1. Context
The COVID-19 pandemic caused a lot of physical, psychological, and social consequences for the people of the world. Due to the lack of definitive treatment and effective vaccines, the world's governments faced many problems (1, 2).
Eventually, after much effort, the food and drug management licensed the Pfizer-BioNTech vaccine on December 11 and the Moderna one on December 18. In step with studies, these vaccines are 95% effective against COVID-19 for humans over sixteen years of age (3).
Vaccinating and immunizing people worldwide against disease is recognized as one of the public health's greatest achievements (4).
Public vaccination can't be guaranteed even after the public get admission to safe vaccines; due to the fact we're facing resistance to vaccine injection (5). Opposition to numerous vaccines has been found in medication records and is not a brand-new phenomenon. Because studies have proven that vaccination compliance is variable and contradictory, reaching customary recognition calls for widespread education concerning the safety and effectiveness of various vaccines (6).
It should be cited that everyone's vaccines mission the immune device of people and purpose a boom in inflammatory markers within a few hours after vaccination in humans with excessive hypersensitive reactions and sensitivities. Vaccination may motivate unusual reactions, so earlier than beginning the national vaccination, the clinical file of humans should be tested (7).
Resistance to vaccine attractiveness can be described as a complicated phenomenon that varies depending on the place, time, and kind of vaccine, and this complexity has led to demanding situations and ambiguities in clinical efforts to define it (8). People who resist the vaccine are those who were reluctant to do so or refused to receive the COVID-19 vaccine despite the availability of vaccination offerings (9-11).
Studies have examined several factors such as age, gender, level of education, and income in the degree of resistance of people to the COVID-19 vaccine (12, 13). Another important factor is directly related to acceptance and resistance. The vaccination process is the mental health of individuals (14). With COVID-19, home quarantines and increased anxiety and fear were reported worldwide, affecting people's ability to make decisions and cognitive processing (15, 16). After the production of different vaccines, some people did not participate in the nationwide vaccination process for various reasons such as death anxiety, paranoid thoughts, conspiracy, fear of the vaccine, and depression (17, 18). Simione et al. (19) examined the psychological factors determining the tendency to inject the COVID-19 vaccine. Studies have shown a high prevalence of uncertainty, paranoid thoughts, and fear of the COVID-19 vaccine in resistant individuals. Murphy et al. (20) showed that 35 and 31% of people were skeptical and resistant to the COVID-19 vaccine. People skeptical about the vaccine were mostly women, lived in the suburbs, and were less educated. People with phobias know that their fears are irrational and extreme, but they have no control over how much they fear. This causes them not to participate in the global vaccination process, not to trust the vaccine and their government, and to focus only on the negative dimensions (21). Many people have a needle phobia and show a very strong fear of getting vaccinated for this purpose. Studies have shown a prevalence of 11 to 66 million acupunctures among American adults who did not participate in the vaccination process (22).
Vaccines have long been considered a life-saving invention that has eliminated and controlled many infectious diseases in many parts of the world (23, 24). Acceptance of the COVID-19 vaccine seemed to be a determining factor in controlling the epidemic, but the notion that high vaccination rates fully controlled the virus emerged with the emergence of more infectious strains, such as delta and omicron, with significant proportions of hesitant vaccine recipients (25).
2. Objectives
The present study evaluated the psychological factors determining resistance to COVID-19 vaccine injection.
3. Data Sources
3.1. Protocol and Search Strategy
The PRISMA tick list became used to review research on the psychological factors that determine the resistance to COVID-19 vaccine injection (26). Articles in 2020 (June) and 2022 (May) indexed were used in research databases such as Google Scholar, ISI, Scopus, ScienceDirect, and PubMed.
3.2. Keywords
The following combinations of keywords were used in the search method: (Resistance) OR (Hesitancy) (abstract/title) AND (COVID-19) (abstract/title) AND (Epidemic) (abstract/title) AND (Vaccine) OR (Psychological Determinants) OR (Depression) OR (Anxiety) OR (Stress) (abstract/title).
3.3. Exclusion and Inclusion Criteria
Studies articles had been purposely selected in line with the inclusion and exclusion standards. Standards for entering the research protected; relating to the motive of this research, the lifestyles of a structured research framework, and eBook in a legitimate magazine exclusion criterion covered; articles wherein full-textual content became no longer available, articles which had been letters to the editor or having no abstracts.
