Dear Editor,
Due to the increasing number of cesareans, cesarean scar pregnancies are also increasing.
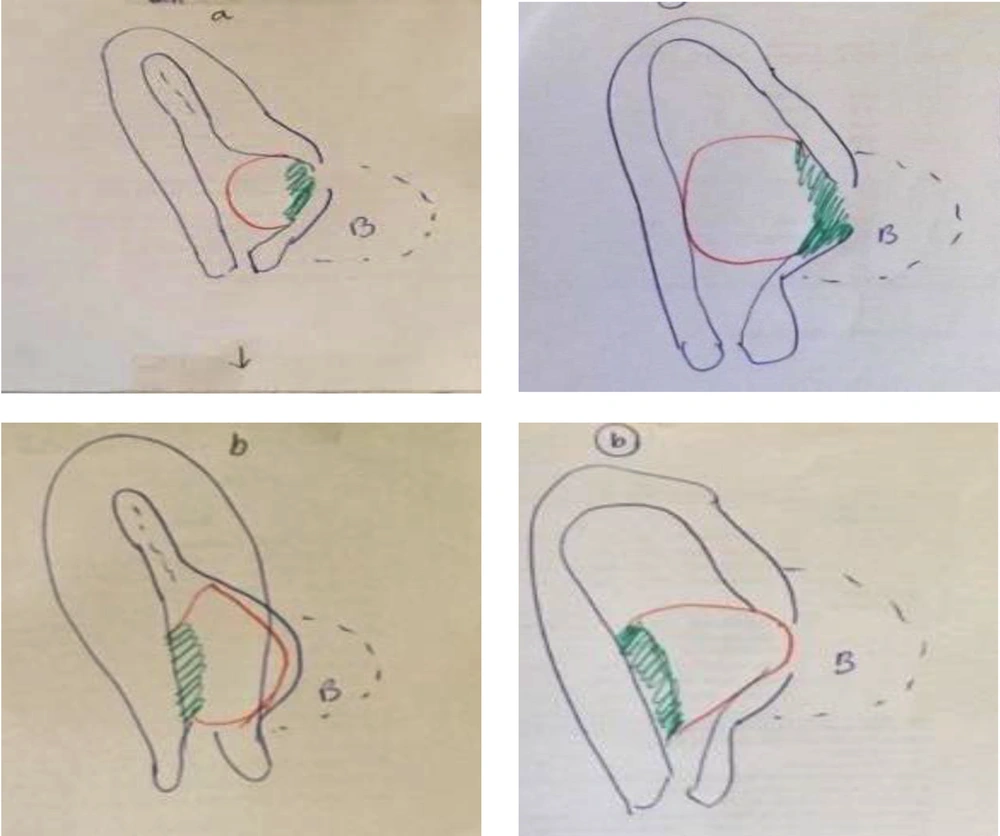
It is not intended to reemphasize the importance of diagnosis of this life threatening event since it is well known. In the literature, practical diagnosis of cesarean scar pregnancy is based on the history of cesarean delivery, a positive pregnancy test result, and the following sonographic criteria: (1) Empty uterine cavity, and closed and empty endocervical canal, (2) chorionic/gestational sac and/or placenta located in low and anterior walls of the uterus, below the bladder, in close proximity, and at the level of the internal os of the site of a previous hysterotomy scar (niche), with or without fetal or embryonic pole and/or yolk sac, with or without heart beats (depending on gestational age), (3) absence or thin myometrial layer between the chorionic/gestational sac and unusually close proximity to the bladder wall, and (4) abundant blood flow around the chorionic/gestational sac concentrated on the anterior side of the chorionic sac. The typical sonographic appearance of an arteriovenous malformation (AVM) is rarely observed (1). There were some cases of cesarean scar pregnancy in which placenta was low, but not necessarily located in the anterior wall of uterus. Placenta in some cesarean scar pregnancies is dominantly located in lateral wall or even posterior wall of uterus. But lateral parts of placenta extended to lateral sides of previous scar and invaded from lateral side of scar to outside of uterus. Therefore, if low-lying placenta/pregnancy is considered fewer cases of cesarean scar pregnancy are missed.
