1. Background
In December 2019, an increasing number of viral severe acute respiratory syndrome (SARS) cases was reported from Wuhan, China (1). The World Health Organization (WHO) called the disease COVID-19, which has been spreading worldwide since then. More than 180 million confirmed cases were reported from 220 countries, and it is estimated that 6 million people died because of COVID-19 until April 2022 (2). According to the reports, more than 7 million COVID-19 cases and 140,000 deaths have been recognized in Iran (3).
Global public health campaigns started to develop preventive guidelines that recommended quarantine, face masks, and social distancing to reduce the virus spread (4). Governments have been making efforts to stop or reduce the spreading of COVID-19. However, there is insufficient information about this disease. It has been observed that people do not practice COVID-19 preventive measures well due to several reasons such as false beliefs about health, inaccessibility to personal protective equipment like face masks, high costs of living, cultural beliefs, and unsupportive governments (5). Smith et al. conducted a study in England. They reported that 75.1% of participants had left their homes 24 hours before the interview, which implies ignoring the enforced quarantine protocols by people (6).
COVID-19 brings about several physical and mental health problems (7). It is crucial to highlight the importance of practicing COVID-19 preventive measures (8). In order to control the virus spread, people are supposed to cooperate with the government and society by changing some of their behaviors and traits (9). If people refuse to adapt to the new situation and continue ignoring preventive measures, the spread of the disease may result in a crisis leading to an inefficient health system (10). It is assumed that empathy, trust in science, and personality traits are among the factors determining how much people adhere to practicing COVID-19 preventive measures (11). Despite the efforts, some people continue ignoring COVID-19 preventive measures (12). Many cases of young people and adults have been observed worldwide ignoring the preventive measures (13). While medical information about the severity of COVID-19 and virus transmission methods has been updated, social and psychological responses of people to this issue have remained unknown (14). People have their reasons for practicing or ignoring COVID-19 preventive measures. Thus, it is crucial to investigate barriers and facilitators to practicing the measures. Plohl and Musil designed an instrument to investigate people's behaviors and the extent to which they adhere to practicing COVID-19 preventive measures in Slovenia (12). Regarding cultural differences, it is essential to design and develop instruments according to the cultural norms of each society.
2. Objectives
Since no similar instrument has been developed in Iran, the present study aimed to design one to identify barriers and facilitators to practicing COVID-19 preventive measures.
3. Methods
This is a methodological study attempting to develop and evaluate the psychometric properties of an instrument to identify barriers and facilitators to practicing COVID-19 preventive measures in Sanandaj city, Iran. The questionnaire was designed and developed according to the following steps.
In the first phase of the study, COVID-19 preventive measures were explained to some residents of Sanandaj city. A total of 20 participants were selected through the purposive sampling method. The sampling process continued until data saturation was achieved. Deep and unstructured interviews were conducted for data gathering. The participants discussed their experiences regarding barriers to practicing COVID-19 preventive measures. Each interview lasted for about 30 to 90 minutes. The interviews were then recorded and transcribed. The data was analyzed through conventional content analysis. The scripts were reviewed several times for immersion and a holistic data view and then reviewed carefully to extract codes. This process continued until all codes were extracted. Afterward, the codes were classified according to their similarities and differences. Finally, the categories were assigned as statements or items of the questionnaire. Meanwhile, more statements were extracted from the related literature (12) and added to the questionnaire. The researchers asked the developer of the COVID-19 preventive guidelines for permission. The final version of the questionnaire was developed based on the related literature review and qualitative phase of the study.
In the second phase of the study, the validity of the questionnaire was investigated through face, content, and construct validity investigation. Face validity was initially investigated (15) by interviewing ten people. Level of difficulty (understanding words and phrases), relevancy (relevancy of phrases to the questionnaire aspects), as well as ambiguity (probability of false understanding due to ambiguous words and phrases) were investigated. The researchers attempted to write logical and grammatically correct sentences to develop statements of the questionnaire. The statements were reviewed several times by the research team, and corrections were made. Then, two Farsi (Persian) language experts reviewed and reconsidered the questionnaire.
