1. Context
The first cases of the global coronavirus 2 (SARS-CoV-2) or COVID-19 pandemic were observed in Wuhan, China, in December 2019 and spread out quickly worldwide (1). COVID-19 can mainly be spread through respiratory droplets and is generally diagnosed using the real-time reverse transcription-polymerase chain reaction (rRT-PCR) test. However, all suspected patients cannot undergo the rRT-PCR test for COVID-19 (2).
This is while chest computed tomography (CT) images can detect the disease more quickly than rRT-PCR. Moreover, the CT images are more sensitive in the diagnosis of the disease. Accordingly, the CT scan has become an essential tool to diagnose and evaluate the severity of the COVID-19 infections (3-5).
According to current experience, the disease symptoms appear earlier in lung imaging than other clinical symptoms as such imaging in the clinical screening of the COVID-19 infection is critical. In this regard, high-resolution computed tomography (HRCT) is now of paramount importance in evaluating the lesion nature and locating the disease scope (3).
Although chest radiography is mainly used for the early assessment of pulmonary diseases, CT in many cases is superior to chest radiography for the accurate diagnosis of chest diseases. However, it is established that HRCT is superior to the chest radiography and conventional CT in evaluating the pulmonary parenchymal abnormalities. HRCT can be impressive for detecting the small foci of parenchymal cavitation in the areas of confluent pneumonia and the areas of dense fibro calcific disease, which are associated with the distortion of the underlying lung parenchyma. Furthermore, the chest HRCT is superior to the conventional CT due to its thinner and more accurate cuts in the diagnosis of lung diseases (4).
Pulmonary inflammation is the significant pathologic expression of the COVID-19 disease. The COVID-19 expression in the chest CT images usually includes ground-glass opacity (GGO), consolidation, vascular enlargement, GGO mixed with consolidation, interlobular septal thickening, and air bronchogram (5).
Although viruses usually cause respiratory infections, the imaging findings of the viral pneumonia are diverse and may be similar to other non-viral infections or inflammatory diseases. The identification of underlying viral pathogens may not always be easy. There are several indicators associated with the pathogenesis of viral infections, which can be applied to determine viral pathogens according to imaging patterns. Viruses in the same viral family demonstrate a pathogenesis analogue to pneumonia. Although normal patterns detect not all cases, the imaging patterns of viral pneumonia can be determined considering viral families. Since accurate detection is not possible only by relying on imaging specifications, recognizing patterns of viral pneumonia may help differentiate viral pathogens. Accordingly, clinical features such as age and the immune condition of patients, seasonal changes, and the prevalence of communities, and pathogenesis can affect imaging (6).
2. Objectives
Concerning what was mentioned and the significance of detecting and classifying the severity of the COVID-19 disease, this systematic review aimed to evaluate and classify the COVID-19 disease manifestations in the HRCT images of patients' chests. The study results can provide a comprehensive and concise reference on the appearance of various types of involvement and lung lesions and the extent of these lesions for patients with severe diseases. In the presented systematic review, relevant studies were evaluated from different perspectives, such as the reported lesion types in patients' lungs and the severity and the extent of lung involvement, which would be helpful for other researchers.
3. Data Sources
This systematic review was performed according to the PRISMA-ScR guidelines (7).
3.1. Search Strategy
To review different manifestations of the HRCT images for COVID-19 infection in patients' lungs, we systematically searched four major indexing databases (namely PubMed, Science Direct, Google Scholar, and Cochrane Central) for articles published by May 2021 using keywords such as HRCT, COVID-19, and Manifestations. No language restriction was considered. Then articles irrelevant in titles were excluded. Abstracts were screened for their relevance to the study.
3.2. Inclusion and Exclusion Criteria
The title and abstract screening of the primarily selected studies for inclusion or exclusion was independently performed by the reviewers (S. A. & E. R.). Any disagreement between two reviewers was resolved by either discussion or the help of a third reviewer (M. T.). Only original articles were included providing that they addressed the following characteristics: (1) The HRCT manifestations of COVID-19, (2) lung extent involvement, and (3) human sample. Studies were excluded if they were (1) narrative or systematic reviews, (2) irrelevant to the HRCT manifestations of COVID-19, (3) irrelevant to the concerned subject, (4) letter to editorial, and (5) guidelines.
