1. Context
Regular exercise training is key in weight management and preventing obesity and overweight. It reduces the risk of cardiovascular diseases, such as high blood pressure and stroke (1). Exercise training prevents or delays type 2 diabetes development risk (2). On the other hand, many types of cancer are reduced by regular exercise and physical activity. The world is currently reeling under the COVID-19 pandemic, a complex multisystem disorder (3) displaying high morbidity and mortality and affecting many systems. The COVID-19 pandemic has led to rapid, incredible changes in the lives of millions of people worldwide. At the start of the coronavirus pandemic, many people, especially children and adolescents, were subjected to home confinement and unable to do their physical and sports activities the same way as before. Physical activity is any bodily movement produced by skeletal muscle that requires energy expenditure (4). An average of 60 min/day of moderate- to vigorous-intensity aerobic physical activity across the week provides health benefits for children and adolescents (5).
Today, some countries have reduced some of the corona restrictions. On the other hand, there are various vaccines, but after three years since the beginning of the corona pandemic, the number of infected cases has reached more than 603 million, and the number of deaths has reached 6484136 until this date (September 7, 2022) (6). There is still no belief that we are in the post-corona era. Based on this, in this review article, the status of physical activity during the corona period and its relationship with the physical and mental health of children and adolescents were investigated, and practical recommendations regarding physical activity during the corona period were highlighted for the target groups.
2. Methods
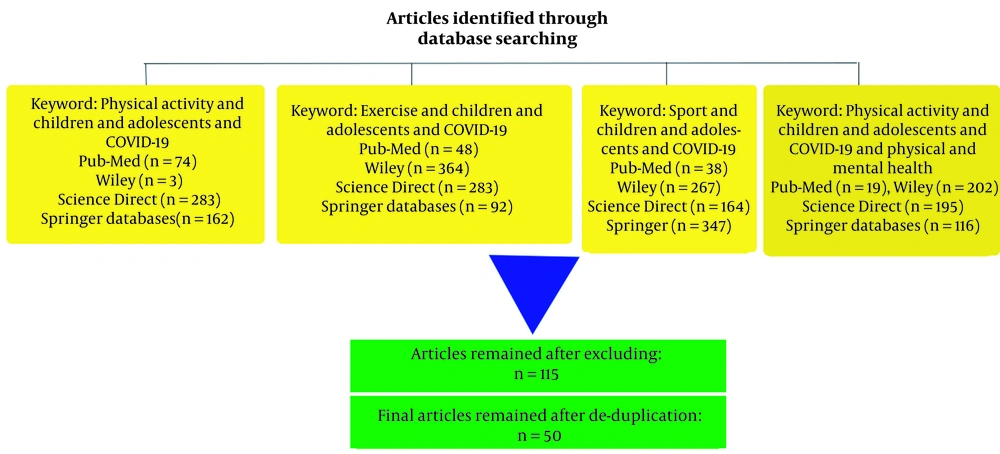
A literature search was conducted on Pub-Med, Wiley, Science Direct, and Springer databases from 2020 to 2022 to find related articles using the following keywords (Figure 1): Exercise and children and adolescents and COVID-19 (Pub-Med (n = 48), Wiley (n = 364), Science Direct (n = 283), and Springer databases (n = 92)), physical activity and children and adolescents and COVID-19 (Pub-Med (n = 74), Wiley (n = 3), Science Direct (n = 283), and Springer databases (n = 162)), sport and children and adolescents and COVID-19 (Pub-Med (n = 38), Wiley (n = 267), Science Direct (n = 164), and Springer databases (n = 347)), physical activity and children and adolescents and COVID-19 and physical and mental health (Pub-Med (n = 19), Wiley (n = 202), Science Direct (n = 195), and Springer databases (n = 116)). Two thousand six hundred fifty-seven articles were found in the primary research process. In this review, we included any randomized single or double-blinded case-control, review, cohort, or experimental study with an intervention involving or an objective to explore the level of physical activity in children and adolescents during the corona period and its relationship with physical and mental problems. Objective or subjective measures of exposure and outcomes were considered. Exclusion criteria included: (1) Clinical populations (e.g., children and adolescents with chronic health conditions, e.g., asthma, cardiovascular diseases, diabetes, cancer, neuromuscular problems or developmental disorders, e.g., cerebral palsy, autism); (2) qualitative studies; (3) studies with unclear statements or results. In addition, studies that were not available in English were excluded. One hundred fifteen articles remained after being excluded. Also, duplicate articles were removed. Finally, 50 articles remained that met the necessary conditions to enter the study and were related to the purpose of the article.
