1. Background
At the end of 2019 December, prevalence of an infectious disease was reported in Wuhan, China, which was originated from a corona virus and officially was termed as coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO) (1). According to the studies, COVID-19 patients suffer from low psychological flexibility and, given the current status of the disease in the world, are faced with psychological disorders such as depression, stress, and anxiety (2, 3). The pathogenic feature of the virus, its speed of spread, and its mortality rate might jeopardize mental health of general people, including infected ones (4). Depression is considered as one of the most prevalent disorders among patients with COVID-19. Identifying and examining depression is so important, and if it is left unidentified and untreated, the patients may suffer from immunodeficiency and commit suicide at the end (5). Stress is a construct that can increase depression, anxiety, worry, and other forms of psychological distress among patients when combined with other psychological factors. Physiologically, anxiety and stress can affect the immune system and make people prone to physical and psychological disorders by diminishing body’s resistance (6). Anxiety is characterized by excessive and persistent (often unrealistic) anxiety. Anxiety disorder is important because of individuals’ loss of efficiency and the need to use medical resources (7). People with Corona disease suffer from a high prevalence of anxiety (4).
Psychological interventions are among applicable treatments to help deal with their problems. The mindfulness-based cognitive therapy (MBCT) is one of the latest treatments introduced for depression, stress, and anxiety (8). Mindfulness redirects an individual’s attention toward inner and outer experiences of the present and leads to accept them without any change or interpretation. It includes attending in purposeful and specific ways in the present and without prejudice (9). Evidence suggests that MBCT has positive effects on physical and psychological symptoms and can be an effective additional therapy for physical ailments (10). The results of a research study conducted to examine the effectiveness of MBCT on patients with depression, there was a significant reduction in depressive symptoms (11). In a study, Nila et al. (12) showed that reducing stress through mindfulness enhances distress tolerance and resilience. In another study, Denninger et al. (13) showed that MBCT affects health through changing the mind. Fordham et al. (14) found that MBCT significantly affects patients’ emotional beliefs about stress, anxiety, and quality of life. Thus, this treatment can provide a perceptual structure to help patients to accept their problems. Based on these notions and given the growing prevalence of COVID-19 and the significant role of psychological factors in the treatment process, it is necessary to create effective interventions to help patients who face these problems. So far, few studies have been performed on the effectiveness of MBCT in patients with COVID-19. Therefore, examining the effectiveness of MBCT to restore mental health in patients and improve physical health is important and necessary.
2. Objectives
The current research aimed to determine the effectiveness of the MBCT on depression, stress, and anxiety among people with COVID -19.
3. Methods
This study is an experimental study with a pretest-posttest design and control group in which the effectiveness of the independent variable “MBCT” is examined on the dependent variables "depression, stress, and anxiety" among patients with COVID-19 referred to health centers of Ahvaz, Iran. The statistical population of the study included all recovered COVID-19 patients referred to health centers in Ahvaz in 2020. In this regard, 144 COVID-19 patients filled out the Depression, Anxiety, and Stress scale (DASS-21) questionnaire. Out of 59 patients with the highest scores, 30 patients who were eligible to enter the study were selected using simple random sampling method and randomized into either experimental (MBCT) or control group. The inclusion criteria were holding a minimum of high school diploma, in the age range of 30-50 years, and not using psychiatric and cardiovascular drugs. The exclusion criteria were two consecutive or non-consecutive absences, the use of psychiatric or cardiovascular drugs during the study, and inaccurate homework and home practices for two consecutive or non-consecutive sessions. The sample size was determined 15 in each group according to the formula presented by Chow et al. (15) as follows:
Data collection tools were: (1) demographic characteristics questionnaire that was designed according to the objectives of the study including age, gender, level of education, and medical history; (2) the short form of DASS-21 questionnaire, in which depression, stress, and anxiety were measured. This scale has been developed by Louis Band (1995) and includes 21 items associated with symptoms of negative moods (16). The participants should determine the intensity (frequency) of the symptoms in the statements that represent their experience over the past week with a 4-point scale scoring (between zero and 3). Each subscale includes seven items, which are scored by summing all the seven items. The depression subscale includes items 3, 5, 10, 13, 16, 17, and 21; the stress subscale includes items 1, 6, 8, 11, 12, 14, and 18; and the anxiety subscale includes items 2, 4, 7, 9, 15, 19, and 20. Higher scores in this scale indicate higher degrees of depression, stress, and anxiety in subjects (17).
Lovibond and Lovibond (18) reported 0.77 for validity of DASS-21 and Cronbach’s α was.89, 0.84, and 0.83 for the depression, anxiety, and stress subscales, respectively. Reliability and validity of the scale has been examined by Samani and Jokar (19) in Iran, that reported the test-retest validity of the scale for depression, anxiety, and stress as 0.8, 0.76, and 0.77, respectively, and its validity was confirmed using confirmatory factor analysis.