4. Results
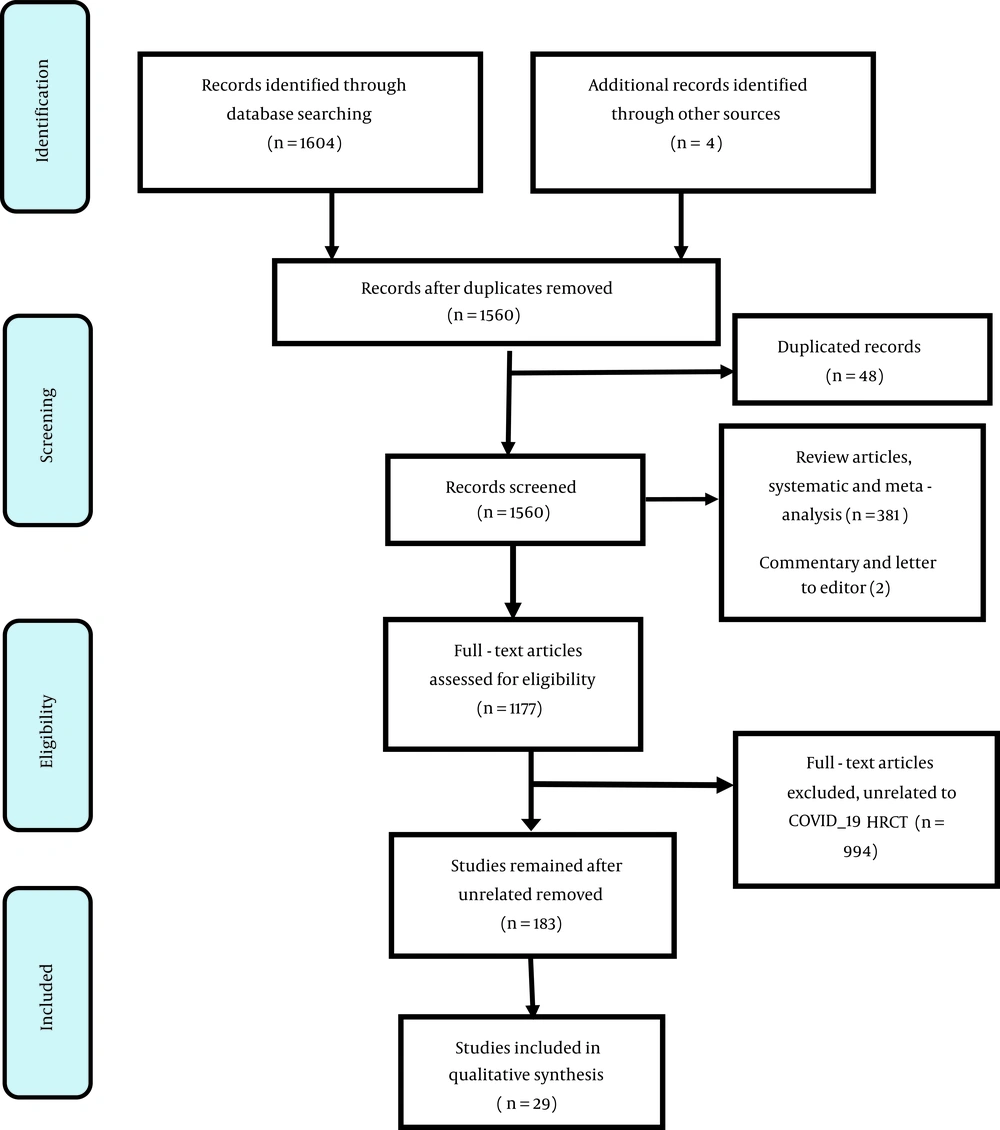
The search procedures revealed 1604 records, and 48 duplicated records, 381 systematic review articles, and two commentaries and letter to editor records were excluded. Moreover, 994 records were excluded since they were not related to the subject and did not have a specific conclusion. Finally, 183 studies remained for the full review, 29 of which were included in the study based on the inclusion criteria, as presented in Figure 1.
