1. Background
Knee osteoarthritis (OA) is the most common type of degenerative joint disease leading to physical disability, particularly among middle-aged and elderly individuals (1). Approximately 3.6% (250 million) of the world population have knee OA, and this figure is projected to upsurge in the coming years due to the aging population and the growing prevalence of obesity coupled with the increasing numbers of joint injuries (2). The impact of knee OA is complex as it leads to pain (3), walking‐related disability (4), poor life quality, and substantial economic costs (5).
Most large-scale studies on the prevalence and pattern of knee OA have been conducted in developed countries (6, 7), and limited information is available from less developed countries. The prevalence of knee OA in Nigeria has been reported to be 16.3% in individuals ≤ 30 years old (8) and 19.6 – 20.6% in individuals ≥ 40 years old (8, 9). These correspond with the prevalence rates of 19.2 – 27.8% in ≥ 45 years old and 37.4% in ≥ 60 years old reported for developed countries (10). Consistent with the reports from developed countries (11, 12), the occurrence of knee OA in Nigeria is believed to be multifactorial, with many risk factors such as advanced age, female gender, overweight, knee extensor weakness, knee misalignment, and knee injuries (13-15). With the rising prevalence of knee OA in Nigeria, effective short- and long-term treatment strategies are desirable to tackle this disease.
It is well-documented that individuals with advanced age and knee OA exhibit proprioceptive acuity (ie, joint position sense and joint movement sense [kinesthesia]) deficits (16-18). These proprioceptive deficits may predispose to pain and disability (19, 20). Consequently, interventions targeting to reduce knee proprioceptive deficits may improve dynamic joint stability while reducing pain and functional disability. Proprioceptive exercise in the form of kinesthesia, balance and agility (KBA) is a relatively new intervention in the rehabilitation of knee OA. Initially designed to rehabilitate and prevent knee ligamentous injury and ankle instability, KBA is designed for individuals with knee OA to enhance knee proprioceptive accuracy using a series of balance and walking-based agility exercises to stimulate, challenge, and adapt the proprioceptors of the nervous system (21, 22).
Although KBA exercises appear to be a valuable treatment for patients with knee OA (21-24), the appropriate treatment dosage to achieve the highest effectiveness is yet to be clarified, owing to the mixed findings of available studies. For example, in two randomized controlled trials (RCTs) conducted by Roger et al. (21, 22), thrice-weekly KBA plus resistance exercise was not better than resistance exercises alone for physical function when interventions were administered for eight weeks. However, in another RCT (23) with a similar treatment, superior results were observed with the addition of KBA to resistance exercises compared to resistance exercises alone. In another vein, Fitzgerald et al. (24) found no additional benefit in physical function with the addition of twice-weekly KBA to resistance exercises compared to resistance exercises alone when the interventions were applied for 6-8 weeks. On the contrary, a 6-week, twice-weekly KBA program significantly improved pain and functional capacity compared to non-treatment (25). Additionally, most prior studies (22–24) compared KBA program with resistance exercise program, and comparison with standard or conventional physical therapy is limited.
In light of the foregoing, it is unclear as to the appropriate KBA exercise dosage in terms of weekly application that may produce greater outcomes. Therefore, we plan to conduct a large-scale RCT to determine the effectiveness of different weekly applications of KBA among individuals with knee OA. However, before conducting any large, definitive trial, it is worth of conducting a pilot trial to assess feasibility to avoid waste of resources (26, 27).
2. Objectives
This pilot study was conducted to determine the feasibility of a large-scale RCT to examine the effectiveness of different weekly applications of KBA among individuals with knee OA.
3. Methods
3.1. Study Design
A single-blind (assessor), randomized controlled pilot trial was conducted at the Physical Therapy Department, Murtala Muhammad Specialist Hospital (MMSH), Kano State, Nigeria.
3.2. Ethical Consideration
The Health Research Ethics Committee of the Ministry of Health, Kano State, Nigeria, approved this trial (Ref: MOH/Off/797/T.I./600). It was registered with the Pan African Clinical Trials Registry (PACTR201810713260138; 28 November 2017). All participants signed written informed consent before recruitment.
