1. Background
The World Health Organization (WHO) announced on March 11, 2020, that the outbreak of the 2019 novel coronavirus (COVID-19) has turned into a global epidemic (1). In the last two weeks, the number of people infected with the virus has tripled, and the number of countries affected has reached 210. To date, more than 1.8 million cases have been reported in 210 countries, of which about 1,400,000 have died (2). The symptoms of the virus are 80% similar to severe acute respiratory syndrome (SARS), and the virus transmits through coughing and sneezing (3). The symptoms of the early stages of COVID-19 infection occur in the form of high fever, sore throat, shortness of breath, and diarrhea. In the later stages, it causes pneumonia and kidney failure and could eventually lead to the patient’s death (4). There is currently no vaccine or effective treatment for the virus, and the only way to prevent is to diagnose the patient early and quarantine the confirmed and suspected cases (5). Authorities in some countries have asked citizens to refrain from attending crowded and public places. The virus has also spread to several countries through travelers, raising concerns around the world and treated global health security.
In turn, global leaders and international organizations have a collective responsibility to develop and maintain a strong global ability to counter the threat of infectious diseases. This ability includes ensuring that financial resources are provided to fill the gap in the readiness for epidemics, which saves humans and achieves a world free of danger and harm. The Global Health Security (GHS) index is the primarily inclusive indicator and benchmark for assessing health security and related capabilities in approximately all world countries; therefore, this index is a necessary tool to deal with the risks of transnational public health of which uses to avoid, shield, manage, and react without disrupting the global trading. In this index, biological events with high consequences are defined as the prevalence of infectious diseases that can overshadow the national or international capacity to manage them.
However, knowing the dangers is not only not sufficient, but also public policy is required to keep the people safe from the concerns of outbreaks, as well as pandemics, to save human lives and to create a world free of danger and harm. Delays in the global response to the COVID-19 pandemic could lead to a shift in the structure of the world and call for a transparent assessment of countries’ public health capacities. These recommendations for epidemic threats, such as COVID-19, could have a geographical scope, intensity, or social impact, as well as overshadow national or international capacity to manage it. The recommendations have been provided; however, many of them have not yet been implemented due to the lack of funding.
Given the importance of the GHS index as a tool to fully assess the health systems of different countries and their capacities to control the spread of the disease, the existing capacities and programs of countries and their readiness to understand the comprehensive effects of epidemics, their specific measures provide credibility and fill in the gaps in the anti-epidemic system, indicators and questions that form the framework of this index, as well as to analyze the capacity of the national health security, could be a global priority.
2. Objectives
Therefore, this study aimed to calculate and evaluate the GHS index in countries affected by the COVID-19 outbreak and its public health-related consequences, as well as its relationship with the case fatality and recovery rates using up-to-date data at the global level.
3. Methods
We reviewed and analyzed the October 2019 GHS index co-leaders joint report in contribution with Nuclear Threat Initiative (NTI) and Center for Health Security (CHS), Johns Hopkins Bloomberg School of Public Health, to review health security capacities on the basis of the GHS index in the context of six categories, including prevention, early detection and reporting, rapid response, health system, compliance with international standards and norms, and the risk environment, is reviewed and summarized. Among its 140 questions, we prioritized not only the capacities of 210 countries and territories around the world using the GHS index. The overall GHS index, as well as prevention, detection and reporting, rapid response, health system, compliance with international standards and norms, and the risk environment scores among all 195 countries were considered. The average overall GHS Index components among all 195 countries assessed are 40.2, 34.8, 41.9, 38.4, 26.4, 48.5, and 55.0 of a possible score of 100, respectively. All scores were normalized to a scale of 0 to 100, where 100 was considered the best health security condition. Then according to the scores obtained by different countries, we classified them into the highest (most prepared), middle (more prepared), and the lowest (least prepared) countries. This work was approved by the Ethics committee of Ahvaz Jundishapur University of Medical Sciences.