5. Conclusions
Although viruses usually cause respiratory infections, the imaging findings of viral pneumonia are diverse and may be similar to other non-viral infections or inflammatory diseases. The identification of underlying viral pathogens may sometimes be challenging. There are several indicators associated with the pathogenesis of viral infections, which can be applied to determine viral pathogens according to imaging patterns. Viruses in the same viral family demonstrate a pathogenesis analogue to pneumonia. Although normal patterns detect not all cases, the imaging patterns of viral pneumonia can be determined considering viral families. Since accurate detection is not possible only by relying on imaging specifications, recognizing patterns of viral pneumonia may help differentiate viral pathogens. Accordingly, clinical features such as age and the immune condition of patients, seasonal changes, and the prevalence of communities, and pathogenesis can affect imaging (6).
Pulmonary inflammation is the significant pathologic expression of the COVID-19 disease. The COVID-19 expression in chest CT images usually includes ground-glass opacity (GGO), consolidation, vascular enlargement, GGO mixed with consolidation, interlobular septal thickening, and air bronchogram (5). In this study, we aimed to prepare a comprehensive review to evaluate all studies on the HRCT manifestations of COVID-19 disease, which addressed in patients' lungs and the commonly infected lung lobe concerning the extent of lung involvement.
According to the results of reviewed articles (Table 1), most of the studies were completed in China, with sample sizes of three to about 4000 patients.
| Country/ID | Authors | Sample Size | Lung Extent Involvement | Affected Lobe | Mean Age (y) | Type of Lesion (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GGO | Irregular Solid Nodules | Fibrous Stripes | Patchy Consolidation | Crazy-Paving | Consolidation /Punctate Ground-Glass Opacities | Air Bronchogram Sign | Consolidation | Reticulation | ||||||
| China | Pan et al. (8) | 63 | 30.2% one affected lobe/ 7.9% two affected lobes/ 6.3% three affected lobes/ 11.1% four affected lobes/ 44.4% five affected lobes | 44.9 ± 15.2 | 85.70 | 12.70 | 17.50 | 19.00 | ||||||
| China | Shi et al. (9) | 81 | 79% bilateral/ 54% peripheral/ 60% unilateral | 49.5 | 65.75 | 15.25 | 2.50 | |||||||
| China | Ai et al. (10) | 1014 | Bilateral | 46 | 3 | 56 | 1 | |||||||
| China | Lin et al. (11) | 52 | 93% lower lobes | 44.98 ± 11.29 | 84.61 | 23 | 26.92 | 13.46 | 53.84 | |||||
| China | Zhu et al. (12) | 4121 | 73.8% bilateral lung involvement | 48 | 68.10 | 20.50 | 40.30 | 35.60 | 44.70 | 32.00 | ||||
| China | Meng et al. (13) | 58 | 44% peripheral/ 14% central/ left upper lobe 31%/ left lower lobe 36%/ right upper lobe 30%/ right middle lobe 12%/ right lower lobe 40%/ | 24% one lobe involvement/two lobes 14% involvement/6% three lobes /7% four lobes and 7% five lobes | 42.60 ± 16.56 | 51.70 | 12.10 | 8.60 | 5.20 | |||||
| China | Zhao et al. (14) | 89 | 33% left upper lobe/ 45% left lower lobe/ 29% right upper lobe/ 24% right middle lobe/ 52% right lower lobe/ 64% peripheral/ 25% peribronchovascular/ 21% peripheral and peribronchovascular | 24% one lobe involvement/12% two lobes/ 6% three lobes/ 6% four lobes/ and 20% five lobes | 41 ± 14 | 47 | 14.16 | 30.34 | 23.26 | 11.12 | ||||
| China | Li et al. (15) | 15 | 83.35 peripheral | 48 | 86.50 | 13.30 | 3.35 | 46.70 | ||||||