3.3. Participants
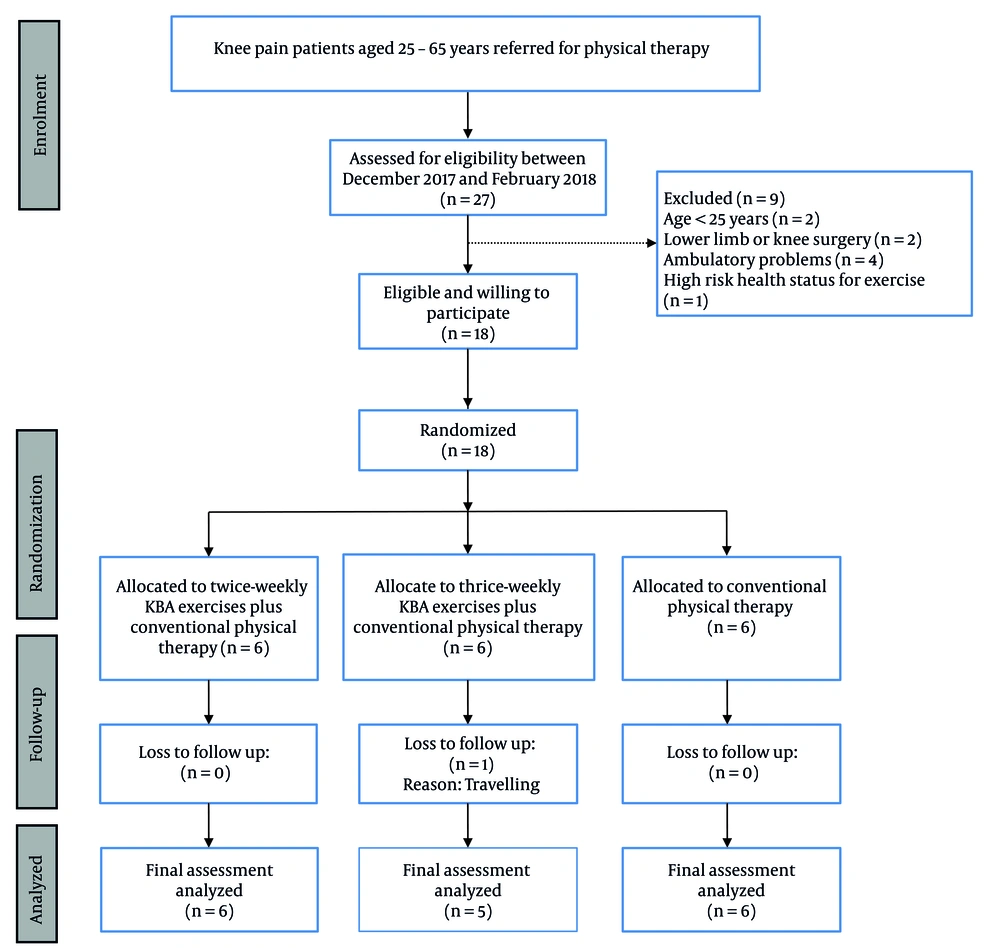
The study population included individuals with symptomatic knee OA referred to MMSH for physical therapy by physicians or orthopedists. The inclusion criteria were males or females aged 25 - 65 years and unilateral or bilateral knee OA meeting at least three of the American College of Rheumatology (ACR) clinical classification criteria (28). Patients were excluded if they had a history of lower limb joint surgery, obvious lower limb deformity, rheumatic disease other than OA, ambulatory problems, assistive device use for ambulation, balance or neurological disorder affecting lower limbs, peripheral vascular disease, and visual problems. The overall trial flow is outlined in Figure 1.
Before the beginning of the study, three physical therapists with two to five years of experience in musculoskeletal physical therapy were recruited for the study. One of the physical therapists was responsible for eligibility and outcome assessments. The other two physical therapists and the primary investigator (AIA) were responsible for the treatment. All the therapists were given one-on-one instruction on the study procedures by the primary investigator to standardize the intervention.
3.4. Sample Size and Randomization
We did not perform a formal sample size calculation for this pilot study. However, 18 participants were recruited to assess the feasibility. Following baseline assessments, the participants were randomly assigned to three study arms of six participants: Twice-weekly KBA, thrice-weekly KBA, and control (conventional physical therapy) by picking sealed, stamped envelopes from a black bag with letters 'A', 'B' or 'C' corresponding to the three study arms. The bag contained only 18 envelopes to allow restricted randomization. A recording officer performed the randomization at the study center. The outcome assessor was blinded to group assignment.
