1. Background
The prevalence of intestinal parasites is relatively high around the world, particularly in developing countries. According to WHO, three billion individuals are infected; out of which, around 450 million are contaminated as a consequence of these diseases. These diseases remain a medical issue. Regardless of endeavors by the WHO, governments try to eliminate the parasites and treat parasitic illnesses (1, 2). Parasitic contamination might be asymptomatic or reach out to horribleness and mortality, contingent upon the nourishment and wellbeing status of influenced people (3, 4). They happen in both rural and urban population, particularly in school-age kids because of their propensity for playing or taking care of tainted soils, eating with dirty hands, unhygienic latrine practices, and ingestion of spoiled sustenance, water or soils (5, 6).
These contaminations can cause press inadequacy, impediment of development, vitality lack of healthy sustenance, and low instruction execution of school youngsters (7).
If the infected individuals with intestinal parasites treated not completely, they can be a transporter of the enteric parasites to healthy people (8). For enhancing hygiene conditions about parasitic diseases, in sustenance parts, as acclaimed by National Food Safety Standards in Iran, all nourishment handlers must be checked for intestinal parasitic contaminations preceding accepting their wellbeing endorsement (9).
In Iran, nourishing, wellbeing, and social states of the general population have caused a few sections of our national progress toward becoming a noteworthy focal point of intestinal parasitic disease in the world. On the other hand, control of parasitic contaminations encounters with obstacles because of natural, monetary, and social conditions (10). Therefore, the existence rates of protozoan contaminations are very high in a few of developing countries, such as Iran (11). Various studies have been done on the prevalence rate of parasites in different areas of the country demonstrating that the existence of intestinal parasitic diseases is about 1.5 to 60.9% (12). Earlier examinations revealed Giardia intestinalis and Entamoeba coli as the most widely detected intestinal parasites in Iran (13).
2. Objectives
This study aimed to investigate the prevalence of intestinal infections among referred individuals to the Central Laboratory of Borujen, Iran.
3. Methods
In this cross-sectional study, 5156 stool samples were randomly collected from referred individuals to the Central Laboratory of Borujen, Iran from 2016 to 2017. The study protocol was reviewed and approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
The objective of the study was explained to the participants to get written informed consent. Therefore, all participants filled informed consent prior to giving stool samples. The special bags were distributed to the individuals, with an information sheet explaining the procedure of sample collection, questionnaire, along with a stool specimen container with toilet tissue paper. Data were obtained by the questionnaire prepared on the basis of age, gender, sampling season, and positive or negative samples.
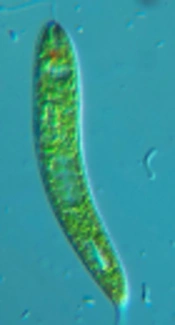
The samples underwent microscopic examination by wet mount preparation of the fecal samples using 100× and 400× of microscopic magnification. Lugol’s iodine dye was used for staining of wet mount slides (10).
Some people refused to give samples in the lab and provided the samples at home and brought to the lab.
The collected data were analyzed using SPSS software (version 20, Chicago, IL, USA). The prevalence of intestinal parasites evaluated with descriptive statistics, while the relationship between the variables and presence of intestinal parasites assessed by the chi-square test. The level of significance was 0.05.
4. Results
Out of 5156 examined stool specimens, 2611 (50.6%) were male and 2545 (49.4%) were female. Out of total samples, 78 cases (1.5%) were positive. Among positive cases, 42 (53.8%) were male and 36 (46.2%) were female, thus there was no significant correlation between the prevalence of infection and sex (P = 0.57).
Of the total number of 78 positive cases, 76 cases (97.4%) infected with the protozoan parasites and 2 cases (2.6%) with the helminthic infection. The highest prevalence of protozoa was related to Giardia, 75 cases (96.1%), Blastocystis, 1 (1.3%), and the highest helminthic infection was related to Enterobius vermicularis with 2 cases (2.6%) of the total number of positive cases.
The most positive cases were related to summer and the least positive cases were related to winter season (Table 1).
| Season | Stool Sample | Total | |
|---|---|---|---|
| Positive | Negative | ||
| Spring | 10 (1.4) | 701 (98.6) | 711 (100) |
| Summer | 43 (3.7) | 1119 (96.3) | 1162 (100) |
| Autumn | 16 (1.2) | 1358 (98.8) | 1374 (100) |
| Winter | 9 (0.5) | 1900 (99.5) | 1909 (100) |
| Total | 78 (1.5) | 5078 (98.5) | 5156 (100) |
aValues are expressed as No. (%).
In all seasons, the most common parasitic contamination was related to Giardia and there is a significant relationship between the frequency of parasites and the season (P < 0.001) (Table 2).
| Parasite Type | Season | Total | |||
|---|---|---|---|---|---|
| Spring | Summer | Autumn | Winter | ||
| Giardia | 10 (100) | 43 (100) | 15 (93.75) | 7 (77.8) | 75 (96.1) |
| Blastocystis | 0 (0) | 0 (0) | 0 (0) | 1 (22.2) | 1 (1.3) |
| Enterobius vermicularis | 0 (0) | 0 (0) | 1 (6.25) | 1 (22.2) | 2 (2.6) |
| Total | 10 (100) | 43 (100) | 16 (100) | 9 (100) | 78 (100) |
aValues are expressed as No. (%).