| China | Wang et al. (16) | 13 | 7.7% central/38.5 peripheral/53.8 non-specific | 15.4% one lobe involvement/ 69.2% bilateral lungs | 49.54 ± 17.419 | 30.80 | 38.50 | 61.50 | 46.20 | 7.70 | ||||
| China | Li et al. (17) | 131 | 83% more than two lobes involved | 20 - 90 | 15 | 5 | 33 | 15 | 47 | 57 | 3 | |||
| China | Zhao et al. (18) | 16 | 44.6 | 64 | 12 | 6 | ||||||||
| Balkan Peninsula | Vegar-Zubovic et al. (19) | 3 | Left upper and lower lobes | 68.3 | 57 | |||||||||
| China | Jiang et al. (20) | 7 | Peripheral and posterior of lungs bilateral | 53.86 ± 12.48 | 100 | 14 | 57 | 14 | ||||||
| China | Hu et al. (21) | 3 | Peripheral of bilateral lungs/ lower lobes and upper lobes | 50.6 | 100 | 66.66 | 33.30 | 66.60 | ||||||
| China | Li et al. (22) | 72 | 72.22 peripheral regions /22.22% central regions | 51.74 ± 11.64 | 47.22 | 13.89 | 52.78 | 11.11 | ||||||
| China | Tan et al. (23) | 160 | 100% peripheral bilateral | 51.6 ± 13.8 | 1.90 | 72.50 | 65 | |||||||
| Korea | Park et al. (24) | 627 | 68% single lobe 32% multiple lobes 77.5% bilateral | 66.75 | 40.80 | |||||||||
| Italy | Cereser et al. (25) | 77 | Bilateral and peripheral | 64 ± 15 | 86 | 26 | 56 | 65 | ||||||
| China | Chen et al. (26) | 98 | Bilateral lung involvement | 43.0 ± 17.2 | 48.80 | 56.20 | 49.40 | |||||||
| China | He et al. (27) | 12 | 58.33% right lung predominant/ 16.67% left lung predominant/ 25% equivalent in both lung/ 91.67% bilateral | 41.67 | 25 | 41.67 | 25 | |||||||
| China | Xu et al. (28) | 41 | Peripheral:95% Central:46.3% Peripheral involving centra:56% Symmetrical:63% | Single lobe:4.8% Two lobes:12% Three lobes:12% Four lobes:29.2% Five lobes:41.4% | <18 (10%) 18 - 50 (60%) >50 (30%) | 73 | 60 | 53.50 | 36.50 | |||||
| China | Zhao et al. (29) | 101 | 82.2% bilateral involvement/ 87.1%pheripheral /54.5% lower lung predominant and multifocal | 21 - 50 | 86.10 | 64.40 | 43.60 | 48.50 | ||||||
| China | Pan et al (30) | 21 | Stage1 = 54% peripheral Stage2 = 59% peripheral Stage3 = 62% peripheral Stage4 = 70% peripheral | 40 ± 9 | Stage1 = 75 Stage2 = 82 Stage3 = 71 Stage4 = 65 | Stage1 = 2 Stage2 = 53 Stage3 = 19 Stage4 = 0 | Stage1 = 42 Stage2 = 47 Stage3 = 91 Stage4 = 75 | |||||||
| America | Azab et al. (31) | 128 | 83.6% bilateral | 49.07 ± 15.89 | 92.20 | 29.70 | 17.20 | 64.80 | ||||||
| London | Pakdemirli et al. (32) | 19 | 80% peripheral | 18 - 100 | 20 | 100 | ||||||||
| Indonesia | Hafiz et al. (33) | 42 | 57.14% multifocal 78.57% bilateral 69% peripheral | 54.7 ± 16 | 42.85 | 7.14 | 11.90 | 30.9 | ||||||
| China | Gao and Zhang (34) | 6 | 33.3% had bilateral lung involvements/ 33.3% with focal subpleural distribution | 40 ± 10 | 83.30 | 66.70 | 16.70 | |||||||
| China | Han et al. (35) | 114 | 98% bilateral | 54 ± 12 | 62 | 2.60 | 24 | 14 | ||||||
| Egypt | Sultan et al. (36) | 85.7% vs. 100% bilateral/ 64.3% vs. 42.3% peripheral distribution. | 70% vs. 80.8% multilobar distribution | 94.3 vs. 88.50 | 5.1 vs 7.70 | 15.7 vs. 3.8 | 25.7 vs. 34.6 | |||||||
Review of Studies on Different Manifestations in HRCT Images for COVID-19 Patients
According to the findings (Table 1), 96.6% of the reviewed articles reported the GGO manifestation in the HRCT images of patients’ lungs. This is while only 13.8% of the reviewed papers referred to fibrous stripes lesions. The frequency of reviewed articles reporting irregular solid nodules, patchy consolidation, crazy-paving, consolidation /punctate ground-glass opacities, consolidation, and reticulation lesions were 55.2%, 20.7%, 34.5%, 34.5%, 34.5%, 65.5%, and 27.6%, respectively.
