1. Background
Oral candidiasis is the most common opportunistic infection affecting the oral mucosa (1). In most cases, these lesions are due to yeast Candida albicans (2). C. albicans is a weak pathogen and primarily inflicts very young or very old individuals (1-3). Candida infections mostly inflict the mucosal layer, and systemic manifestations leading to death are rarely observed (1, 2). The predisposing factors of this infection include local factors, such as long-term use of dentures, smoking, inhaled steroids, hyperkeratosis, and general predisposing factors, which are related to the immune and endocrine system (4). Some lesions, such as denture stomatitis, angular cheilitis, and median rhomboid glossitis, are associated with Candida infection; however, they might also be due to bacteria (5). Candida is a part of the normal flora of the oral cavity with a prevalence of 90%. Candida is more common in women than in men and in summer than in other seasons (2). The prevalence of Candida is higher in hospitalized individuals (3).
The other two Candida species responsible for oral candidiasis are Candida glabrata and Candida tropicalis. C. glabrata is highly observed in younger patients than in adults. On the other hand, C. tropicalis is known to be associated with neutropenia and malignancy in patients (6). C. glabrata is unable to change from yeast to hyphae; nevertheless, due to its different virulence factors, such as thick biofilms, it is still known as pathogenic. It escapes from the host immune system and does not cause any serious damage. C. tropicalis also has several important virulence factors, such as adhering to epithelial and endothelial cells, lytic enzymes, the ability of switching phenotypes, and a strong biofilm. Increased resistance of these species to some antifungal drugs, such as azoles and echinocandins, has recently been reported and received much attention (7).
Aloe barbadensis or Aloe vera is one of the native plants in Northern Africa. Its fleshy leaves contain a gel that packs all the plant’s beneficial properties. The gel could be used to treat internal and external sores of the human body. The gel contains some glycoproteins, which inhibit swelling and pain, and accelerates the remission process. It also contains polysaccharides that stimulate the growth and repair of skin. Its repairing properties are attributed to a compound called glucomannan, which is rich in polysaccharides, such as mannose. Aloe vera gel not only increases the collagen in sores but also increases the transverse connections while changing the collagen structure (8-13).
Aloe vera-derived glycoprotein exerts anti-inflammatory and antimicrobial effects. Moreover, its hydroalcoholic extract manifests fungicidal effects (8). The most prominent property of Aloe barbadensis is its laxative effect when used orally. It can also be used topically to heal sores and burns. Moreover, it could be used in cosmetics, particularly sunscreens (9, 10). The effects of Aloe vera on oral sores are also proved (11).
In treatment, before using antifungal drugs, it is necessary to identify the predisposing and the local factor (2). The antifungal drugs are divided into two groups, polyenes and azoles. The polyenes include nystatin and amphotericin B, which are the first-line treatment option in primary candidiasis. Nystatin cannot be absorbed through the gastrointestinal tract, does not cause drug resistance, and acts through an adverse effect on ergosterol production, which is critical to membrane integrity (10). Moreover, this drug is effective in fungal adhesion. Side effects, such as diarrhea, nausea and vomiting, and abdominal pain, were observed in patients taking the drug. Other side effects, such as oral burning, were also observed (14).
2. Objectives
Given the increasing prevalence of individuals afflicted with candidiasis due to some factors, such as a compromised immune system, endocrine diseases, and local factors, such as smoking and using steroids, which are more commonly used than herbal medicine, and individuals’ current demand for a treatment containing herbal and organic compounds, this study aimed to evaluate the effects of Aloe vera gel on Candida and compare its effects to those of nystatin.
3. Methods
3.1. Materials and Microorganisms
The present study was carried out using Aloe vera gel (Barij Essence Co., Kashan, Iran) and nystatin (Sigma-Aldrich, USA). C. albicans PFCC 89-3003, C. glabrata PFCC 52971, and C. tropicalis PFCC 89-1456 were also collected from the Pathogenic Fungi Culture Collection of the Pasteur Institute of Iran.