3.1. Data Source
Data from global databases, including Worldometer, WHO (6), Disease Control and Prevention Center (CDC) (16), and the weekly report on complications of death and death (prepared by the CDC) were collected and retrieved according to the user guide of data sources for disease registration (7). Owing to the rapid increase in data, the analysis in this study was conducted on April 14, 2020. According to the raw data of countries, the case fatality and recovery rates and their relationship is a unique feature of the GHS index in each country based on the geopolitical considerations of a country and its health system, as well as whether it has tested its capacity to control the spread of the disease. Thus, the case fatality and rate of recovery rates were calculated, then their relationship with GHS index and its six sub-component of GHS was investigated to provide a complete assessment in each country and its health system. Then, the country’s resilience to biological threats has been compared for countries with 1,000 and above COVID-19 confirmed cases (2).
3.2. Statistical Analysis
Continuous variables are reported as range and mean ± standard deviation (SD). Categorical data are expressed as number (percentage). The univariate association between GHS index (and each of its components) with the number of total COVID-19 diagnostic tests, CFR and RR was assessed with correlation coefficient tests. Linear regression models were conducted to examine the association between the explanatory variables and the outcomes of interest. Ridge regression was applied to assess the impact of each parameter on total COVID-19 diagnostics tests, controlling for the effects of population and GPD parameters (model I). Multiple ridge regression analyses were used to determine parameters most predictive of the number of total COVID-19 diagnostic tests (model II). Graphs were depicted with Excel 2013 and SPSS22 (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp). Correlation and regression analyses were performed using the statistical software Stata, version 12 (StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP.). P-values of less than 0.05 were considered statistically significant.
4. Results
This study collected data on 210 countries and territories, of which up to April 14, 2020, 72 countries (34.28%) with more than 1,000 total COVID-19 cases were present (Appendix 1 in Supplementary File). Descriptive statistics of parameters are presented in Table 1.