In the current research, Cronbach’s α was 0.86, 0.83, 0.82, and 0.81 for the depression, anxiety, and stress subscales and the total scale, respectively.
To start the study, patients were randomized into two groups, including an experimental group, in which they received the MBCT intervention and a control group. The intervention was started immediately after assigning the groups by the corresponding author. The patients in the experimental group received eight 90-minute sessions of MBCT, while the control group received no intervention. The control group was assured of receiving the intervention after completion of the research process. A summary of Kabat-Zinn’s mindfulness skills training sessions (20) is given in Table 1. After the intervention, the post-test was performed using the questionnaire. Mean, and standard deviation indices were used to provide descriptive information and at the inferential level, statistical indices of univariate and multivariate analysis of covariance were used. The obtained data were analyzed using SPSS software version 23. The statistical significance level was considered 0.05.
| Sessions | Contents |
|---|---|
| One: Auto navigation | Determining the principles and rules of the course and body scan meditation. |
| Two: Facing obstacles | Body scan meditation and focusing on a daily activity in a different way. |
| Three: Mindful breathing | Mindful movement, practice of stretching and breathing, and distinguishing thoughts from realities. |
| Four: Stay in the present | Five-minute mindfulness observing, meditation, and mindful walking. |
| Five: Acceptance and permission | Meditation sitting and emphasis on how to react to thoughts and feelings. |
| Six: Thoughts are not facts | Meditation sitting, alternative thoughts, and perspectives. |
| Seven: How can I best take care of myself? | Meditation sitting, awareness of breathing, thoughts, and emotions, and creating constructive solutions. |
| Eight: Use what you have learned to cope with mood swings in the future | Practicing body scan and reviewing the whole program: what is learned in the group and planning for the future. |
Protocol of the Mindfulness-Based Cognitive Therapy Sessions
4. Results
In “descriptive findings”, the frequency and frequency percentage of the participants’ demographic properties are presented, followed by mean and standard deviation of the variables.
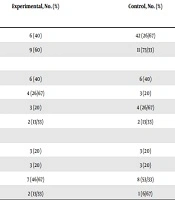
Based on the reported results of Table 2, there were no significant differences between the two groups in terms of the demographic variables (P > 0.05).
| Variables | Experimental, No. (%) | Control, No. (%) |
|---|---|---|
| Gender | ||
| Male | 6 (40) | 42 (26/67) |
| Female | 9 (60) | 11 (73/33) |
| Age | ||
| 31 - 35 | 6 (40) | 6 (40) |
| 36 - 40 | 4 (26/67) | 3 (20) |
| 41 - 45 | 3 (20) | 4 (26/67) |
| 46 - 50 | 2 (13/33) | 2 (13/33) |
| Education | ||
| Diploma | 3 (20) | 3 (20) |
| Associate degree | 3 (20) | 3 (20) |
| Bachelor degree | 7 (46/67) | 8 (53/33) |
| MA | 2 (13/33) | 1 (6/67) |
The Participants' Demographic Info
The results of Table 3 show that the scores of all three variables in the experimental group decreased in the post-tests compared to the pre-tests, while there was no change in the control group.
| Variables | Pre-Test, Mean ± SD | Post-Test, Mean ± SD |
|---|---|---|
| Depression | ||
| Experimental | 15.44 ± 1.76 | 10.22 ± 1.13 |
| Control | 16.08 ± 1.83 | 15.94 ± 1.79 |
| Stress | ||
| Experimental | 25.76 ± 3.21 | 16.82 ± 2.42 |
| Control | 26.48 ± 3.50 | 25.98 ± 3.57 |
| Anxiety | ||
| Experimental | 19.53 ± 2.38 | 15.48 ± 1.86 |
| Control | 19.18 ± 2.34 | 18.83 ± 2.39 |
Mean and Standard Deviation of the Research Variables
Levin test was used to check the homogeneity of variances presumption. The results showed that homogeneity of variances presumption was confirmed in the variables of depression, stress, and default anxiety in the post-test (P > 0.05). The results of M-box test to check the homogeneity of variance-covariance matrices showed that the variance-covariance matrices presumption was confirmed in the post-test (P > 0.05). In addition, the test results of the normality of the research variables in the evaluation stages based on the Kolmogorov-Smirnov test showed that the assumption of normality for the dependent variables including depression, stress, and anxiety in the pre-test and post-test was confirmed in both groups (P > 0.05).