3.5. Outcome Assessments
3.5.1. Recruitment Rate
The recruitment rate was considered acceptable when at least 50% of the participants fulfilling the eligibility criteria were enrolled within the recruitment period (eight weeks).
3.5.2. Retention/Dropout Rate
The retention rate was considered acceptable when 50% of the consented participants completed their treatment sessions (29). The dropout rate was the number of participants lost during the study.
3.5.3. Adverse Events
Serious adverse events are not commonly reported with exercise interventions. However, the participants were told before the interventions to report any serious adverse events, eg, aggravating knee joint pain, evident knee joint swelling, and extreme fatigue, to the primary investigator or any of the physical therapists for further action.
3.5.4. Knee Pain
The Visual Analog Scale for pain (VAS-pain) was used to assess the participants' perception of knee pain. It consisted of a 100 mm bidirectional line with anchor statements "no pain" (0 mm) on the left and "worst possible pain" (100 mm) on the right (28). Participants were instructed to rate their current perceived level of knee pain. The Hausa version of the VAS-pain was validated (30, 31) and used in this study.
3.5.5. Physical Function
The Ibadan Knee and Hip Osteoarthritis Outcome Measure (IKHOAM) developed by Odole et al. (32) was used to assess the participants' physical function. It consisted of 33 items with three main domains: Activity limitations, participation restrictions, and physical performance tests. The items were rated on a Likert scale ranging between 0 and 5. Scores obtained were divided by the total possible scores (ie, 232) and multiplied by 100 to obtain the participant’s perceived level of physical function, with higher scores indicating higher levels of physical function (32). The Hausa version of the IKHOAM was validated (32, 33) and used in this study. Both pain and physical function were assessed at baseline and six weeks post-intervention.
3.6. Interventions
Participants allocated to the conventional physical therapy group received a brief education program, followed by ultrasound therapy and then stretching and strengthening exercises. Treatment was administered twice weekly, except for the education program administered for only two sessions. Participants allocated to the twice-weekly KBA group received two sessions per week of KBA, and those allocated to the thrice-weekly KBA group received three sessions per week of KBA. Participants in the twice-weekly KBA and thrice-weekly KBA groups also received conventional physical therapy in addition to the KBA program assigned to each group. All groups were treated for six weeks. All lower-extremity exercises were completed bilaterally. The exercises were delivered individually under supervision. All participants were encouraged to perform exercises at least twice per day at home. However, exercises necessitating the strict supervision of the therapist were not encouraged as a component of the home exercise program. An exercise leaflet was given to all participants to guide their home program and encourage adherence.
3.6.1. Conventional Physical Therapy
Brief education was provided in a group, and the following topics were discussed: (A) physiological mechanism of knee OA, (B) lifestyle modification and importance of physical activity, (C) diet and weight control, (D) self-management skills, and (E) knee joint ergonomics and protection. The education session lasted for approximately 15 - 20 minutes. Ultrasound therapy was then administered to the patients' affected knees using the direct contact technique with ultrasonic gel as an acoustic coupling medium. The treatment parameters used were frequency = 1.0 MHZ, pulse rest time = 1:1, intensity = 2.0 W/cm2, and treatment time = 7 minutes (34). Thereafter, three stretching exercises (supine hamstring stretch, side-lying quadriceps stretch, and towel calf stretch) were performed as a warm-up. Each exercise was held for 15 seconds and repeated six times, with rest periods of 6 - 10 seconds between exercises. The same stretching exercises were also completed as cool down after performing strengthening exercises. Similar to the stretching, each strengthening exercise (static quadriceps isometrics, seated knee extension, and lying leg curl) was held for 15 seconds and repeated six times, with rest periods of 6 - 10 seconds between exercises. The participants were also encouraged to perform an aerobic exercise program (eg, continuous outdoor walking or biking) at tolerable speed for 20 - 30 minutes a day for at least 3 - 4 days per week at home. The entire program lasted for approximately 30 minutes per session.