Among the positive cases, the highest frequency of parasitic infections was related to the age range of 0 - 10 years (48 cases), 21 to 30 years (12 cases), 11 to 20 years (8 cases), and in the age group of over 70 years significantly reduced the frequency of parasites. There was a significant relationship between parasitic infection and age (P < 0.001) (Table 3).
| Age Group, y | Stool Sample | Total | |
|---|---|---|---|
| Positive | Negative | ||
| 0 - 10 | 48 (3) | 1564 (97) | 1612 (100) |
| 11 - 20 | 8 (1.3) | 591 (98.7) | 599 (100) |
| 21 - 30 | 12 (1) | 1240 (99) | 1252 (100) |
| 31 - 40 | 4 (0.9) | 420 (99.1) | 424 (100) |
| 41 - 50 | 3 (0.9) | 341 (99.1) | 344 (100) |
| 51 - 60 | 2 (0.6) | 330 (99.4) | 332 (100) |
| 61 - 70 | 1 (0.3) | 292 (97.7) | 293 (100) |
| 71 - 80 | 0 (0) | 178 (100) | 178 (100) |
| 81 - 90 | 0 (0) | 93 (100) | 93 (100) |
| 91 - 100 | 0 (0) | 29 (100) | 29 (100) |
| Total | 78 (1.5) | 5078 (98.5) | 5156 (100) |
aValues are expressed as No. (%).
The frequency of sample distribution based on the year was shown in Table 4 (P = 0.115).
| Year | Stool Sample | Total | |
|---|---|---|---|
| Positive | Negative | ||
| 2016 | 15 (1.1) | 1383 (98.9) | 1398 (100) |
| 2017 | 63 (1.7) | 3695 (98.3) | 3758 (100) |
| Total | 78 (1.5) | 5078 (98.5) | 5156 (100) |
aValues are expressed as No. (%).
5. Discussion
In this study, among positive cases, 53.8% were male and 46.2% were female, thus there was no significant correlation between the prevalence of infection and sex. The highest prevalence of protozoa was related to Giardia, 96.1%, Blastocystis, 1.3%, and the highest helminthic infection was related to Enterobius vermicularis with 2.6% of the total number of the positive cases. Also, in all seasons, the most common parasitic contamination was related to Giardia and there is a significant relationship between the frequency of parasites and the season. Finally, there was a significant relationship between parasitic infection and age.
An examination explored the existence of intestinal parasites in sustenance handlers of Bandar Abbas, Iran. 34.9% of the members were sure for stool parasites. The most contaminated people were found in the laborers of bread kitchens almost 55% (P < 0.05). The intestinal parasites were Blastocystis hominis 25%, Entamoeba coli 8%, and Giardia lamblia 6.8% (14).
Another study by Hemmati et al. showed that the prevalence of both pathogenic and non-pathogenic intestinal parasites was high in inhabitants of Roudehen, Iran. Also, the prevalence of Giardia contamination was 1.2%. Blastocystis was the most widely observed intestinal parasite (15).
Next study aimed to survey the prevalence of intestinal protozoa diseases and related risk factors among schoolchildren in Sanandaj, Iran. This examination found that the general prevalence of intestinal protozoa disease was almost 43%; no instance of helminths contamination was recognized. Five major intestinal protozoa were B. hominis, E. coli, E. nana, G. lamblia, and I. buetschlii, respectively (16).
Another study was performed in Tonekabon, Iran. A total of 55% and 46% were male and female, respectively. Moreover, almost 61% and 40% of members had lived in the urban and rural regions, individually. in their study, 222 members (27.1%) infected with more than one intestinal parasites. Prevalence of pathogenic protozoa (Giardia lamblia and Cryptosporidium spp.) and helminths parasites was reported as 3.1 and 1.2%, respectively. The most widely detected intestinal parasites here were: Blastocystis and Endolymax nana. Also Giardia lamblia prevalence was 3% (10).
A study was also done in Jiroft, Kerman province, Iran. By and large, 28% of the cases were contaminated with intestinal parasites. The prevalence of protozoa and helminthic diseases were 27.4% and 1.8%, respectively. The most prevalent protozoan parasites were related to B. hominis and G. lamblia (17).
Another investigation in Boyer Ahmad district, Southwestern Iran showed that the prevalence of both pathogenic and non-pathogenic intestinal parasites in the population was 37.5% (385 out of 1025 cases), some individual with multiple infections. Giardia lamblia was detected in 179 (17.46%), Blastocystis hominis in 182 (17.76%), Entamoeba histolytica/dispar in 9 (0.87%), Endolimax nana in 216 (21.07%), Entamoeba coli in 151 (14.73%), Ioedamoeba butschlii in 45 (4.39%), Chillomastix mesnili in 22 (2.14%), Trichomonas hominis in 2 (0.19%), and Dientamoeba fragillis in 2 (0.19%) of cases (18).
Finally, in Isfahan this subject was investigated and intestinal parasitic infections were observed in 68 (10.42%) out of 652 studied humans. Forty eight Blastocystis hominis (7.36%), thirteen Endolimax nana (1.99%), nine Giardia lamblia (1.38%), five Entamoeba coli (0.76%), four Chilomastix mesnili (0.61%), and two Iodamoeba butschlii (0.15%) were observed in the studied people (19).
5.1. Conclusions
Based on the results of the present study, in all seasons, the most common parasitic contamination was related to Giardia and there is a significant relationship between the frequency of parasites and the season. Therefore, it should be considered the public health in all seasons, especially Giardia lamblia.