In addition to the mentioned keywords, the filters used in the database include publication year (2020 - 2022), medicine and public health. On the other hand, books and chapters have been removed.
Titles and abstracts were screened for relevance (FE, MJ) independently. Full texts of identified articles were retrieved and read to assess eligibility for inclusion. Reviewers independently extracted and cross-checked relevant data using a pre-piloted data extraction form.
Reviewers who extracted the data also assessed the methodological quality of the primary studies, and any discrepancies were resolved by consensus. Risk of bias assessment was completed as part of the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) of evidence quality.
3. Results
3.1. Physical Activity During the Corona for Children and Adolescents
According to World Health Organization Guidelines (5) and Physical Activity Guidelines for Americans (7), an average of 60 minutes per day of moderate- to vigorous-intensity aerobic physical activity across the week provides health benefits for children and adolescents. American Academy of Pediatrics guidelines for leisure screen time is two hours per day or less for children (8). Studies have shown that unprecedented lifestyle stressors associated with the pandemic have led to a decrease in the level of physical activity (9-12), an increase in screen time (9, 10, 12), and BMI (13) hence aggravating the childhood obesity epidemic.
Tulchin-Francis et al. (11) found moderate-to-vigorous intensity physical activity among American children aged 3 - 18 years decreased while light physical activity remained the same compared to before the pandemic. Other studies (14-16) have shown diminutions in physical activity levels due to COVID-19 in the USA. Nagata et al. (16) found that the average moderate-to-vigorous intensity physical activity among adolescents in the United States during the COVID-19 pandemic was only two h per week, and the percentage of adherence to recommended physical activity guidelines reduced from 16.1% before the beginning of the corona pandemic to 8.9% during the pandemic. Mitra et al. (17) observed decreased physical activity among Canadian children and adolescents aged 5 - 17 during the COVID-19 pandemic. Moore et al. (12) reported only 4.8% (2.8% girls, 6.5% boys) of Canadian children and 0.6% (0.8% girls, 0.5% boys) of adolescents were meeting recommended physical activity guidelines during COVID-19 restrictions. In China, Yuan et al. (9) reported only 17.4% of children and adolescents with intellectual disabilities (ages 6 - 18 years) were able to achieve the recommendation of 60 min of daily moderate-to-vigorous physical activity. In Germany, Poulain et al. (10) observed that compared to the pre-pandemic period, physical activity in children aged 8 - 16 was lower during the first COVID-19-related lockdown and did not change significantly between the first and the second lockdown. One study reported that 81% of adolescents aged 11 - 17 are insufficiently physically active globally (18). In Iran, a study (19) conducted on male and female students showed that the average time spent daily in moderate-to-vigorous physical activity was 18.47 min, much lower than the WHO guideline. Also, this study showed that only 4% of Iranian adolescents did moderate-to-vigorous physical activity for more than 30 minutes a day. Meanwhile, male students were significantly more active than their female counterparts. However, in line with Guthold et al.’s (20) findings, there seems to be a significant difference in the prevalence of insufficient physical activity across genders, regions, and countries.
3.2. Physical Activity and Physical and Mental Health During Corona in Children and Adolescents
Numerous previous studies support a clear inverse relationship between moderate exercise training and illness risk, especially influenza, pneumonia, and COVID-19 (21-23). Regarding mental health, several studies showed an increase in depression (19, 24, 25), anxiety (13, 19), psychological stress (26), other mental health problems (10, 27-29), a decreased quality of life (10, 29) and behavioral difficulties (27, 30, 31), during the pandemic lockdown compared to before the beginning of corona pandemic that theses related to the decrease in the level of physical activity. In the study of Ghorbani et al. (19), most Iranian adolescents reported symptoms of mild-to-moderate mental health disorders, including depression, anxiety, and stress. Ben Brik et al. (32) reported that parental physical activity was associated with better parent and child mental health and anxiety symptoms during the COVID‐19 pandemic in Brazil, Mexico, and Colombia. Regarding the effects of decreased physical activity levels on physical health in children and adolescents, most of the observed problems included overweight and obesity and increased BMI (13), negative effects on glycemic control (33), musculoskeletal pain (34), and joint problems (35). On the other hand, evidence showed that being overweight and obese, which extends to nearly a third of the world population, was associated with severe COVID-19 (36). Patel et al. (37) found that the COVID-19 pandemic has decreased the health impacts of weight management programs, particularly in males. This is especially due to the measures taken to reduce the spread of COVID-19, including the closure of many businesses, schools, and recreational facilities and changes in the level of physical activity and eating habits leading to increased body weight and BMI (37).