Validity was investigated through qualitative and quantitative approaches. Experts with sufficient knowledge and experience in nursing, health, and instrument design investigated content validity. The researchers asked 20 experts to feedback on the questionnaire qualitatively in terms of grammar, wording, item allocation and scaling. The content validity ratio (CVR) and the content validity index (CVI) were applied to investigate content validity quantitatively. In order to investigate CVR, the researchers asked 20 experts to scale each item on a three-level Likert scale (significant, helpful but not significant, and not significant). According to the Lawshe content validity ratio table, items with a ratio of 0.42 were reserved and considered meaningful and statistically significant (P < 0.05) (16). Afterward, the researchers asked the experts to determine the relevancy, simplicity, and clarity of each item of the questionnaire according to Waltz and Bausell's content validity index. Thus, three indices of simplicity, relevancy, and clarity were scaled on a four-level Likert scale, and each item was considered by each expert individually. For instance, for the relevancy index, the following levels were scaled: not relevant, fairly relevant, relevant, and quite relevant. The CVI score for each item was calculated by dividing the number of experts scaling an item showing 3 or 4 levels of agreement to the total number of experts (17). Hyrkas et al. recommended scores above 0.79 for accepting the CVI of each item (18). In the next stage, the average CVI (S-CVI/Ave) score was calculated according to the average CVI score of all items of the questionnaire. Polit et al. recommended scores above 0.90 for desired S-CVI/Ave (17).
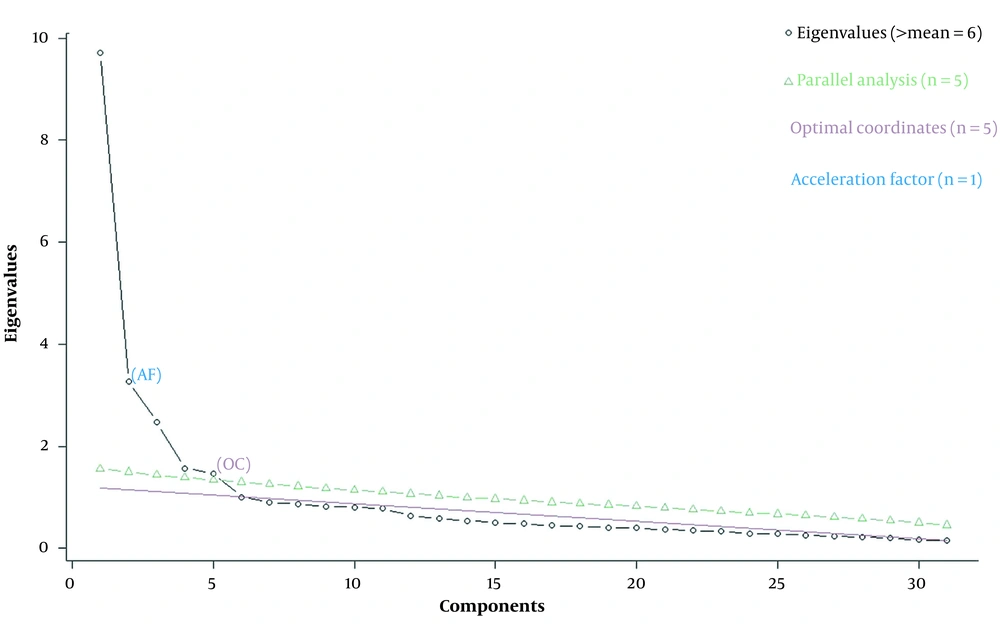
Exploratory factor analysis was applied to investigate construct validity (19). After examining the internal consistency of the items, exploratory factor analysis was performed to determine the correlation among the variables to explore variable categories with the highest correlation. Exploratory factor analysis is a crucial step required to be taken in designing new instruments (20). Exploratory factor analysis was done using STATA and R softwares through the principal-component factors method, the scree test, and Varimax-rotated factor loadings. The required samples for each item are estimated at 5 to 10 (21). In the present study, sampling was done among residents of Sanandaj city, and the number of samples was ten times more than the number of questionnaire items.
In the last phase of the study, Cronbach's alpha was used to determine the internal consistency and reliability of the questionnaire. Cronbach's alpha demonstrates the internal consistency of a group of items assessing a construct. A Cronbach's alpha coefficient of 0.7 - 0.8 is considered a desired internal consistency (22). Ultimately, 300 participants were selected from among residents of Sanandaj city through purposeful sampling.