3.4. Quality Assessment
The great of the article changed into assessing the usage of the PRISMA declaration and the standards proposed with the aid of Gifford et al. (26, 27). The items of the PRISMA assertion are the study objectives, having a look at population, sampling, method, inclusion and exclusion standards, data series equipment, records evaluation, moral concerns, presentation of the findings primarily based on the look at goals, congruence of the thing structure with have a look at kind, and discussion of the findings. The criteria proposed by Gifford et al. are for evaluating high-quality quantitative research, qualitative studies, and overview research. Objects have been scored on a -point zero/1 scale. In the last evaluation, the minimum acceptable inclusion score changed to 4 for quantitative studies and 6 for assessment research. The authors independently examined and analyzed every blanketed article, extracted applicable statistics, and entered them into a content analysis shape (27).
4. Data Extraction and Reporting
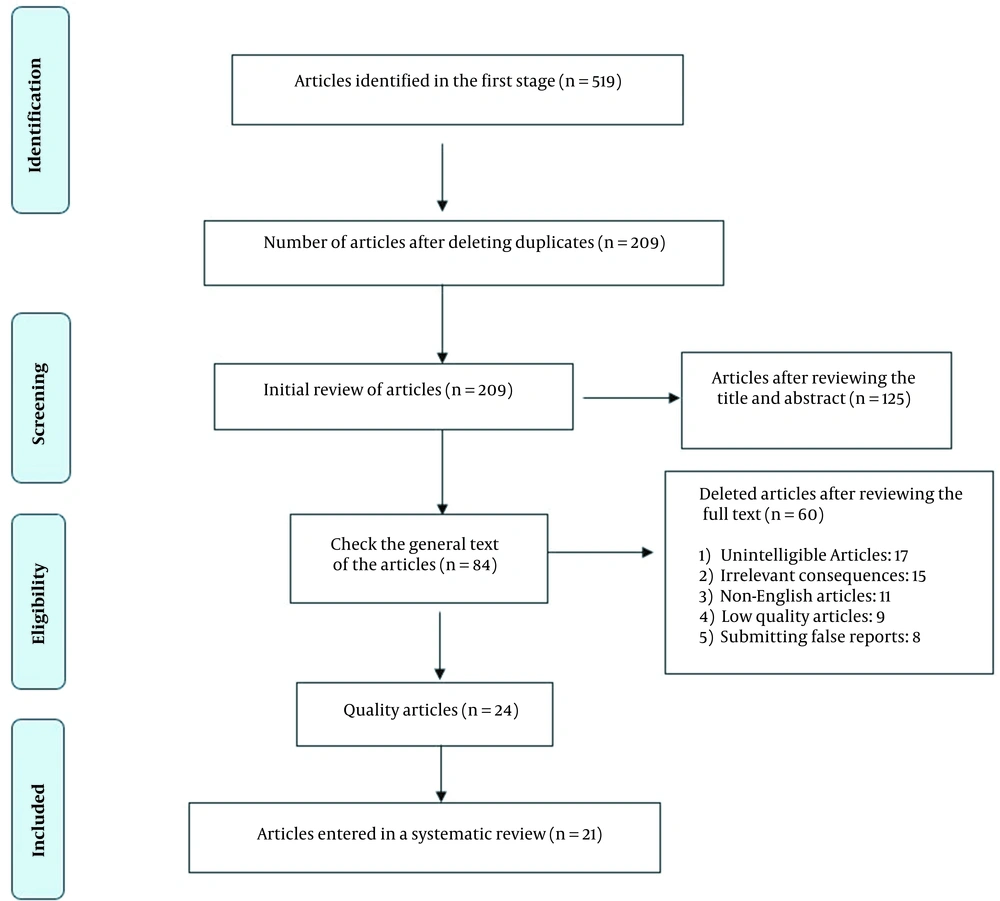
Abstracts of published articles were reviewed, duplicates were eliminated from the study in several stages, and eventually, 21 articles were decided on for comprehensive review and fact extraction (Figure 1).
5. Result
5.1. Selected Studies
In the initial review, 519 related articles were selected; after evaluating and removing duplicate articles, 209 articles remained. After more detailed studies and considering the entry and exit criteria, 21 articles were finally reviewed.
