1. Background
Increasing the health of mothers and children was one of the 10 major achievements in public health in the United States from 1900 to 1999 (1). In the United Kingdom and the United States, it is recommended that fetal Doppler should not be used as a screening tool for placental failure unless the fetus is known as small for gestational age (SGA) (2-4). Late placenta failure may occur in fetuses that are appropriate for gestational age (AGA). However, findings from hemodynamic changes in these fetuses indicate that the fetus suffers from fetal growth restriction (FGR); however, their weight remains higher than 10%. As a result, a small portion of the AGA fetuses in each percentile weight is at risk for stillbirth. Nevertheless, the prenatal diagnosis of IUGR by clinical examination is less than the optimal condition. Babies with birth weights less than 10 percentiles of weight for the gestational are called IUGR (5). Doppler ultrasonography is used to investigate the incidence of uterine growth retardation, fetal distress, asphyxia, anemia, pregnancy, twin to twin transfusion syndrome. Uterine placental blood flow is detectable by Doppler ultrasonography, as a non- invasive method (6, 7). This sonography is very important in high-risk pregnancies. Ultrasound Doppler sonography completes the gray scale ultrasound. The blood vessels, blood flow, obstruction, and stenosis of the vessels, blood flow to organs, and also the dynamics of blood flow in organs can be evaluated for the diagnosis of physiological disorders by it. The aim of this study was to determine the relationship between the cerebroplacental ratio (CPR) in fetuses with normal weight percentile at 28 - 38 weeks of gestational age. So far, no study has been conducted to evaluate the statistical significance of uterine artery Doppler parameters in high-risk pregnancies, and most studies have studied some of the Doppler indices alone, such as PI (Pulsatility Index) or RI (Resistive Index) or early diastolic notching (8-11). One of the parameters for the evaluation of the middle cerebral artery is the following: Peak systolic velocity (PSV) (S), end-diastolic velocity (EDV) (D), and meantime span, systolic/diastolic ratio (S/D) RI, PI and comparison of arterial status of arteries (12, 13). CPR is an appropriate ratio as an important indicator for predicting adverse outcomes during pregnancy, and this includes implications for the proper evaluation of the SGA and AGA fetuses. CPR is obtained by dividing the Doppler index from the middle cerebral artery (MCA) into the umbilical cord vessels. When these changes occur, diastolic flow increases from the MCA with S/D, RI, and PI (14-17). However, when calculating the CPR, it is chosen more often than the recently calculated PI (18, 19). Abnormal CPR may lead to three types of Doppler measurement patterns, including first, when UA PI and MCA PI are in the upper and lower distribution curve, respectively. Second, when UA PI is normal, but the MCA PI is reduced and the third, the UA PI is abnormally high and the MCA PI abnormally decreases and is therefore abnormal in all three CPR patterns (20-24).
2. Methods
This descriptive-analytic study was conducted in Ahvaz from January 2016 until January 2017. This research was approved by the department of obstetrics and gynecology of the Jundishapur, Ahvaz University of Medical Sciences and Ahvaz University Research Committee and Imam Khomeini Hospital. The sample consisted of 230 pregnant women referred to the Prenatal and Emergency Health Clinic of Imam Khomeini Hospital. CPR was evaluated in the pregnant women at 28 to 38 weeks of gestational age, except for women with multiple pregnancies and women who had severe SGA fetuses. The relationship between CPR and some maternal-fetal factors such as diabetes, gestational hypertension, body mass index (BMI), PAPP-A, and drug use were investigated. The ultrasound device was V10, V20 Medison. Data were put in Astraia software of obstetrics. All measurements were done in the prenatal clinic.
2.1. Ethical Considerations
The verbal consent for performing the research was obtained through the direct reference of professional assistant of Obstetrics and Gynecology to each patient. Every patient was informed that all tests were non-invasive and non-risky. Total information of the patients was encoded and preserved in the checklist and they were not available for real and legal persons. The study was approved by the Research Committee of Ahvaz University of Medical Sciences and ethically by the Ethics Committee of the University. Before starting the study, all participants were given informed consent.
3. Results
According to Table 1 among 230 pregnant women entered this study, 31 women had diabetes. Of these 31 women with diabetes, 22 persons have normal CPR but, 9 of them have low CPR, which has significant analytic value. Of 230 pregnant women entered this study, 9 women had gestational hypertension, which all of them had Low CPR (Table 2).