3.1. Ethical Considerations
The present study was considered and confirmed by the Ethics Committee and Research Committee of the Clinical Care Research Center at Kurdistan University of Medical Sciences (No. IR.MUK.REC.1399.073). The participants were informed about the aim and significance of the study and participated voluntarily. Also, the participants’ consent was obtained for recording the interviews, and they were assured that the data would be merely used for research purposes and that only the research team would access the data. Moreover, the participants were informed that they could quit the research process at any time and that their information would remain confidential during the research process.
4. Results
After analyzing the qualitative data, three categories of adherence to practice, barriers (false beliefs, being pressured, and carelessness), and facilitators (awareness, fear, commitment, union against the disease, and alert) appeared.
In the first phase of the study, initial items concerning practicing preventive measures by the people of Sanandaj city were elicited through conducting qualitative interviews and reviewing the related literature. In this phase, two main categories, eight categories, and 25 sub-categories were organized based on the 257 extracted initial codes. Afterward, 24 items (questions) were developed from the sub-categories, and seven more items were added after reviewing the related literature. At last, 31 items were classified into three categories of adherence to practice, barriers, and facilitators. Then, the phrases were written as equivalent items (economic challenges causing less commitment to practicing preventive guidelines; fear of the disease and its consequences enforcing more commitment to practicing preventive guidelines). The research team reviewed the items in three different sessions. The items were then given to 20 experts and ten residents of Sanandaj city for further consideration concerning the comprehensiveness of the items. The recommended corrections were applied.
In the next phase, the instrument's content validity was analyzed by 20 experts in the realm of instrument analysis. Hyrkas et al. recommended scores above 0.79 for accepting the CVI of each item (18). Content validity indices of all the items were above 0.8. The panel included 20 experts, which is considered acceptable, and the calculated CVI for each item was 0.24 according to the Lawshe table. The CVR of the items was calculated at 0.7, according to the expert pane’s opinion. Therefore, none of the items was deleted. Then, the questionnaire was distributed among the 300 residents, and exploratory factor analysis was performed on 31 items. Exploratory factor analysis, done by STATA, demonstrated that six factors had more than one eigenvalue, the sum of which covered 62% of the information or variations. Then, all the factors were analyzed by R software and the scree test. The results showed that the top five factors with more than one eigenvalue were meaningful, and the total variance was 0.59 (Figure 1). The internal consistency of the items was investigated according to the five significant factors and through Varimax-rotated factor loadings in STATA software, and they were classified into five factors (Table 1): (1) adherence to practice (the first factor); (2) facilitators (the second factor); (3) barriers (the third factor); (4) facilitators of group 2 (the fourth factor); and (5) barriers of group 2 (the fifth factor).
| No. | Items | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 |
|---|---|---|---|---|---|---|
| 1 | I wash my hands or sanitize them with alcohol regularly. | 0.6559 | ||||
| 2 | I avoid touching my eyes, nose, and mouth. | 0.7004 | ||||
| 3 | When I cough or sneeze, I cover my mouth and nose with a tissue or my bent elbow. | 0.6111 | ||||
| 4 | I avoid participating in crowded meetings. | 0.7312 | ||||
| 5 | I adhere to social distancing. | 0.7366 | ||||
| 6 | I avoid infected people. | 0.6308 | ||||
| 7 | If I feel sick, I stay home (except for medical purposes). | 0.6664 | ||||
| 8 | Fear of transmitting the virus to others causes more adherence to the preventive guidelines. | 0.5759 | ||||