5.2. Characteristics of Studies
The systematic review also included 20 countries: Ireland, the United Kingdom, Indonesia, China, Turkey, the Netherlands, Belgium, Portugal, Italy, Kuwait, Egypt, Jordan, the United Arab Emirates, Ethiopia, Malta, Germany, the United States, Cameroon, Singapore, and Saudi Arabia.
5.3. Main Findings
Studies have shown that women of young age, education, low income, people with conspiratorial and paranoid thoughts, poor cognitive processing and decision-making, and people with depression, fear, and anxiety were highly resistant to the COVID-19 vaccine. In contrast, vaccine safety and efficacy levels, confidence, collective responsibility, media literacy, and good health were associated with accepting the COVID-19 vaccine.
In this evaluation study, 21 certified research articles have been analyzed. For this reason, Table 1 gives the results acquired from research articles on the psychological factors that determine resistance to the COVID-19 vaccine (Table 1).
| Authors | Purpose | Participants | Design | Country | Results |
|---|---|---|---|---|---|
| Nazli et al. (7) | Psychological factors affecting COVID-19 vaccine hesitancy | 467 | Cross-sectional | Turkey | Significant positive correlation between conspiracy theories and resistance to vaccination. Also, people who were not too afraid of COVID-19 and did not wear masks were more resistant to the COVID-19 vaccine. |
| Wismans et al. (8) | Psychological characteristics and the mediating role of the 5C model in explaining students' COVID-19 vaccination | 7,404 university students | Cross-sectional | Netherlands, Belgium, and Portugal | 41% of students were resistant to the COVID-19 vaccine. It was found that collective confidence and responsibility had a significant relationship with the students' intention to get the COVID-19 vaccine. People who were skeptical of the vaccine makers and only thought about themselves did not go for the vaccine. |
| Batty et al. (9) | Pre-epidemic cognitive function and COVID-19 vaccine hesitancy | 11740 | Cross-sectional | United Kingdom | 17.2% of participants were resistant to the COVID-19 vaccine. Also, people with low cognitive scores were more resistant. Age, gender, marital status, level of education, and income were significantly associated with the severity of resistance to the COVID-19 vaccine. |
| Ghazy et al. (10) | Determining the cutoff points of the 5C scale for assessment of COVID-19 vaccines | 446 | Cross-sectional | Egypt, United Arab Emirates and Jordan | 44.8% were from Egypt, 21.1% from Jordan, and 33.6% from the UAE. Studies have shown differences in psychological dimensions in acceptance and resistance to the COVID-19 vaccine. People with high levels of confidence and collective responsibility had a good acceptance of the vaccine. |
| Zintel et al. (11) | Gender differences in the intention to get vaccinated against COVID-19 | 46 studies | Review | Germany | 58.3% of the studies showed that men were more accepted than the COVID-19 vaccine. Young age, femininity, distrust of government, and education were significantly associated with resistance to the COVID-19 vaccine. |
| Butter et al. (12) | Psychological, social, and situational factors associated with COVID-19 vaccination intentions | (Key worker = 584; not key worker = 1,021) | Cross-sectional | United Kingdom | 17.7% were skeptical about getting vaccinated, and 8.1% were reluctant to get vaccinated. Lack of trust in the government, being a woman, low age, income, and low education showed a significant relationship with resistance to the COVID-19 vaccine. |
| Liu and Li (13) | Hesitancy in the time of coronavirus: Temporal, spatial, and sociodemographic variations in COVID-19 vaccine hesitancy | 443,680 | Cross-sectional | U.S. A | The role of individual and environmental factors in acceptance of the COVID-19 vaccine. Black people with paranoid thoughts and conspiracies were more resistant to the COVID-19 vaccine. Blacks did not trust whites for a variety of reasons. Being a woman, young age, education, and low income also played a role in the rate of vaccine resistance. |
| Al-Sanafi and Sallam (14) | Psychological determinants of COVID-19 vaccine acceptance among healthcare workers | 1019 | Cross-sectional | Kuwait | 83.3% were accepting of the vaccine, 9% were not accepting, and 7.7% were resistant. Dentists had the highest resistance to the COVID-19 vaccine. Various psychological factors, such as paranoid thoughts, phobias, uncertainty, and collective responsibility, were significantly associated with resistance to the COVID-19 vaccine. |
| Hajure et al. (15) | Attitude towards COVID-19 vaccination among healthcare workers | 24 studies | Review | Ethiopia | 70% of the studies had a positive attitude towards the COVID-19 vaccine, and 30% reported resistance to the COVID-19 vaccine. Numerous factors such as age, gender, mistrust, psychological distress, depression, concerns about vaccine safety, and fear were involved in resistance and acceptance of the COVID-19 vaccine. |
| Moccia et al. (16) | Perception of health, anxiety, and indecision in a group of Italians vaccinated against COVID-19 | 1564 | Cross-sectional | Italian | People were more receptive to vaccines with high efficacy and safety. more fear and anxiety were reported in the first dose. Various psychological dimensions, such as depression, stress, fear, and uncertainty, affected the resistance and acceptance of the COVID-19 vaccine. |