| Maternal Diabetes | CPR Classification | Total | ||
|---|---|---|---|---|
| > 5 | 2.5 - 5 | < 2.5 | ||
| No | 186 | 9 | 4 | 199 |
| Yes | 22 | 8 | 1 | 31 |
| Total | 208 | 17 | 5 | 230 |
The Frequency of CPR Versus Maternal Diabetes in the Study Population (N = 230)
| CPR | Gestational Hypertension | Total | |
|---|---|---|---|
| Negative | Positive | ||
| > 5 | 208 | 0 | 208 |
| 2.5 - 5 | 10 | 7 | 17 |
| < 2.5 | 3 | 2 | 5 |
| Total | 221 | 9 | 230 |
The Frequency of Gestational Hypertension in the Sample with CPR
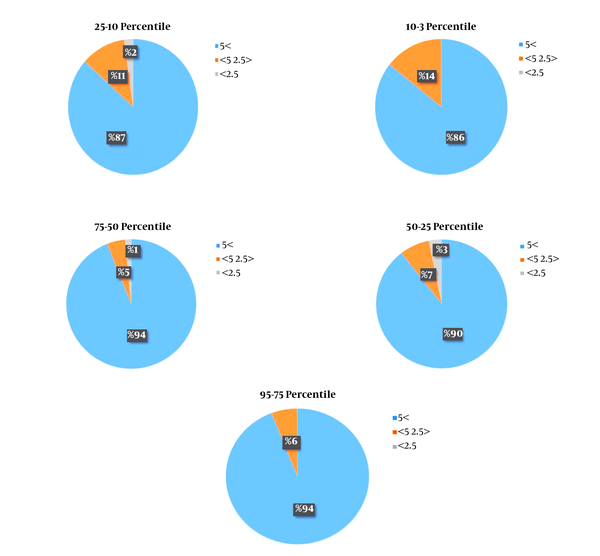
Of total 7 women with diabetes, which used insulin, three women had significantly lower CPR. Of the total 4 women, which used Methyldopa all of them had low CPR. Other drugs had no influence on CPR (Table 3). According to Table 4, there was no significant relationship between PAPP-A and CPR in our study. There was no significant relationship between BMI and CPR in our study. According to the Figure 1, distribution of low CPR in different EFW percentiles, 3 - 10, 10 - 25, 25 - 50, 50 - 75, 75 - 95 were 14%, 13%,10%, 6%, 6%, respectively, showing the presence of low CPR even in high EFW percentiles, but low CPR were more common in 3 - 10 EFW percentile.
| Drug Use | CPR Classification | Total | ||
|---|---|---|---|---|
| > 5 | 2.5 - 5 | < 2.5 | ||
| No use | 183 | 10 | 3 | 196 |
| ASA | 1 | 1 | 0 | 2 |
| Aspirin | 1 | 0 | 0 | 1 |
| Insulin | 4 | 3 | 0 | 7 |
| Levothyroxine | 15 | 0 | 1 | 16 |
| Prednisolone | 1 | 0 | 0 | 1 |
| Metformin | 1 | 0 | 0 | 1 |
| Carbamazepine | 1 | 0 | 0 | 1 |
| Clonazepam | 1 | 0 | 0 | 1 |
| Methyldopa | 0 | 3 | 1 | 4 |
| Total | 208 | 17 | 5 | 230 |
The Frequency of CPR Versus Drug Use
| CPR | PAPP-A | Total | ||
|---|---|---|---|---|
| < 0.4 | 0.4 - 2.6 | > 2.6 | ||
| > 5 | 13 | 190 | 5 | 208 |
| 2.5 - 5 | 4 | 12 | 1 | 17 |
| < 2.5 | 0 | 5 | 0 | 5 |
| Total | 17 | 207 | 6 | 230 |
The Frequency of CPR Versus PAPP-A Values
| Items | P Value (2-Sided) |
|---|---|
| Maternal diabetes | 0.00 |
| Maternal hypertension | 0.642 |
| Taking medication | 0.00 |
Chi-Square Test for Analyzing Research Hypotheses
4. Discussion
In this study, 230 women were studied and the cerebrospinal ratio (CPR) was measured. Diabetes and gestational hypertension are two factors that influence the cerebroplacental ratio.
Gibbons et al. (25) in their study examined the relationship between cerebrospinal CPR and the outcome of delivery and birth in complicated pregnancies, including insulin-dependent diabetes, non-insulin-dependent diabetes, and gestational diabetes, and concluded that regardless of the type of diabetes, there is a significant relationship between low CPR and diabetes. In another study conducted in 2016 by Gibbons et al., there was a correlation between CPR and gestational diabetes (26).
Studies have shown that diabetes can affect the outcome of pregnancy and childbirth. This effect includes fetal complications, such as macrosomia, hypoglycemia, and hypoglycemia in newborns. In a recent study, the effect of diabetes and gestational diabetes on CPR was studied. The results of this study showed that there is a relationship between blood flow to the brain in the fetus and the mother’s diabetes. Gibbons et al. (25) generally examined diabetes and found it related to CPR, the results of this study are consistent with diabetes. On the contrary, the results of this study did not match the results of Gibbons et al. (26).
Gaikwad et al. (27) showed that there was a relationship between CPR and GHTN. Shahinaj et al. (28) concluded in their research that the CPR was a predictor of the adverse outcomes in preeclampsia and GHTN. Parshuram et al. in 2014 showed that CPR is very useful for prenatal monitoring of mothers with gestational hypertension (29).
4.1. Conclusions
The results of this study indicated a relationship between CPR and maternal diabetes, GHTN and drug use. However, there was no relationship between CPR and PAPP-A and BMI. To conduct multicenter studies for study generalization, further studies with a larger sample size to increase the validity of the results, and further studies on the association of CPR with PI in the uterine artery are recommended. It is hoped that more comprehensive results could be presented via further studies with a larger sample size.
4.2. Limitations
This study has some limitations that are worth mentioning. Unfortunately, the duration of study was relatively short; therefore, we suggest that for future studies other factors such as neonatal-maternal complications etc. should be investigated. We also suggest that a study with the same purpose should be conducted with a greater sample size in patients with diabetes and hypertension.