3.6.2. Kinesthesia, Balance and Agility Exercises
The KBA protocol used in this study was identical to that described in previous trials (21, 22, 35), with slight modifications regarding the training intensity (number of sessions) in addition to the introduction of visual manipulation for some specific walking-based agility exercises (Table 1). All agility-based exercises were conducted before progressing to balance exercises. For the balance exercises, the participants performed static and dynamic balance exercises with eyes open and then closed by standing on a hard surface and then standing on a soft surface. While encouraging the patients to maintain balance with bilateral limbs, the physical therapist perturbed the patients in a different direction to stimulate neuromuscular mechanisms. Exercises were progressed based on the patient's tolerance and abilities. The entire KBA exercise program lasted approximately 30 - 40 minutes per session. Table 1 shows the detailed descriptions of KBA exercises.
| Progression, Exercise | Treatment Intensity |
|---|---|
| Week 1 - 2 | |
| Sidestepping | 15 - 75 steps × 3 sets |
| Semi-tandem walk | √ |
| Tandem walk | √ |
| Crossbody leg swings | √ |
| Crossover forward walk | √ |
| Crossover backward walk | √ |
| Week 3 - 4 | |
| Toe walk | 10 - 30 seconds × 3 sets |
| Heel walk | √ |
| Multiple changes of direction drills | √ |
| One-leg stand on a hard surface with eyes open | √ |
| One-leg stand on a hard surface with eyes closed | √ |
| Double-leg stand (eyes open) on a hard surface with perturbations | √ |
| Double-leg stand (eyes closed) on a hard surface with perturbations | √ |
| Week 5 - 6 | |
| Crossover forward walk with eyes closed | 15 - 75 steps × 3 sets |
| Crossover backward walk with eyes closed | √ |
| One-leg stand on a foam surface with eyes open | 10 - 30 seconds × 3 sets |
| One-leg stand on a foam surface with eyes closed | √ |
| Double-leg stand (eyes open) on a foam surface with perturbations | √ |
| Double-leg stand (eyes closed) on a foam surface with perturbations | √ |
Kinesthesia, Balance and Agility Exercises
3.7. Statistical Analysis
Descriptive statistics such as the mean (standard deviation, SD) and frequency (percentage) were used to summarize the data, including feasibility outcomes, as appropriate. Shapiro-Wilks test was used to check the normality of the data. One-way ANOVA and Fisher’s exact test were used for baseline comparison among the groups. A 3 × 2 (treatment group × time) mixed-model ANOVA was used to analyze the treatment effect on pain and physical function. Bonferroni correction was applied for pairwise comparison for any significant ANOVA. Effect size was computed using partial eta squared (ηp2) and rated as small (0.2), moderate (0.5), and large (0.8) effect (36). For each outcome, percentage of change relative to baseline was calculated. All data analyses were conducted in SPSS version 23.0 (IBM Corp., Armonk, NY., USA) with a statistical significance level of P < 0.05.
4. Results
4.1. Characteristics of Participants
The participants’ age and body mass index were 47.5 ± 9.84 years and 29.5 ± 4.37 kg/m2, respectively. The majority of the participants were female (95%), full-time housewives (70%), and had tertiary education. The left knee was the most commonly affected joint (66.6%). The participants were comparable in all demographic variables, as no statistically significant differences were found between the three groups (P > 0.05). The demographic characteristics of the participants are shown in detail in Table 2.