| Characteristics | Range | Mean ± SD |
|---|---|---|
| Population; million | 0.36 - 1386 | 80.71 (228.38) |
| GDP | 0.01 - 19.39 | 1.26 (3.05) |
| Total cases | 1010 - 587155 | 26369.86 (76379.09) |
| Total death | 2 - 23644 | 1652.38 (4630.98) |
| Total recovered | 25 - 77738 | 6102.27 (15774.32) |
| Active cases | 583 - 526563 | 18612.29 (64612.20) |
| Serious critical | 1 - 12772 | 754.54 (2065.39) |
| Number of total COVID-19 diagnostic tests | 3359 - 2943955 | 204228.02 (425866.98) |
| CFR | 0.15 - 15.78 | 3.92 (3.50) |
| RR | 0.15 - 94.52 | 21.95 (19.58) |
| Prevention | 19.40 - 83.10 | 50.005 (14.34) |
| Detection | 12 - 98.20 | 60.03 (20.08) |
| Response | 19.50 - 91.90 | 50.69 (14.47) |
| Health system | 11 - 73 | 42.87 (14.40) |
| Capacity | 25.80 - 85.30 | 54.77 (13.85) |
| Risk environment | 29.20 - 87.10 | 65.77 (12.85) |
| GHS index | 23.60 - 83.50 | 53.37 (12.82) |
Characteristics of Countries with More Than 1,000 Total Cases
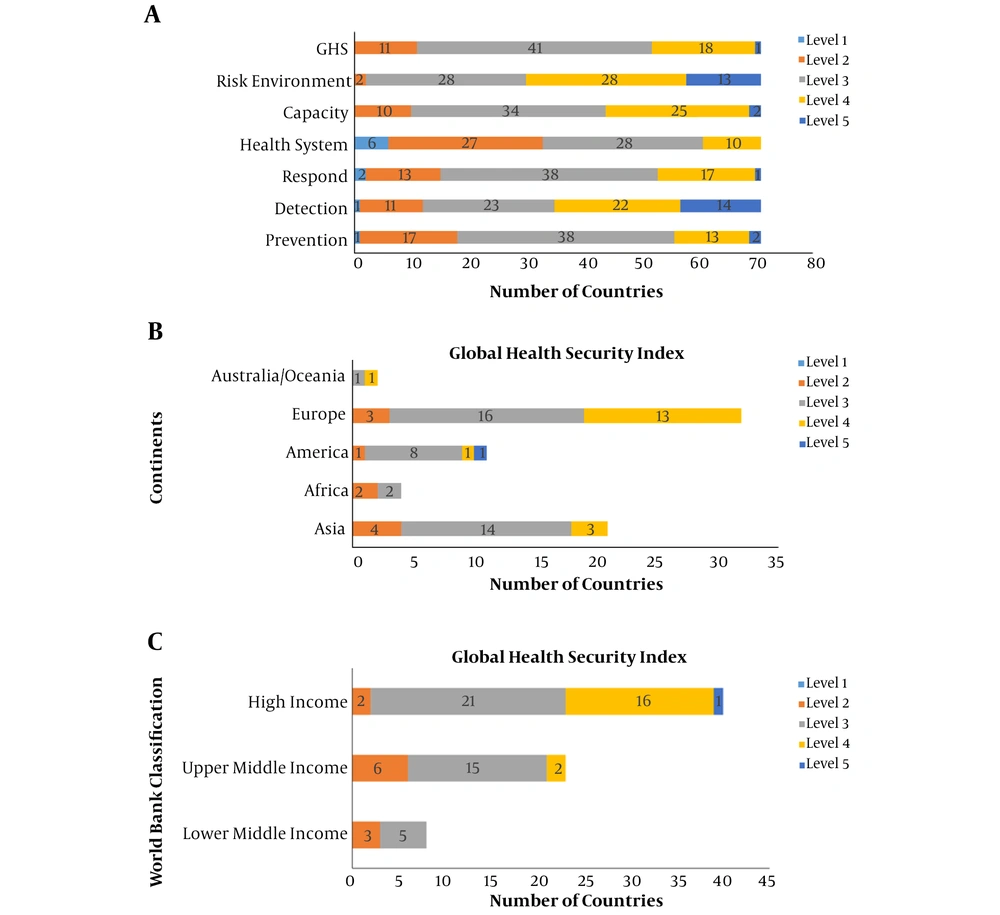
The frequency of countries according to capacities to prevent, detect, respond, health system, capacity, risk environment, and general health score is represented in Figure 1. In this figure, level 1 represents the lowest, while level 5 represents the highest capacity. Nineteen (26.38%) out of 72 countries had overall health safety capacity at levels 4 and 5 (Figure 1). Moreover, 14 (19.45%) countries had relatively high capacities to prevent, 36 (50%) had relatively high capacities to detect, 18 (25%) had relatively high capacities to respond, 10 (13.89%) had relatively high capacities in health system, 27 (37.5%) had relatively high compliance with international standards, and 41 (56.95%) had relatively high-risk environment (Figure 1A). The highest overall health safety capacity at levels 4 and 5 was observed in Europe in thirteen (18.05%) countries (Figure 1B). The highest overall health safety capacity at levels 4 and 5 was observed in high-income countries (Figure 1C).
A, number of studied countries according to capacities to prevent, detect, respond, health system, capacity, risk environment and general health score. Level 1 represents the lowest capacity, while level 5 represents the highest; B, Global Health security Index by continents. Level 1 represents the lowest capacity, whereas level 5 represents the highest; C, Global health security Index by World Bank classification. Level 1 represents the lowest capacity, while level 5 represents the highest.