| Aw et al. (17) | COVID-19 vaccine hesitancy | 97 studies | Review | Singapore | Resistance to the COVID-19 vaccine was higher in less developed countries. Factors such as distrust of government, paranoid thoughts, fear, death anxiety, and family dissatisfaction were implicated in increasing individuals' resistance to the COVID-19 vaccine. |
| Salomoni et al. (18) | A systematic review on global COVID-19 vaccine acceptance | 100 studies | Review | Italy | Age, gender, race, education level and income level, mental health, and fear of COVID-19 play a significant role in accepting and resisting the COVID-19 vaccine. In general, the results of studies indicate the role of conspiratorial and paranoid thoughts in increasing resistance to the COVID-19 vaccine. |
| Simione et al. (19) | Effects of psychological factors on the propensity of the COVID-19 vaccine | 374 adults | Cross-sectional | Italian | High prevalence of uncertainty, paranoid thoughts, and fear of the COVID-19 vaccine in resistant individuals. Also, people with death anxiety were less likely to get the COVID-19 vaccine. |
| Murphy et al. (20) | Psychological characteristics associated with COVID-19 vaccine hesitancy | Ireland (1041) and the U.K. (2025) | Cross-sectional | Ireland and the United Kingdom | 35% and 31% of people were skeptical and resistant to the COVID-19 vaccine. People who were skeptical about the vaccine were mostly women, lived in the suburbs, and were less educated. They also had little psychological trust in their government, poor cognitive processing, and paranoid thoughts. |
| Cordina et al. (21) | Attitudes toward COVID-19 vaccination, vaccine hesitancy, and intention to take the vaccine | 2,529 | Cross-sectional | Malta | Fifty percent of people were resistant to the COVID-19 vaccine, and many were women. The opinions of friends and family played an important role in the acceptance and resistance of individuals. Conspiracy theories, fear of losing control, and death anxiety were also significantly associated with resistance to the COVID-19 vaccine. |
| Dinga et al. (23) | Evaluation of vaccine hesitancy to a COVID-19 vaccine | 2512 | Cross-sectional | Cameroon | 84.6% of people were resistant to vaccination. According to the results, people with low media literacy and health who were affected by the conspiracy theories about the vaccine were more resistant to the COVID-19 vaccine. Levels of anxiety and fear also played an important role in their acceptance. |
| Nehal et al. (24) | Worldwide vaccination willingness for COVID-19 | 63 studies | Review | Netherlands | 66% of people had a good acceptance of the COVID-19 vaccine. Also, being a woman, young age, low education, fear, and anxiety were significantly associated with the degree of resistance to the COVID-19 vaccine. |
| Almaghaslah et al. (25) | COVID-19 vaccine hesitancy adults | 862 | Cross-sectional | Saudi Arabia | 48% of people were vaccinated after the vaccination became mandatory. Many people were unsure of the vaccine produced and had a high level of fear. Also, being a woman, high anxiety, low levels of delirium, and phobia compared to COVID-19 contributed to the degree of resistance to the vaccine. |
| Yanto et al. (28) | Psychological factors affecting COVID-19 vaccine acceptance | 190 | Cross-sectional | Indonesia | 86.8% of people were accepted with the COVID-19 vaccine. In contrast, 13.2% had resistance to the vaccine. Factors such as smoking, education, trust in the government, and doctors played a role in resistance to the COVID-19 vaccine. |
| Walsh et al. (29) | Psychological correlates of COVID-19 vaccine hesitancy and resistance | Irish (N = 500) and UK (N = 579) | Cross-sectional | Ireland and the U.K. | 76% and 7% of Irish and British people accepted the COVID-19 vaccine. In contrast, 23% and 26% of people in Ireland and the United Kingdom resisted the COVID-19 vaccine. Women under the age of 30 were more resistant to the COVID-19 vaccine. People with higher education and children had a good acceptance of the vaccine. |
| Li et al. (30) | The relationship between self-document and behavioral measures of normal sadism and COVID-19 vaccination | 188 | Cross-sectional | China | People with antisocial and sadistic characteristics highly resisted the COVID-19 vaccine. They also had low education, poor economic status, and mental health problems. |
Articles About the Psychological Factors of Resistance to the COVID-19 Vaccine
5.4. Discussion
This study aimed to investigate the psychological determinants of resistance to the COVID-19 vaccine. The results showed that in addition to the influence of various demographic factors, inclusive of age, area of residence, gender, level of education, and income on the resistance of people to the COVID-19 vaccine, various psychological factors such as conspiratorial and paranoid thoughts, cognitive processing ability and Poor decision making, mistrust, depression, fear, and anxiety caused different levels of hesitancy and resistance to the COVID-19 vaccine among the people of the world (12-16).