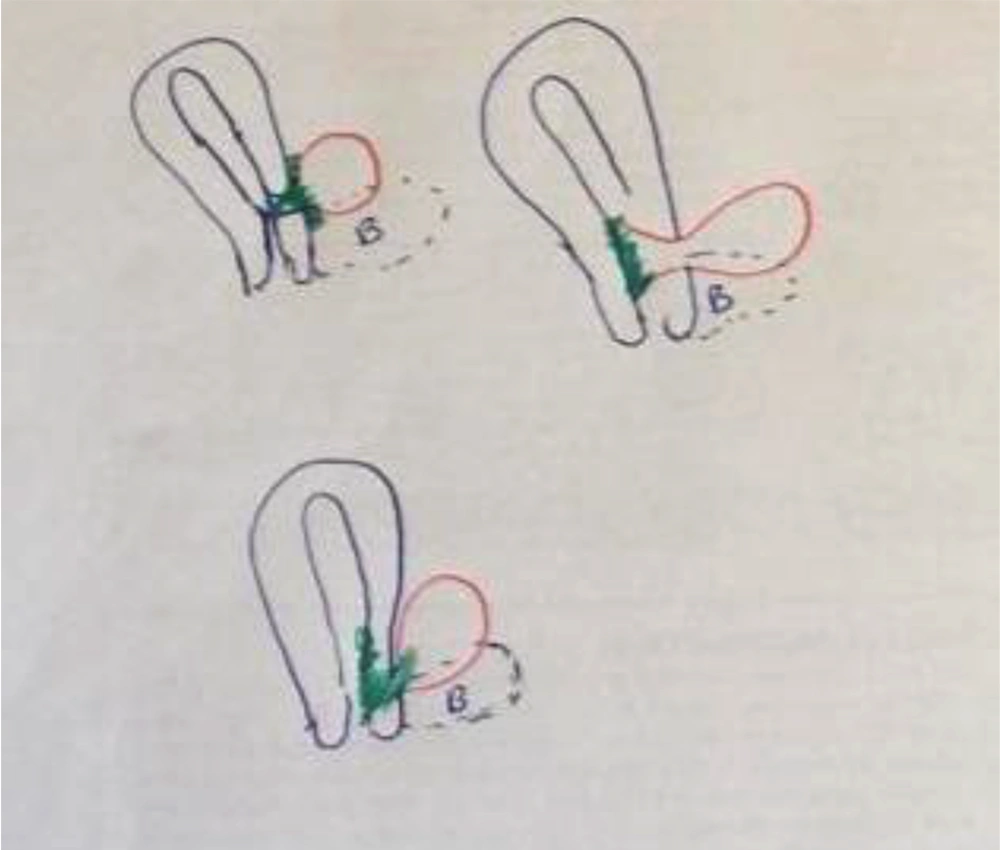
Based on gestational age, and size of fetus and placenta, there are different types of scar pregnancy: Site of placenta, site of the whole pregnancy (sac and fetus), and appearance of endometrium in upper part of uterus in early weeks of pregnancy.
In some cases it seems that with growing placenta and fetus, intrauterine pregnancy and later morbidly adherent placenta occur.
Different types of scar pregnancy
For a practical approach, scar pregnancy is divided into two groups:
A: Death scar pregnancy
B: Live scar pregnancy
Based upon authors' opinion, in group A, nature by itself passed more than half of the way of treatment. Decision between medical or surgical management depends on the site of scar pregnancy. In case of an extrauterine placenta and extrauterine pregnancy, curettage and intrauterine procedures are not enough and maybe dangerous.
In group B, decision about the kind of management is a per-case decision. In live extrauterine and line embedded scar pregnancy, both nonsurgical and/or surgical approaches are suggested. Management and decision in live intrauterine scar pregnancy is very obscure. It is not predictable which pregnancy reaches more than 24 weeks of gestation.