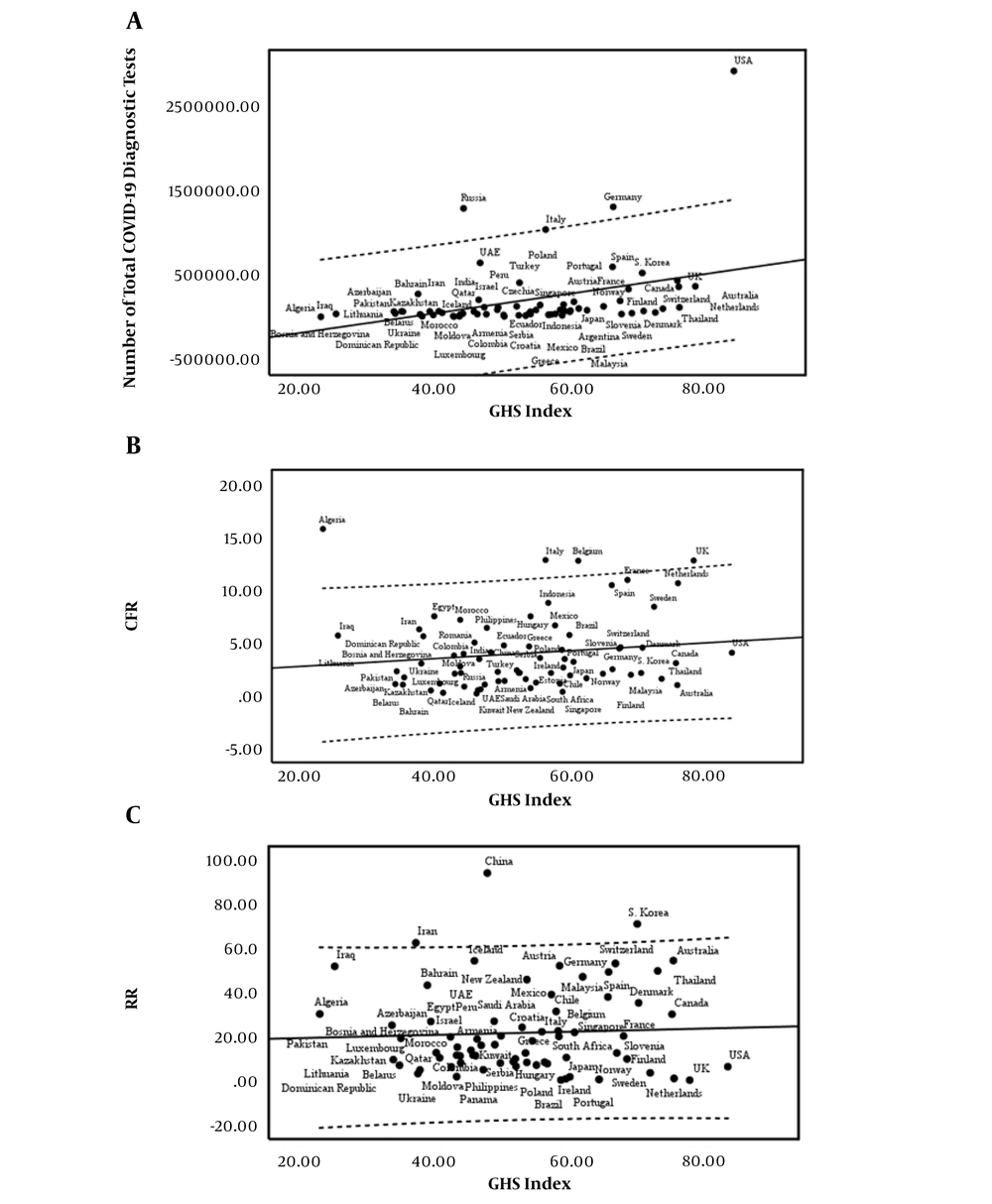
There was no significant association between the GHS index (and its components) with both case fatality rate and recovery rate (Appendix 2 in Supplementary File). The number of total COVID-19 diagnostic tests positively correlated with GHS index (r = 0.363; P = 0.002) and all of its components except for the risk environment index (Appendix 2 in Supplementary File). According to the result of univariate linear regression models, there was a significant association between GHS index (Figure 2) and all of its components (Appendix 11 in Supplementary File) with number of total COVID-19 diagnostic tests (Appendix 3 in Supplementary File).