As presented in Table 1, the GGO lesions were the most frequently observed lesions in HRCT as they were reported almost in all articles. Their frequency in different studies ranged from 5 to 100% (1, 3, 8, 9, 11, 15, 17, 19, 25). The second most observed lesion was consolidations, ranging from about 3% to 75% in some studies (3, 11-14, 19-22, 24, 25).
In some of the reviewed articles, GGO along with consolidation lesions were reported to be 12 - 100%, and air bronchogram signs changed from about 8% to 72% in some other articles (23, 27, 37). However, these lesions were not noticed in some studies. Moreover, lesions such as fibrous stripes or reticulation were reported in a few articles (8-11, 14, 15, 17, 18, 22, 23, 26, 29, 35).
As mentioned, GGO, consolidation, and irregular solid nodules were the most common manifestations in the HRCT of COVID-19 patients in reviewed articles. These findings were in line with those reported by Khaliq et al. (1), Wan et al. (37), and Ishfaq et al. (38). In their systematic reviews, these researchers reported GGO lesions and consolidations as the most frequent lesions in the HRCT of the COVID-19 patients. In this regard, Khaliq et al. (1) reported the frequency of GGO lesions to be 88.5% and that of consolidation manifestation to be 52.8%. Further, Wan et al. (37) reported the frequencies of GGO and consolidation manifestations as 69% and 47%, respectively. Ishfaq et al. (38) also reported the frequencies of GGO and consolidation manifestations in their study as 71.6% and 35.2%, respectively.
According to the findings of the reviewed articles, lesions diagnosed by HRCT, were mainly detected in the peripheral subpleural section of the lungs, mainly in the posterior or the lower lobes. Moreover, most of the patients had bilateral lung involvement. Lesions may expand from the periphery to the center by deterioration.
Furthermore, according to the results of the reviewed articles, the extent of lung involvement varied in the studies, indicating the severity of the disease (9, 11-17, 27-36).
Pan et al. (30) reported the highest severity of lung abnormalities in chest CT about ten days after the primary inception of symptoms for recovered COVID-19 patients (without intensive respiratory distress during the disease period). According to these researchers, different stages determined for lung abnormality were stage I, stage II, stage III, and stage IV. These stages include 0 - 4, 5 - 8, 9 - 13, and ≥ 14 days, respectively.
As noticed in (Table 1), 54% of observed lesions had peripheral distribution for stage I patients. Moreover, the peripheral distributions of lung lesions in patients’ chest CTs were 59%, 62%, and 70% for stages II, III, and IV, respectively.
Regarding the extent of lung involvement, Khaliq et al. (1) reported 24.1% unilateral, 75.8% bilateral, 29.8% central, 81.6% peripheral, 27.5% mixed (central + peripheral) involvement of lungs in patients. Furthermore, Wan et al. (37) observed 70% right lower lobe and 67% peripheral distribution for lung involvement.
In a same vein , Li et al. (5) considered 24 COVID-19 patients with the moderate-severe disease. The results of imaging comparison in their study revealed that, as for patients with moderate COVID-19, the nature of simultaneous imaging of the grand glass view, scattered shadows, and mixed shadows in both lungs was that of the grand glass view in both lungs with air bronchogram. The likelihood of progression of severe conditions in these patients increased, and the differences were statistically significant.