As Table 4 depicts, the results of all four tests showed that the intervention had a significant effect on at least one of the dependent variables. Since multivariate analysis of covariance is valid, the effect of intervention on each of the dependent variables can be assessed separately.
| Effect | Tests | Value | F-Value | P-Value | Effect Size | Statistical Power |
|---|---|---|---|---|---|---|
| Intervention methods | Pillai effect | 0.834 | 97.164 | 0.001 | 0.813 | 0.931 |
| Wilks Lambda | 0.019 | 97.164 | 0.001 | 0.813 | 0.931 | |
| Hotling effect | 1.973 | 97.164 | 0.001 | 0.813 | 0.931 | |
| The biggest root on | 1.973 | 97.164 | 0.001 | 0.813 | 0.931 |
Results of Multivariate Analysis of Covariance to Examine the Effectiveness of the Mindfulness-Based Cognitive Therapy on the Dependent Variables
As Table 5 show, the intervention significantly reduced the variables of depression, stress, and anxiety in COVID-19 patients (P < 0.05).
| Dependent variable | Effect Source | Total Squares | Freedom | Mean Squares | Statistic F | Validity | Effect Value | Statistical Power |
|---|---|---|---|---|---|---|---|---|
| Depression | group | 39.520 | 1 | 39.520 | 91.466 | 0/0001 | 0/753 | 0.885 |
| Stress | group | 43.589 | 1 | 43.859 | 99.158 | 0/001 | 0/860 | 0.948 |
| Anxiety | group | 45.151 | 1 | 45.151 | 97.687 | 0/0001 | 0/829 | 0.936 |
Results of Univariate Analysis of Covariance in the Context of Multivariate Analysis of Covariance
5. Discussion
The aim of this study was to determine the effectiveness of MBCT on the symptoms of depression, stress, and anxiety in COVID-19 patients. Mindfulness helps people identify situations that lead to depression, stress, and anxiety, get to know themselves better, identify their strengths and weaknesses, and then deal with them using coping strategies. As a result, they find the strength to control their anxiety and worrying thoughts, and consequently, depression, stress, and anxiety levels are continuously reduced (21). The results of this study are in line with those of Mackenzie et al. (22), Sohn et al. (10), and Sepanta et al. (23), that confirmed the effectiveness of this treatment on depressive, stress, and anxiety disorders. For example, Mackenzie et al. observed a reduction in depressive symptoms in studies that examined the effectiveness of MBCT on patients (22). The results of Sohn et al. (10) showed the effectiveness of mindfulness-based cognitive-behavioral therapy in improving anxiety and stress symptoms in kidney patients. Sepanta et al. (23) showed the effectiveness of mindfulness-based therapy on reducing pain-related anxiety in patients with leukemia. In order to explain these findings, it can be said that the disease overshadows individuals’ various functions and leads to changes in their attitudes and thoughts over time due to its physical, psychological, and social limitations. The presence of depression in these patients can be due to the clinical condition of the disease and the limitation of these patients due to the prevailing physical and psychological conditions, which itself is again considered as an aggravating factor of the disease. In explaining the findings of this study in reducing depression in the post-test and follow-up steps, we may mention that mindfulness reduces negative thoughts in depressed patients through emotional regulation (24). MBCT offers a distinguished way to deal with excitement and distress. Letting go of negative thoughts and not engaging in them prevents the person from mental rumination. In mindfulness exercises, people realize the connection between thoughts, emotions, and bodily sensations at every moment, and as a result of this awareness, depressive thoughts and states are identified and gradually diminished by practicing letting go of and accepting these thoughts (25). Due to the mindful exercises and being in the moment and awareness of the bodily senses, patients focus more attention on the body, which in turn increases the body awareness, feelings, and thoughts related to anxiety, which improve person’s sense of control over symptoms and lead to reduced anxiety. Stress and anxiety are active factors in creating and increasing dysfunctional thoughts and worries. Segal et al. believe that MBCT is a key element in raising the necessary self-awareness for empowerment and optimal responses in critical situations to prevent the experience of anxiety and acts as a strong preventive stimulus (26). According to the findings of the present study and aforementioned research, it can be concluded that MBCT can be effective in reducing patients’ psychological symptoms and bring about happiness and joy in their daily activities through changes in patients’ cognitive content and providing strategies to deal with disease-related problems.
The most important limitations of the current research were: not comparing the results based on gender, lack of follow-up assessment (due to time constraints), use of self-report tools for data collection, non-random sampling, and a small sample size that can affect the results of the research. Therefore, comparing the results based on gender, follow-up assessment of the effectiveness of the results, and using interviews to collect data are recommended. It is also suggested that further research be conducted with a larger sample size and the results be announced to counseling centers and hospitals for information and operation, and to use this treatment for clients.