| 9 | Commitment to oneself causes more adherence to the preventive guidelines. | 0.7553 | ||||
| 10 | Commitment to family causes more adherence to the preventive guidelines. | 0.6356 | ||||
| 11 | Commitment to others and the community causes more adherence to the preventive guidelines. | 0.8038 | ||||
| 12 | A sense of collaboration among people for breaking the virus transmission chain leads to more adherence to the preventive guidelines. | 0.8012 | ||||
| 13 | A sense of collaboration among people to stop the virus spread leads to more adherence to the preventive guidelines. | 0.8126 | ||||
| 14 | Public education via media results in more adherence to the preventive guidelines. | 0.5708 | ||||
| 15 | Economic challenges cause ignoring preventive guidelines. | 0.6885 | ||||
| 16 | Disturbed life routines lead to ignoring preventive guidelines. | 0.8207 | ||||
| 17 | Impatience leads to ignoring preventive guidelines. | 0.7107 | ||||
| 18 | Unpreparedness for fighting against the disease causes ignoring preventive guidelines. | 0.6802 | ||||
| 19 | People's bias and opposition against the preventive guidelines lead to ignoring them. | 0.4635 | ||||
| 20 | Forgetfulness leads to ignoring preventive guidelines. | 0.6526 | ||||
| 21 | The hardship of practicing the guidelines leads to ignoring them. | 0.6286 | ||||
| 22 | Awareness of the mortality rate and other statistical information about the disease results in more adherence to the preventive guidelines. | 0.5781 | ||||
| 23 | Awareness of the disease's causes and symptoms leads to more adherence to the preventive guidelines. | 0.6081 | ||||
| 24 | Fear of the consequences of getting the disease causes more adherence to the preventive guidelines. | 0.8214 | ||||
| 25 | Fear of losing a family member or loved one leads to more adherence to the preventive guidelines. | 0.8243 | ||||
| 26 | Fear of death results in more adherence to the preventive guidelines. | 0.6463 | ||||
| 27 | False beliefs about the disease cause ignoring the preventive guidelines. | 0.7162 | ||||
| 28 | Wrong thoughts lead to ignoring the preventive guidelines. | 0.7525 | ||||
| 29 | Disbelief in the disease causes ignoring the preventive guidelines. | 0.8100 | ||||
| 30 | Carelessness and procrastination lead to ignoring the preventive guidelines. | 0.5319 | ||||
| 31 | Lack of commitment to the community and family results in ignoring the preventive guidelines. | 0.5817 |
Rotated Factor Loadings (Pattern Matrix) and Unique Variances
In the final phase of the research process, the questionnaire was distributed among the 300 residents, and Cronbach's alpha was calculated to determine its reliability. The first factor, adherence to practice, was scaled on a five-level Likert scale (always/usually/sometimes/rarely/never). The other factors were scaled on a five-level Likert scale (totally agree/agree/no idea/disagree/totally disagree). The Cronbach's alpha was 0.829 for the first factor (adherence to practice category including seven items) and 0.8374 for the second factor (facilitators including seven items). The calculated Cronbach's alpha for the third factor (barriers including five items), the fourth factor (facilitators of group 2 including five items), and the fifth factor (barriers of group 2 including five items) were 0.8374, 0.8639, and 0.8277, respectively. The total calculated Cronbach's alpha for all the 31 items was 0.9169 (Table 2). At last, concerning the similarities among items of the third and fifth factors (barriers of groups 1 and 2) and those of the second and fourth factors (facilitators of groups 1 and 2), the researchers decided to organize the final version of the questionnaire in three categories of adherence to practice, barriers, and facilitators of COVID-19 preventive measures. The items of the adherence to practice category were scaled on a five-level Likert scale as always, usually, sometimes, rarely, and never. The items of the barriers and facilitators categories were scaled on a five-level Likert scale as totally agree, agree, no idea, disagree, and totally disagree (Table 3).