Using ridge regression, no significant association was found between the parameters and the number of total COVID-19 diagnostic tests after controlling for the effects of population and GDP (Table 2).
| Parameter | Model I | Model II | ||||
|---|---|---|---|---|---|---|
| Beta (SE) | P | R2 | Beta (SE) | P | R2 | |
| Population | - | - | - | 150.61 (246.81) | 0.544 | 0.45 |
| GDP | - | - | - | 91899.56 (15487.18) | < .001 | |
| Prevention | 3718.38 (2756.94) | 0.182 | 0.47 | 162.1787 (4887.926) | 0.974 | |
| Detection | 1819.08 (1934.64) | 0.351 | 0.46 | -468.58 (2736.61) | 0.865 | |
| Responds | 2745.77 (2680.66) | 0.309 | 0.46 | -864.23 (4115.45) | 0.834 | |
| Health system | 4288.48 (2586.44) | 0.102 | 0.48 | 2195.206 (4753.78) | 0.646 | |
| Capacity | 4561.02 (2776.31) | 0.105 | 0.48 | 2849.622 (3980.09) | 0.477 | |
| Risk environment | 4962.31 (2890.10) | 0.091 | 0.48 | 2703.46 (4169.51) | 0.519 | |
| GHS index | 4878.43 (3023.36) | 0.111 | 0.48 | - | - | - |
Results of Multiple Ridge Regression Analyses to Determine Parameters Most Predictive of the Number of Total COVID-19 Diagnostic Testsa
Countries were divided into three categories according to their preparedness levels to face pandemics. In “the most prepared group”, number of total COVID-19 diagnostic tests had a significant positive relationship with the GHS index (r = 0.713; P = 0.006). The recovery rate was negatively associated with the prevention index (r = -0.593; P = 0.033). Case fatality rate was directly associated with the detection index (r = 0.304; P = 0.023) in “more prepared group” (Table 3).
| Preparedness Level | Number of Total COVID-19 Diagnostic Tests | CFR | RR | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CC | 95% CI for CC | P | CC | 95% CI for CC | P | CC | 95% CI for CC | P | |
| Most prepared countries (n = 13) | |||||||||
| Prevention | 0.382 | (-0.214, 0.771) | 0.197 | 0.193 | (-0.400, 0.673) | 0.527 | -0.593 | (-0.862, -0.062) | 0.033 |
| Detection | 0.457 | (-0.125, 0.805) | 0.116 | -0.036 | (-0.576, 0.525) | 0.906 | 0.046 | (-0.518, 0.582) | 0.882 |
| Response | 0.281 | (-0.320, 0.720) | 0.353 | 0.311 | (-0.290, 0.736) | 0.301 | -0.148 | (-0.646, 0.439) | 0.629 |
| Health. system | 0.505 | (-0.064, 0.826) | 0.078 | -0.210 | (-0.682, 0.385) | 0.491 | 0.087 | (-0.487, 0.609) | 0.776 |
| Capacity | 0.545 | (-0.008, 0.843) | 0.054 | -0.210 | (-0.682, 0.386) | 0.491 | -0.286 | (-0.723, 0.315) | 0.344 |
| Risk. environment | 0.015 | (-0.541, 0.561) | 0.962 | 0.285 | (-0.315, 0.723) | 0.345 | -0.258 | (-0.708, 0.342) | 0.395 |
| GHS index | 0.713 | (0.268, 0.908) | 0.006 | 0.113 | (-0.467, 0.625) | 0.713 | -0.309 | (-0.735, 0.292) | 0.305 |
| More prepared countries (n = 56) | |||||||||
| Prevention | 0.212 | (-0.059, 0.454) | 0.123 | 0.150 | (-0.117, 0.397) | 0.269 | 0.035 | (-0.230, 0.295) | 0.799 |
| Detection | 0.096 | (-0.176, 0.355) | 0.488 | 0.304 | (0.044, 0.525) | 0.023 | 0.028 | (-0.237, 0.289) | 0.839 |
| Response | 0.172 | (-0.100, 0.421) | 0.212 | 0.106 | (-0.162, 0.359) | 0.439 | 0.018 | (-0.246, 0.279) | 0.896 |
| Health. system | 0.112 | (-0.161, 0.369) | 0.420 | 0.129 | (-0.138, 0.379) | 0.342 | 0.167 | (-0.101, 0.412) | 0.220 |
| Capacity | 0.193 | (-0.079, 0.438) | 0.162 | 0.199 | (-0.067, 0.439) | 0.141 | -0.142 | (-0.390, 0.126) | 0.298 |
| Risk. environment | 0.143 | (-0.130, 0.395) | 0.303 | -0.060 | (-0.318, 0.206) | 0.658 | 0.193 | (-0.073, 0.434) | 0.154 |
| GHS index | 0.221 | (-0.049, 0.462) | 0.108 | 0.245 | (-0.019, 0.477) | 0.068 | 0.084 | (-0.183, 0.339) | 0.539 |
| Least prepared countries (n = 3) | - | - | - | - | - | - | - | - | - |
Association Between GHS Index and its Component with the Number of Total COVID-19 Diagnostic Tests, CFR and RR in Different Preparedness Levelsa