The world has witnessed a primary humanitarian crisis because of COVID-19, which has affected all components of lifestyles around the globe and compelled international locations around the arena to take precautions and strict controls to decrease COVID-19 (1-3). However, in the very first months, it became clear that such precautionary measures were insufficient to stop the spread of COVID-19. Thus, the world agreed on vaccine production and development as one of the maximum promising health intervention strategies to reduce the superiority of COVID-19 (30). Because past studies have proven that the model of vaccines is variable and contradictory, achieving public acceptance calls for huge training in the protection and efficacy of various vaccines (21).
One of the interesting results of the present study was the high level of paranoid and conspiratorial thoughts among people with hesitancy and resistance to the COVID-19 vaccine (13-17). Paranoia entails irrational and continual mind and emotions that purpose a person to consider that others are looking to damage, deceive, or abuse them. In this case, they suppose that others are watching, listening, or following them. However, they do not have sufficient evidence to prove it (20). The most bizarre superstition surrounding the COVID-19 vaccine is the presence of a tracking chip, with conspiracy theories about the presence of a microbial chip in the vaccine to track individuals. The superstition was spread by posting a video on social media showing a microchip on the label of the COVID-19 vaccine. The purpose of this microchip is to ensure that the vaccine is not counterfeit and that it has expired (29). Another superstition is the vaccine's ability to alter people's DNA, but this information is completely contrary to science. DNA is in the nucleus of cells, and the vaccine does not enter the nucleus; thus, the vaccine does not alter DNA (11).
Emotional factors are very influential in acceptance and resistance to the vaccine (5). On the other hand, many people refuse to get the COVID-19 vaccine because of the limited side effects that it can cause and cause others to be skeptical (21). According to the results of this study, death anxiety, stress, depression, acupuncture, and fear of vaccine side effects increased hesitancy and resistance in many people around the world (16-19). It must be mentioned that each vaccine ventures the immune device and boom inflammatory markers within a few hours after vaccination, in addition to people with severe allergic reactions. The vaccine reasons unusual reactions, so the individual's scientific file ought to be reviewed earlier than beginning general vaccination (9). This can increase people's confidence in the vaccine and reduce resistance to safe vaccination (15). An extensive look has proven that allergic reactions to vaccines commonly arise for 1.31 percent according to million vaccine doses and not using fatalities (12). Preliminary studies have proven that the Pfizer-BioNTech vaccine also can reason slightly too mild aspect outcomes after the first and second doses, consisting of muscle pain, redness or swelling on the injection web page, fatigue, headache, joint ache, and fever. Of course, these signs can suggest the warfare and effort of the immune device to fight the virus (3).
6. Conclusions
The survey results in the last two years indicated the role of psychological, social, economic, academic, personality, and interpersonal factors in accepting or resisting the COVID-19 vaccine. Since the timely injection of the vaccine can prevent much damage and increase the level of physical and mental health of society, to begin with, it's miles necessary to pay special interest to the psychological and social dimensions of the vaccine further than scientific offerings. In different words, the non-reputation of vaccines in emergencies can create widespread demanding situations for public health authorities, and in the context of the COVID-19 pandemic, failure to address such challenges can disrupt the user's unprecedented efforts in managing the epidemic. Health literacy, responsibility, and mental health of society's citizens must be improved to achieve this.