| Variables | Twice-KBA (N = 6) | Thrice-KBA (N = 6) | Conventional Physical Therapy (N = 6) | P-Value |
|---|---|---|---|---|
| Age (y) | 45.3 ± 11.3 | 42.3 ± 8.59 | 54.8 ± 5.07 | 0.062 b |
| Height (m) | 1.65 ± 0.66 | 1.63 ± 0.41 | 1.59 ± 0.97 | 0.313 b |
| Weight (kg) | 76.3 ± 14.6 | 83.5 ± 10.1 | 75.5 ± 15.1 | 0.541 b |
| BMI (kg/m2) | 27.7 ± 4.70 | 31.2 ± 3.39 | 29.7 ± 4.91 | 0.414 b |
| Gender | 0.347 c | |||
| Male | 1 (10.0) | 0 (0.0) | 0 (0.0) | |
| Female | 5 (90.0) | 6 (100.0) | 6 (100.0) | |
| Limb affected | 0.792 c | |||
| Right | 2 (20.0) | 3 (50.0) | 2 (20.0) | |
| Left | 4 (80.0) | 3 (50.0) | 4 (80.0) | |
| Marital status | 0.570 c | |||
| Married | 5 (83.3) | 5 (83.3) | 6 (100.0) | |
| Single | 1 (16.7) | 1 (16.7) | 0 (0.00) | |
| Educational status | 0.512 c | |||
| None | 1 (16.7) | 0 (0.00) | 3 (50.0) | |
| Completed primary | 1 (16.7) | 2 (33.3) | 1 (16.7) | |
| Completed secondary | 1 (16.7) | 1 (16.7) | 0 (0.0) | |
| Completed tertiary | 3 (50.0) | 3 (50.0) | 2 (33.3) | |
| Occupational status | 0.308 c | |||
| Civil servant | 2 (33.3) | 3 (50.0) | 0 (0.0) | |
| Self-employed (business/trading) | 2 (33.3) | 2 (33.3) | 2 (33.3) | |
| Housewife | 2 (33.3) | 1 (16.7) | 4 (66.7) |
Demographic Characteristics of the Participants a
4.2. Outcomes
4.2.1. Recruitment Rate
Twenty-seven individuals were assessed for eligibility between December 2017 and February 2018, of which, 18 fulfilled the eligibility criteria, representing a recruitment rate of 66.6%.
4.2.2. Retention/Dropout Rate
The retention rates in the twice-weekly KBA, thrice-weekly KBA, and conventional physical therapy groups were 100%, 83.3%, and 100%, with a corresponding dropout rate of 0%, 16.6%, and 0%, respectively.
4.2.3. Adverse Events
None of the participants in any group reported serious adverse events during or after the completion of the study.
4.2.4. Knee Pain and Physical Function
Mixed-model ANOVA revealed a significant within-group or time effect on VAS-pain ([1, 17] = 22.17, P = 0.001, and ηp2 = 0.61) and IKHOAM ([1, 17] = 7.933, P = 0.014, and ηp2 = 0.362) (Table 3). Bonferroni correction showed a significant decrease in the VAS-pain scores in all the groups from baseline to six weeks post-intervention (P < 0.05). For IKHOAM, Bonferroni correction showed a significant increase in the IKHOAM scores in both the twice-weekly KBA and thrice-weekly KBA groups from baseline to six weeks post-intervention (P < 0.05). However, no significant increase in the IKHOAM scores was observed for the conventional physical therapy group (P > 0.05).
There was no significant group-by-time interaction effect for both VAS-pain and IKHOAM (P > 0.05), indicating that the changes in these outcomes were equal between the three groups (Table 3). Similarly, the between-group effect was not statistically significant in all of the clinical outcomes evaluated (all P > 0.05), indicating no differences between the groups at baseline and six weeks post-intervention (Table 3).
| Groups | Baseline (Mean ± SD) | 6 Weeks (Mean ± SD) | Δ Relative to Baseline (%) | Within-Group Effect | Interaction Effect (Treatment Group × Time) | Between-Group Effect | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | ηp2 | P-Value | F | ηp2 | P-Value | F | ηp2 | P-Value | ||||
| VAS-pain | 22.17 | 0.612 | 0.001* | 0.966 | 0.121 | 0.404 | 0.662 | 0.086 | 0.531 | |||
| KBA (2x) | 6.83 ± 2.13 | 3.83 ± 1.94 | ↓ 43.9 | |||||||||
| KBA (3x) | 5.80 ± 3.34 | 3.20 ± 1.09 | ↓ 44.8 | |||||||||
| CPT | 4.91 ± 2.01 | 3.50 ± 0.83 | ↓ 28.7 | |||||||||
| IKHOAM | 7.933 | 0.362 | 0.014** | 2.984 | 0.229 | 0.083 | 1.593 | 0.185 | 0.238 | |||
| KBA (2x) | 68.3 ± 9.51 | 85.5 ± 4.61 | ↑ 25.1 | |||||||||
| KBA (3x) | 77.4 ± 17.6 | 95.0 ± 4.63 | ↑ 22.7 | |||||||||
| CPT | 80.8 ± 9.00 | 79.0 ± 11.4 | ↑ 2.22 | |||||||||
Evaluation of Clinical Outcome Parameters Before and After Intervention Among Treatment Groups Using Mixed-model Analysis of Variance a
5. Discussion
This pilot trial determined the feasibility of a large-scale RCT on the effectiveness of different weekly applications of KBA exercises among knee OA individuals. The results suggest the feasibility for recruitment and retention of participants, acceptability of the trial intervention, and promising effects of the intervention in terms of enhancing physical function.