According to different World Bank countries classifications, countries with more than 1,000 total cases were divided into three categories. In “lower-middle-income economies” group, the case fatality rate is positively related to detection, response, and risk environment indices. Recovery rate has a negative association with health system index (r = -0.637; P = 0.09). Case fatality rate negatively related to response, health system, and GHS indices in “upper-middle-income economies” group. In “high-income economies”, group case fatality rate and number of total COVID-19 diagnostic tests were positively related to the GHS index and its components except for the risk environment index (Appendix 6 in Supplementary File).
According to different cut-offs for the GHS index and its components, studied countries were categorized. Bivariate correlation between GHS index and outcomes of interest in each subgroup is shown in (Appendix 7 in Supplementary File). Appendix 7 in Supplementary File represents the association between each index with outcomes in subgroups, according to the GHS cut-off.
Countries were divided into five categories, according to their continent. In Asia, case fatality rate had a significant negative relationship with risk environment index (r = - 0.489; P = 0.021). The recovery rate was positively associated with the risk environment index in European countries (r = 0.353; P = 0.048). Also, the case fatality rate was directly associated with the GHS index (r = 0.547; P = 0.001) and its component except for the risk environment index. There was a significant association between the GHS index (and its components except for detection index) with the number of total COVID-19 diagnostic tests in America (Appendix 8 in Supplementary File).
5. Discussion
This study evaluated the GHS index in countries affected by the COVID-19 outbreak and its public health-related consequences, as well as its relationship with the case fatality and recovery rates, which showed a wide variation between countries in terms of prevention, detection, and response to COVID-19. In line with the present study, a recently published report of the International Health Regulations (IHR) on data from 182 countries preparedness, capacity building, and collaboration between countries still need improvement, as well as local readiness for outbreak control, need to strengthen (8). Numerous factors affect COVID-19 emergence and spread within countries and between geographical regions, comprising the national capacities, the ability of detection, prevention, and control, climate-related factors, and population density (9-11). One of the important factors in the context of the GHS index is the health system. Our results revealed a significant correlation between the number of COVID-19 tests and health security capacities (12, 13). Other aspects of such an important variable are implementing public health prevention strategies, such as public awareness about hand hygiene and social distancing (14, 15). Our analysis shed light on the fact that most countries at the top of the list with the highest number of cases, as well as deaths from COVID-19, were in more prepared condition, according to the GHS index. This may point to this issue that health security is essentially weak at the national and global levels (16); thus, no country or region was fully prepared to handle COVID-19 epidemics and pandemics, and each country or region has its own gaps to fill. Many countries have been ranked as regions with low capacities to detect, prevent and combat the outbreak through their experience with former infectious diseases (17, 18). This fact may indicate more than ever that special attention on regions of low human and health development is needed, as well as further improvements in observation with additional international collaboration are required (19, 20).