In a similar vein, Wang et al. (16) reviewed the CT findings distinguishing between COVID-19 and influenza pneumonia. They evaluated the CT scans of 13 patients with COVID-19 and 92 confirmed influenza patients (namely 76 and 16 type A and type B influenza patients, respectively). They evaluated some features of the CT images as the distribution of pulmonary lesions, the number of the involved lobe, lobe dominance, border, contour, grand glass superficies involvement template, bronchial wall thickening, air bronchogram, interstitial wall thickening, intracellular wall thickening, and pleural effusion for COVID-19 and influenza patients. Finally, they concluded that the environmental and nonspecific distributions in the COVID-19 patients' CT images had a significantly higher frequency than those of the influenza patients. Furthermore, most lesions in the COVID-19 group illustrated moderate lobe localization; however, for the influenza group, the lesions were predominantly settled in the lower lobe of the lung. Moreover, scans of the COVID-19 patients presented a clearer and smaller contour margin compared to the influenza group. The COVID-19 patients had a patch or a combination of GGO turbidity and consolidation; however, the cluster pattern and bronchial wall thickening were more prevalent in the influenza group (16). Similarly, Zhao et al. (18) observed certain changes in the COVID-19 images compared them with the images of the common pneumonia virus.
Another point in the reviewed literature was noted by Leonard-Lorant et al., who reported the acute pulmonary embolism associated with COVID-19 for 32 (30%) out of 106 COVID-19 patients (39).
As it was noted, different lesions may emerge in the chest CT of the COVID-19 patients. Pan et al. (8) classified and reported the CT manifestations of COVID-19 patients as follows: background glass nodules, stained/perforated glass opacities, patchy consolidation, fibrous stripes, and irregular solid nodules. Moreover, Khaliq et al. (1) showed that the typical image finding on HRCT was GGO with multilobe involvement. He concluded that CT-SS (chest CT severity scoring) helps categorize pneumonia into different types and identify patients with severe diseases.
Further, Han et al. (35) declared that the radiologic-pathologic correlation needs to be more explored as itis expected to specify prognostic imaging features and clinical treatment guidelines effectively.
The early detection and isolation of the COVID-19 patients have a significant impact on controlling this pandemic, particularly for patients with false-negative RT-PCR or patients with no detectable symptoms (35). Since RT-PCR indicates a low sensitivity, the CT of patients' chest can play a critical role in the diagnosis of COVID-19, particularly for patients with false-negative RT-PCR tests, It is also of great significance in monitoring the clinical trends and assessing the severity of the disease (28). Accordingly, this systematic review study aimed to classify and evaluate the COVID-19 disease manifestations in the CT images of patients' chests to provide a comprehensive and concise reference on the appearance of various types of involvement and lung lesions as well as the extent of these lesions in patients with severe diseases. This research summarized different studies on various manifestations in the HRCT images for the COVID-19 patients.
In sum, different manifestations of COVID-19 in the reviewed articles were GGO, irregular solid nodules, fibrous stripes, patchy consolidation, crazy-paving, consolidation /punctate ground-glass opacities, air bronchogram sign, consolidation, and reticulation. These manifestations were reported with different percentages in the concerned articles. Almost all of the articles (96.6%) reported GGO manifestation in the CT images of patients' lungs, which was at the same time the most frequently observed lesion in the HRCT of patients. This is while only 13.8% of the articles referred to fibrous stripes lesions. The second most observed lesions in the HRCT of the COVID-19 patients were consolidations.
Although bilateral GGO and consolidation were the main specifications in the COVID-19 patients' chest CT, these manifestations may change in different patients and at different stages of the disease. Since the manifestations of the COVID-19 disease are diverse, we need to determine and classify different lesion types regarding the image changes and reinforce the detection of image changes to help physicians in their quick and accurate diagnoses.
Our study had some limitations. For example, we only focused on the HRCT images and did not include articles on patients' radiography. Another limitation was that most of the reviewed studies were conducted in China, and we did not have access to studies on diverse communities from different Countries.