3.2. Antimicrobial Assay
The minimum inhibitory concentrations (MICs) of Aloe vera and nystatin were determined using the broth microdilution method (15). First, a colony of each Candida species was inoculated into the Mueller-Hinton medium and incubated at 37 °C for 24 hours. Then, a 0.5 Mcfarland standard suspension equivalent to 1.5 × 108 colony-forming units was prepared. Afterward, Aloe vera (1000 μL/mL) and nystatin (100 μL/mL) prepared stocks in dimethyl sulfoxide (16) were serially diluted from 1:1 to 1:2048, and the microorganisms were added to each well taken from the standard suspension followed by 24 hours of incubation in order to screen further growth inhibition.
3.3. Statistical Analysis
The data were then inserted into SPSS software (version 24) and statistically analyzed using the one-way analysis of variance and posthoc turkey’s test. In this study, a P-value less than 0.05 was considered statistically significant.
4. Results
4.1. Aloe vera
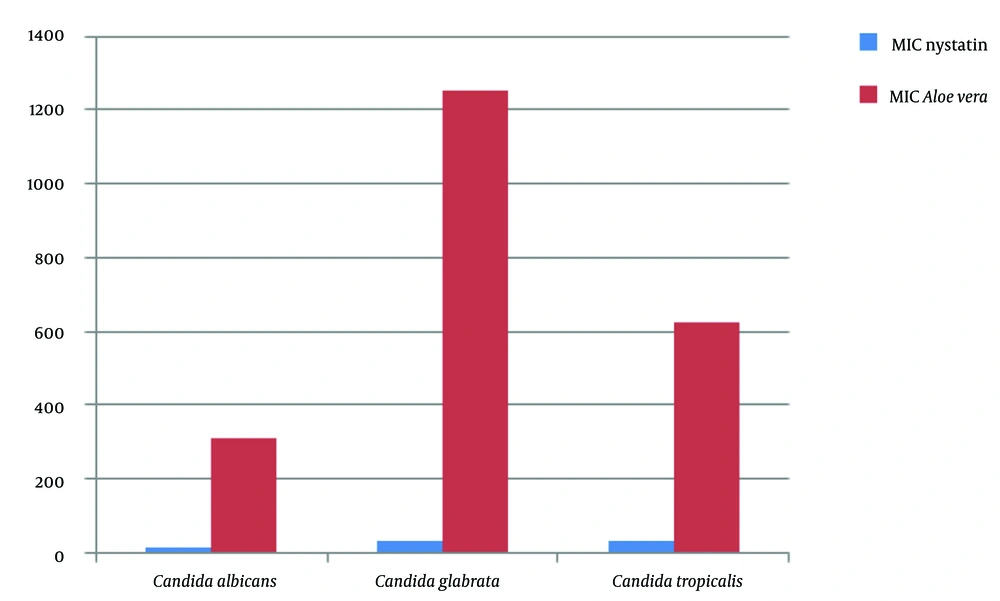
The inhibitory effect on all Candida subspecies was observed when assessing the plate MICs of Aloe vera gel. The inhibition of C. albicans growth was observed at 312.5 μL/mL and higher concentrations. Moreover, in the lower concentrations, fungal growth was detected in all media wells. C. glabrata and C. tropicalis showed higher resistance against the extract and could grow at concentrations higher than the inhibitory concentration of C. albicans. The inhibitory concentrations were 1250 and 625 μL/mL for C. glabrata and C. tropicalis, respectively (Table 1).
| No. | MIC | MIC Level | |
|---|---|---|---|
| Candidaalbicans | 11 | 312.5 μL/mL | 32 |
| Candida glabrata | 11 | 1250 μL/mL | 8 |
| Candida tropicalis | 11 | 625 μL/mL | 16 |
Inhibitory Concentrations of Aloe vera Extract
4.2. Nystatin
When assessing the plate MICs of nystatin, it was observed that the growth of all three subspecies was inhibited in various concentrations. The inhibitory concentration was 15.5 μL/mL for C. albicans, which occurred at 1:64. The inhibitory concentration was also 31.2 μL/mL for C. glabrata and C. tropicalis, which occurred at 1:32 (Table 2).