The WHO claimed that one of the reasons for the large difference in mortality rate among various countries might be the difference in life expectancy, medical facilities, and the number of tests performed. Though Europe and America have become the center of COVID-19 outbreak in the world now, some countries in these regions, such as Belarus that is the only country in Europe whose officials are not seeking fundamental changes in people’s daily lives, have taken a very different approach to combat COVID-19 compared with other European countries and even its closest neighbors such as Russia and Ukraine. While Ukraine is close to declaring a state of emergency, and Russia has closed public places, universities, and schools, canceled public events, and stopped all incoming and outgoing flights (21). Interestingly, the highest prepared region according to the GHS index was Europe, with the most frequent level 4 and above results. Although European countries account for the highest number of COVID-19-confirmed cases and related deaths, this can be attributed in part to the high number of hospital and Intensive Care Unit (ICU) beds (22). Besides, these countries also quickly conducted reliable screening and diagnostic tests for COVID-19 and implemented strict social distancing measures to prevent the outbreak (23). Another possible reason for the rapid test for COVID-19 could be that in some of these countries, such as Germany, private laboratories across the country were free to provide testing and have helped the country test millions of people for the disease.
The most important point is that the condition of the healthcare system, hospital and ICU beds, and mechanical ventilation facilities of a country and its preparedness, which can slow down the course of COVID-19 outbreak, are in what situation; therefore, a sufficient, well-equipped and well-prepared healthcare system in a country is crucial for severe patients infected with COVID-19. Lessons learned from the previous infectious disease spread and emergencies, such as the outbreak of SARS-CoV, MERS-CoV, H1N1 flu, Zika, and Ebola viruses, have lead several countries to make substantial improvement in effective detection, prevention, and the ability to respond to similar conditions (24-26). One of the key components that lead to increasing the ability of a country to respond quickly to the disease outbreak is early detection by the development of laboratories equipped specifically for COVID-19. We observed 50% of countries with robust detection capacities, mostly felled in the European and Asian continents, as well as were from high-income countries. The rapid response capacity relies on the level of preparedness of a country in terms of the availability of health system resources and emergency logistics. The present study findings showed that most countries need more support by national as well as global actions to more strengthen health security. Besides, it seems that many countries, especially low-income countries, not only have not increased their capacity and readiness but also underline the importance of the investment in the ability to combat the disease outbreak (27).
COVID-19 testing provides two functions, including diagnosing people infected with the virus, and monitoring and surveillance, especially in cases where the symptoms are mild or not obvious at all. We observed a significant association between numbers of COVID-19 tests performed and case fatality rate, as well as GHS index. This means that in most prepared countries to deal with the disease outbreak, more will be tested in less time, and as a result, more will be diagnosed (28). Thus, less testing or insufficient testing at the proper time may decelerate resourceful patient care and sending a heavily lagged view of the COVID-19 outbreak to the healthcare system and its decision-makers.
5.1. Limitations
Even with clear and precise descriptions for each of the GHS index components and the index itself, finding the relevant data points remains controversial. Thus, although quicker detection and response to COVID-19 outbreaks help to diminish the total number of cases, it is still unclear whether process improvements, which may be reflected in measuring the GHS index, will improve health outcomes in a population. There are many confounding factors, which may affect the analysis, including political wills and readiness for the control of COVID-19, insufficient medical service in countries with a big outbreak, insufficient tests in countries with a big outbreak; besides, numbers of confirmed cases may not be a reliable assessing factor in countries with low GHS indexes.
5.2. Conclusions
Measuring the GHS index for each country, as well as globally, may help create a progression in faster detection and response to disease outbreaks, as well as improve health security at national and global levels. But it is necessary to work with countries and their regional networks to improve the approach to share accurate and up-to-date local knowledge with the global health community. In light of necessities to enhance local and global capacities, preparedness, and response to the COVID-19 outbreak, future efforts might be beneficial to measure global health security when using complementary modes of data collection. Finally, this shows the importance of timely and comprehensive evaluations and emphasizes that even more must be done to build surge capacity to prevent, detect, and respond to such emergencies around the world.