| Cronbach’s Alpha; Factor 1 (Practice Items) | Cronbach’s Alpha; Factor 2 (Facilitators of Group 1) | Cronbach’s Alpha; Factor 3 (Barriers of Group 1) | Cronbach’s Alpha; Factor 4 (Facilitators of Group 2) | Cronbach’s Alpha; Factor 5 (Barriers of Group 2) | Total Cronbach’s Alpha |
|---|---|---|---|---|---|
| 0.8296 | 0.8913 | 0.8374 | 0.8639 | 0.8277 | 0.9169 |
The Reliability of the Factors
| No. | Items | Scale | ||||
|---|---|---|---|---|---|---|
| 1 | I wash my hands or sanitize them with alcohol regularly. | Always | Usually | Sometimes | Rarely | Never |
| 2 | I avoid touching my eyes, nose, and mouth. | Always | Usually | Sometimes | Rarely | Never |
| 3 | I avoid touching my eyes, nose, and mouth. | Always | Usually | Sometimes | Rarely | Never |
| 4 | I avoid participating in crowded meetings. | Always | Usually | Sometimes | Rarely | Never |
| 5 | I adhere to social distancing. | Always | Usually | Sometimes | Rarely | Never |
| 6 | I avoid infected people. | Always | Usually | Sometimes | Rarely | Never |
| 7 | If I feel sick, I stay home (except for medical purposes). | Always | Usually | Sometimes | Rarely | Never |
| 8 | Fear of transmitting the virus to others causes more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 9 | Commitment to oneself causes more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 10 | Commitment to family causes more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 11 | Commitment to others and the community causes more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 12 | A sense of collaboration among people for breaking the virus transmission chain leads to more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 13 | A sense of collaboration among people to stop the virus spread leads to more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 14 | Public education via media results in more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 15 | Economic challenges cause ignoring preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 16 | Disturbed life routines lead to ignoring preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 17 | Impatience leads to ignoring preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 18 | Unpreparedness for fighting against the disease causes ignoring preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 19 | People's bias and opposition against the preventive guidelines lead to ignoring them. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 20 | Forgetfulness leads to ignoring preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 21 | The hardship of practicing the guidelines leads to ignoring them. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 22 | Awareness of the mortality rate and other statistical information about the disease results in more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 23 | Awareness of the disease's causes and symptoms leads to more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 24 | Fear of the consequences of getting the disease causes more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 25 | Fear of losing a family member or loved one leads to more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 26 | Fear of death results in more adherence to the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 27 | False beliefs about the disease cause ignoring the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 28 | Wrong thoughts lead to ignoring the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 29 | Disbelief in the disease causes ignoring the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 30 | Carelessness and procrastination lead to ignoring the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
| 31 | Lack of commitment to the community and family results in ignoring the preventive guidelines. | Totally agree | Agree | No idea | Disagree | Totally disagree |
The Final Questionnaire
5. Discussion
The present study attempted to develop and test the psychometric properties of an instrument to identify barriers and facilitators to practicing COVID-19 preventive measures among residents of Sanandaj city. The questionnaire was designed in three categories: adherence to practice, barriers, and facilitators.
In this study, the psychometric properties of the instrument, such as the face, content, and construct validity as well as reliability, were investigated in Sanandaj city, Iran. The questionnaire had a content validity coefficient of 0.79, calculated according to Waltz and Bausell's content validity index, making it valid enough according to the instrument’s assessment purposes. Content validity is a crucial property of each newly developed instrument since the validity of the obtained data comes from the instrument's content validity (23). All the items were consistent with the total consistency score, implying the sufficient reliability of the instrument.
5.1. Adherence to Practice
Practicing preventive measures is recognized as one of the most important indices of controlling COVID-19 spread and guarantees public health during a pandemic. Reynolds et al. (24) discussed that women are more committed to practicing preventive measures than men. This might be caused by differences in their responsibilities. Since men are supposed to support and provide for the family, they must go out and work (25).
Fallahi et al. reported that the more people were aware of the consequences of COVID-19 disease, the more they seemed to be committed to practicing preventive measures (26).
5.2. Barriers
False beliefs, feeling of pressure, and carelessness have been recognized among the barriers to practicing preventive measures. On the other hand, awareness, fear, alertness, and union against the disease are facilitators to practicing preventive measures. Whenever a pandemic breaks out, unscientific opinions about the prevention and cure of the disease spread widely (27). People need scientific truth in the pandemic crisis to feel safe. If that need is not met, false ideas become interesting (28). False information and rumors spread fast on social media, which can affect the process of treatment (27, 29, 30). False beliefs about the COVID-19 pandemic started to spread in many countries in 2020. This trend caused a serious challenge, which persuaded the director-general of the World Health Organization (WHO) on February 15, 2020, to declare that "we are fighting against a pandemic and an epidemic of false information simultaneously. An important aspect of it is false information concerning the disease spread" (7).
Therefore, it is required to constantly provide society with comprehensive scientific and evidence-based information. Health information must be clear and confident, so that correct preventive and treatment measures are taken to protect people from anxiety, fear, and injury (31). Thus, correct information must be available through valid media. Simplicity should be considered in the information for the public, and false beliefs must be eliminated by an appropriate method compatible with the community.