The recruitment rate (66.6%) recorded in the current study is encouraging, as more than 50% of the eligible participants were recruited within the expected recruitment period. However, this percentage is somewhat low to anticipate a high recruitment rate in large-scale trial. Thus, additional study settings and longer recruitment periods may be required to achieve an adequate sample size for the future large-scale trial. Interestingly, the retention rates in all the three study groups (90 - 100%) were excellent. Only one participant (16.6%) was lost to follow-up in the thrice-weekly KBA group. However, this finding should be interpreted with caution due to the small sample size and short nature of the study. Overall, the excellent retention rates and absence of any adverse events suggest acceptability of the interventions.
In the present study, the studied participants appeared to be homogenous, as no significant clinical and demographic variables were observed between the groups at baseline. The participants were predominantly females and full-time housewives. The finding that the participants were mainly females is in line with the common finding that OA is highly prevalent among females (37). Additionally, the left knee was the most commonly affected joint, and none of the participants had bilateral affectation.
No cure is available for OA, and current treatment approaches for knee OA focus on reducing pain, physical disability, and disease progression (38). The existing treatment guidelines for knee OA consistently recommend education, instruction on self-management, exercise, weight loss (for overweight individuals), and thermal modalities as the first-line treatment (39). In the present study, improvement in perceived knee pain was observed in all the groups after intervention with a moderate effect size. This suggests that all the intervention strategies were promising in ameliorating knee pain, which is one of the most important outcomes in knee OA. Although compared to the conventional physical therapy group (28.7%), greater pain reduction was observed in the thrice-weekly KBA group (44.8%) followed by the twice-weekly KBA group (43.7%) post-intervention, no statistically significant difference was observed between the groups. The lack of significant between-group difference particularly between the two KBA groups could be due to the short-term nature of the interventions. Thus, a longer study period (> 6 weeks) and follow-up may yield different results. Nevertheless, a similar short-term program (six weeks, twice per week) of KBA resulted in significant improvement in perceived pain compared to no treatment control (25).
Regarding physical function, both the twice-weekly KBA and thrice-weekly KBA groups significantly improved after intervention with a moderate effect size. However, patients in the conventional physical therapy group did not improve. This implies applying KBA twice or thrice KBA weekly may be the appropriate dosage to achieve the highest effectiveness of the KBA program for physical function in persons with knee OA. However, given that the twice-weekly KBA group seems to enhance physical function (25.1%) better than the thrice-weekly KBA group (22.7%) even though the difference was not statistically significant, the former may be cost-efficient. Still, considering the short treatment sessions in the present study, definitive conclusions cannot be made until tested in a large, full-scale high-quality RCT. Consistent with our study, Fitzgerald et al. (24) did not observe superior improvement in physical function with twice-weekly combined KBA and resistance exercise compared to resistance exercise when the interventions were applied for six to eight weeks. In contrast, Diracoglu et al. (23) found significant improvement in physical function with the addition of thrice-weekly KBA to resistance exercise compared to resistance exercise alone when the interventions were applied for eight weeks. The variation in results across studies could be partly explained by the variation in the frequency and duration of KBA program application.
Though the present study is generally promising and suggests the feasibility for a full-scale trial in the future, some limitations are evident that should be considered when interpreting the study results. First, the study was limited by the small sample size and lack of power calculation, which is crucial to detect treatment effects between intervention arms. Second, the study period was short (six weeks), which might not allow the detection of significant treatment effects. Lastly, we did not conduct a qualitative interview to assess the acceptability of the KBA program based on the subjective opinions of the participants. However, since our study is a pilot trial, the aforementioned limitations will be addressed in a future large-scale RCT. Moreover, other aspects worth to be addressed include the need to improve the recruitment rate probably by recruiting patients from other hospitals and extending the duration of the recruitment period, and assessment of other important outcome measures such as knee stability, proprioception, and quality of life.
In conclusion, this study suggests the feasibility of a large-scale RCT to examine the effectiveness of different weekly applications of KBA exercises among knee OA individuals, with minor amendments.