4. Discussion
With the spread of the corona pandemic, children and adolescents in many countries faced massive changes in their daily lives, including school closures, quarantine, home confinement, and social distancing rules, which can put considerable pressure on them and cause a decrease in the level of physical activity and a negative effect on their physical and mental health.
Experimental evidence supports a clear inverse relationship between moderate exercise training and the incidence of numerous mental and physical health problems (10, 13, 21, 22, 26-28, 32). So, we mainly recommend moderate-intensity exercise training for healthy and asymptomatic children. One of the mechanisms by which moderate-intensity exercise can improve the immune system’s response is by regulating leptin levels and weight management. There is a link between obesity and respiratory tract infections, especially COVID-19 (38). Levels of leptin, a hormone that regulates appetite, metabolism, and the ability to fight infection, are high in obese people (39). It seems that an increase in leptin levels, thus the incidence of leptin resistance, impairs the body’s ability to fight off infections in the lungs and various parts of the body, including diminished natural killer (NK)-cell cytotoxicity and delayed pro-inflammatory cytokine expression (40). Moreover, leptin plays an important role in regulating body weight by signaling the size of adipose tissue mass (41). It has been reported that moderate-intensity exercise training decreased plasma leptin levels both in obese people (42) and healthy subjects with normal weight (43). At least an average of 60 min/day of moderate- to vigorous-intensity aerobic physical activity across the week is strongly recommended for weight management and other physical and mental health benefits in children and adolescents (5). A suitable aerobic exercise training modality can include dancing to music, participating in aerobic exercise classes online, walking up and down the stairs, skipping rope, cycling, jogging, or walking outdoors. We recommend that children and adolescents add resistance, stretching, and balance exercises or a combination to their home workouts.
In schools, students should be educated to maintain a distance of at least 1 meter and not gather during physical activity classes. If a student shows any abnormal respiratory symptoms, should be contacted with the student’s parents immediately. In order to avoid crowding in physical education classes, it is recommended to implement staggered timetables (44). Although school closures are an effective measure against the spread of COVID-19 (10), considering its negative effects on the level of physical activity and, as a result, physical and mental health, school closures should be prevented for as long as feasible.
Students who have underlying diseases (such as asthma, cancer, diabetes, heart diseases, immune problems, or neurodevelopmental disorders), since they have a weak immune system in the face of the coronavirus and so higher risk of severe COVID-19 illness (45), it is better to avoid attending physical education classes at school. However, suitable activities should be designed for them at home or outdoors. Also, children and adolescents who play sports at professional levels should note that in elite athletes who do heavy training, their immune system is weakened due to the effect of the open window against respiratory infections. Hence, they are at risk and must strictly follow the health instructions. The open window is a situation where several immune cell functions, including oxidative burst activity and chemotaxis of neutrophils, monocyte antigen presentation, monocyte, and lymphocyte cytokine production, production of immunoglobulins by B lymphocytes, NK cell cytolytic activity and T-lymphocyte proliferation is temporary depressive after heavy training (46). Numerous studies have reported that prolonged high-intensity physical activity leads to immunosuppression (47-50). The effect of prolonged high-intensity physical activity on immune function has been mainly ascribed to increasing circulating stress hormones such as cortisol, adrenaline, prolactin, and growth hormone known to have immunomodulatory effects (46). For elite athletes with strenuous training to prepare for sporting events, it is necessary to limit outdoor exercise training to sports camps designed by clubs with strict observance and separation of team members from contact with outsiders. All athletes should be tested for coronavirus before entering training camps. A 2-week quarantine out of camps and competitions is necessary for any athlete or coach with suspected or established COVID-19 disease (51).
5. Conclusions
Restrictions on mobility, social distancing, or closure of schools, clubs, and recreational centers, although an effective measure against the spread of COVID-19, have caused an increase in sedentary behavior, and so the incidence of numerous mental and physical health problems. Therefore, when it is necessary to create these restriction periods, their prolongation should be avoided as much as possible. Engaging in vaccination and continuing physical activities in compliance with safety guidelines is also necessary.