One of the barriers is associated with the consequences of COVID-19 disease that cause too much pressure on people. Many people do not afford to purchase preventive equipment and practice the measures. They have to work to provide for their family. Some live in crowded and under-privileged neighborhoods, so they cannot adhere to social distancing (32). Hutt stated that while the world is dealing with the COVID-19 pandemic, the economic consequences of the disease are growing (33). The pandemic has also affected the workforce in the world; some employees do not go to work, and some are fired. For instance, some airline companies have asked their employees to take unpaid leaves or register in workforce adjustment programs (34). Therefore, people need to be supported by the government to survive and practice preventive measures during the COVID-19 pandemic.
Another recognized barrier to practicing COVID-19 preventive measures is unpreparedness. Crises typically cause tension in society. It seems that the authorities did not plan an appropriate program for raising public awareness of the crisis. They had no strategy or a coherent program for information management during the crisis. Ashrafi-Rizi, and Kazempour mentioned that one of the challenges of COVID-19 management was hesitancy and procrastination in publishing information, resulting in a lack of preparation for dealing with the pandemic (35).
The opposition has been identified as another crucial obstacle associated with adherence to preventive measures. Bavel et al. and Bonell et al. reported that one of the solutions to reduce people's opposition to preventive measures is publishing health messages that do not imply fear or obligation (36, 37).
5.3. Facilitators
The findings of Ashrafi-Rizi and Kazempour (35). are in line with the present study’s results. They showed that raising public awareness, publishing accurate information, and correct statistics about the disease resulted in more adherence to practicing preventive measures (38). It can be concluded that raising people's awareness by giving correct information at the right time facilitates adherence to practicing preventive measures.
Ren et al. stated that fear might persuade people to follow preventive guidelines (39). Maaravi et al. mentioned that people scared of COVID-19 tended to practice preventive measures more seriously (40). Therefore, giving people information about the consequences of ignoring preventive guidelines will result in more adherence to the guidelines.
Another factor associated with adherence to the preventive measures was recognized in many studies, and that is empathy, which plays a significant role in modern health and improves treatment outcomes (41). Commitment to society raises the level of health care strategies like washing hands in a hospital to prevent spreading diseases. It can also affect how an individual protects vulnerable people by practicing social distancing (42). Therefore, it seems crucial to enhance empathy and commitment to society to increase adherence to the preventive guidelines.
One of the most prominent properties of COVID-19 is that it spreads fast, and the disease's mortality rate has challenged health care systems, particularly those of developed countries. Accomplishing a union against the disease will certainly affect the virus transmission chain and stop it. A review of experiences in countries with efficient health care systems shows that controlling the virus transmission chain has been recognized as an effective strategy in dealing with the disease. Coronavirus appeared in Wuhan, Chia, for the first time on December 31, 2019. It took seven days for China to administer the required measures, such as quarantining the cities, houses, and infected areas, isolation, patient tracking in public places, constraining commuting, allocating all the facilities in hospitals and government organizations to preventive programs, prolonging the new year's holidays, controlling traffic, telecommuting, and enhancing public health education as main strategies of fighting against the disease, which resulted in a remarkable decrease (almost zero) in the number of patients. Successful countries in managing programs for fighting against COVID-19 have policies concerning prevention, which entails comprehensive programs of breaking the virus transmission chain through promoting social distancing, especially between infected and healthy people. Regarding cultural similarities between Iran and Asian countries, one of the most important facilitators to practicing preventive measures is to promote a collaborative atmosphere against the virus spread in the country.
The media is also considered essential in promoting adherence to the COVID-19 preventive guidelines. As stated in Cinelli and Limaye, warnings people receive from officially validated media impact their lives on both individual and public levels. Thus, the role of media cannot be underestimated. The media can positively promote efficient strategies during the COVID-19 pandemic (43, 44). Thus, it is required to publish scientific and evidence-based information.
5.4. Limitations of the Study and Further Recommendations
Since no instrument had been developed before the present study to identify barriers and facilitators to practicing COVID-19 preventive measures in Iran, investigating the parallel reliability of the questionnaire was impossible.
5.5. Conclusions
The developed questionnaire has proper psychometric properties to identify barriers and facilitators to practicing COVID-19 preventive measures among residents of Sanandaj city, Iran. This questionnaire is valid and confident enough to be applied. Although the designed questionnaire is the first instrument developed in Iran to identify barriers and facilitators to practicing COVID-19 preventive measures and still requires parallel reliability investigation, it can be considered an appropriate instrument for assessing its aims.