| No. | MIC | MIC Level | |
|---|---|---|---|
| Candida albicans | 11 | 15.5 μL/mL | 64 |
| Candida glabrata | 11 | 31.2 μL/mL | 32 |
| Candida tropicalis | 11 | 31.2 μL/mL | 32 |
Inhibitory Concentrations of Nystatin
4.3. Comparison of Aloe vera Gel and Nystatin
By comparing the two groups, a significant relationship was observed between the nystatin and Aloe vera extract groups, and both compounds had the inhibitory ability but at different concentrations (Figure 1).
5. Discussion
The study results showed that Aloe vera gel could inhibit the growth of understudy fungi. This study assessed three fungal subspecies of C. albicans, C. glabrata, and C. tropicalis. The inhibitory concentration of C. albicans was 312.5 μL/mL for Aloe vera gel. The inhibitory concentrations of C. albicans were also 1250 and 625 μL/mL for C. glabrata and C. tropicalis, respectively. The inhibitory concentrations of C. albicans, C. glabrata, and C. tropicalis for nystatin were 15.5, 31.2, and 31.2 μL/mL, respectively.
By comparing the two understudy groups, a significant relationship was observed between nystatin and Aloe vera gel groups, and both compounds had the inhibitory ability but at different concentrations. In a study, Taheri Bonab aimed to assess the antifungal effects of Aloe vera and honey compound on C. albicans and compare them to those of nystatin in vitro and examine the standard subspecies of C. albicans and bacterial count. The results of the aforementioned study showed that the MIC of Aloe vera and honey compound was 300 mg/mL for C. albicans. The results also confirmed the excellent inhibitory effect and bacterial susceptibility of Gram-negative bacteria and Enterococcus faecalis to Aloe vera and honey compound; however, the aforementioned effects were less substantial on C. albicans and increased with concentration. Taheri Bonab proposed 300 mg/mL as the concentration that significantly inhibits Candida growth. The results of Taheri Bonab’s study are consistent with the results of the present study, which can be attributed to using the standard C. albicans subspecies and similar methods (17).
Nalin Pagi and Payal Patel, who conducted a study aimed at evaluating the antimicrobial potential and phytochemical analysis of Aloe barbadensis Miller leaves extract, stated that the growth of all understudy fungi was inhibited by the Aloe barbadensis Miller leaves extract, which is consistent with the results of the present study (18). Bernardes showed in his study that a solution of 10% Aloe vera extract could inhibit the growth and germ tube formation by C. albicans (8). In another study by Bajwa et al. aimed at assessing the antifungal activity of Aloe vera stem extract, it was shown that the aqueous extract obtained from Aloe vera extract inhibited the growth of all three understudy subspecies. Although the subspecies studied by Bajwa et al. are different from those of the current study, in general, both studies highlighted the antifungal effects of Aloe vera extract, and the aforementioned study confirmed this finding (19).
Aggary et al. conducted a study that aimed to compare the antimicrobial effects of Aloe vera gel and leaves against Staphylococcus aureus, Pseudomonas aeruginosa, Trichophyton mentagrophytes, T. schoeleinii, Microsporum canis, and C. albicans. The antimicrobial susceptibility test showed that both gel and leave extract inhibit the growth of S. aureus. Only the gel inhibits the growth of T. mentagrophytes (20.0 mm); nevertheless, the leaves extract had inhibitory effects on P. aeruginosa and C. albicans (11).
There were several limitations in the present study, such as the high costs of preparing used herbal ingredients and other materials. Aloe vera was only used in gel form, and extraction methods for its preparation were not employed. Moreover, this study suggests evaluating the antibacterial efficacy of Aloe vera gel against clinical species instead of standard ones in future studies.
5.1. Conclusions
Given the study results, it could be stated that Aloe vera gel exhibited antifungal effects on all the understudy subspecies. The inhibitory concentrations of Aloe vera gel were much higher than nystatin. Therefore, to use this extract for humans, human toxic concentration should be estimated to minimize potential harm.