, an isotonic solution is used. This isotonic irrigating fluid is believed to protect against the TUR syndrome, which is the hazardous complication of TURP.
Coagulation of bleeders is better done by bipolar technology (10). In TURP, by bipolar technology, the surgeon has a clearer field (4). There are many studies that reported greater amount of blood loss during monopolar TURP in contrast with bipolar TURP (10).
In our study there was greater decrement in haemoglobin concentration in monopolar cases compared with bipolar cases, however, the difference was not significant. In the immediate post-surgical period, the necessity for blood transfusion was seen in six (13%) and two (4%) cases in the monopolar and bipolar groups, respectively. HB loss in bipolar TURP was less than the monopolar TURP due to cauterization of the small bleeding vessels, therefore, bladder irrigation was less demanded post surgically and duration of hospitalization and catheterization time were clearly shorter in the bipolar group in our study. Decrease in the mean concentration of hemoglobin in the monopolar group was greater than that of the bipolar group, however, the difference was not significant. During the early postoperative period, blood transfusion was required in two (4%) and six (13%) patients in the bipolar and monopolar groups, respectively.
Mean catheterization and hospitalization time and transfusion rate in the Borboroglu study were 1.4 and 1.1 days and 0.4%, respectively (11).
TUR syndrome is the worst complication of TURP, which is a result of increasing in the load of fluid absorption along the continued surgery (12). Chen et al. reported that the mean decrease in plasma sodium levels was 10.7 and 3.2 mmol/L in monopolar and bipolar cases, respectively (8). In our study, the mean decrease in sodium concentrations in monopolar cases was significantly less than bipolar cases, however, TUR syndrome didn’t happen in any cases of the groups.
Our results confirmed that the reduction in IPSS score is developed in both groups. IPSS score improvement is resulted from removal of obstruction (12).
The rate of urethral stricture after bipolar and monopolar techniques is discussable. Some studies reported similar rates of urethral strictures between two techniques (8, 13), whereas other reports show a higher rate of this complication after bipolar TURP (9).
In our study, the rate of urethral stricture was not clearly different in two groups as like as the result of Mamoulakis et al. study (14). A significant correlation between erectile dysfunction and the LUTS was found in many recent studies (11, 15). There are still disagreements regarding the influence of TURP on the erectile function (12).
In our study, during the six months follow up, a decline in erectile function happened in 17.6% of cases and erectile dysfunction progressed in 18.5% of cases, which had normal erections before surgery; 82.4% of cases became better or unaffected. There wasn’t any correlation between diabetes mellitus, age, and erectile function. During the follow up, the alterations in IIEF-5 scores were similar between groups.
4.1. Future Studies
Longer follow-up studies are warranted to establish the long-term effects of bipolar TURP versus monopolar TURP.
4.2. Conclusion
Bipolar TURP is an impressive and secure technique that is correlated with a distinctly shorter catheterization time, shorter hospital stay, less decrement in the levels of serum sodium and is correspondent with monopolar TURP about efficacy by attention to IPSS IIEF-5 scores. In contrast with monopoar TURP, it showed similar improvement in urinary symptoms along six months of follow up.