1. Context
Transgender is incongruence between gender identity (gender expression) and biological sex (1, 2). Transgender individuals constitute about 0.5% of the adult population (3). On the one hand, the prevalence of transgender individuals in today’s societies is increasing; on the other hand, many experience psychological distress (4). Despite efforts to support this vulnerable group and the availability of medical and psychological treatment, they face many challenges and barriers (such as social discrimination and marginalization) that put them at risk for negative psychological outcomes, including suicidal behaviors (5).
Suicide behavior has a broad meaning and includes a range of phenomena, including suicide ideations (thoughts about killing oneself without preparatory behavior), other suicidal behavior and preparatory acts (preparing to commit an attempted suicide before the possibility of injury has begun), suicide attempts (a self-destructive and non-lethal act in which the conscious person puts herself/himself at risk of death), and suicide (death from self-inflicted trauma to kill oneself consciously) (6).
According to research, suicide is one of the health concerns among sexual minorities (7, 8). In this regard, some studies have found that the risk of suicidal behavior in transgender people is high (9-11). However, the relationship between transgender and suicidal behaviors is unknown (7)). Various studies have noted different statistics on suicidal behaviors among transgender people, which challenges health policymakers to plan for protective interventions (7, 12). Since transgender people experience many social, economic, and health vulnerabilities (13) and increasing the chances of suicide in transgender individuals may be related to psychological issues such as depression, family and social rejection because of their sexual identity, the likelihood of having sexually transmitted diseases such as HIV/AIDS, being unmarried, and the possibility of violence against them (4, 8, 14-18); therefore, transgender individuals may be at great risk of suicidal behaviors (19). Also, transgender individuals avoid receiving health care for various reasons, such as experiences of stigma and discrimination (20). Therefore, behaviors such as alcohol and drug abuse, depression, victimization, and trauma are frequently seen among transgender individuals (21-23). However, there is little information about suicidal behaviors in transgender individuals (24), and the exact statistics of suicides in transgender individuals are without sufficient documentation (25).
Although research on suicide in transgender individuals is on the increase, most of these studies have small sample sizes (26, 27), are related to a specific geographical area or a specific country (28-31), are about a single suicide-related outcome such as attempt (32, 33) or ideation (34, 35), and specific gender (32) or age group (36, 37). Based on this description, the purpose of the current research was to review the prevalence of suicidal behaviors among transgender people.
2. Methods
The current research is a systematic review and meta-analysis of the prevalence of suicidal behaviors in transgender people. This research was planned and conducted in 2020. The technique of reporting the current research was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) list.
2.1. Search Approach
In September 2020, the researchers surveyed six international sites, i.e., EMBASE, Medline/PubMed, Google Scholar, ProQuest, ISI Web of Science, and Scopus. Keywords for international databases included prevalence, epidemiology, suicide, suicide behavior, suicide attempt, suicide ideation, transgender, transsexual, gender identity disorder, gender dysphoria, transgender person, and transsexual person. The collected information arrived at EndNote, X8 software, and duplicate papers were automatically removed. It is worth noting that two researchers (a Ph.D. in psychiatric nursing and a senior expert in epidemiology) examined the studies separately.
2.2. Inclusion and Exclusion Criteria
Papers on the occurrence of suicidal behaviors (suicide ideation and suicide attempt) in transgender persons were included in the research. Also, the language of the studies should be English, the full text of the papers should be available, and the type of studies should be cross-sectional. On the other hand, studies published in conferences, posters, and congresses were excluded from the study.
2.3. Assessment of the Quality of Studies
Joanna Briggs Institute’s critical appraisal checklist was used to evaluate the quality of studies (38). Assessment of the quality of the studies was done by two members of the team who had previously received the necessary training.
2.4. Statistical Analysis
Totally analyses were performed by STATA, version 13 software. The discrepancy among the studies was reviewed by Cochran’s test (with a significance level less than 0.1) and its combination using I2 statistics (with a significance level greater than 50%). Random effects were used with the variance image method for the heterogeneity model.
2.5. The Registration and Protocol
Not applicable.
3. Results
3.1. The Study Selection
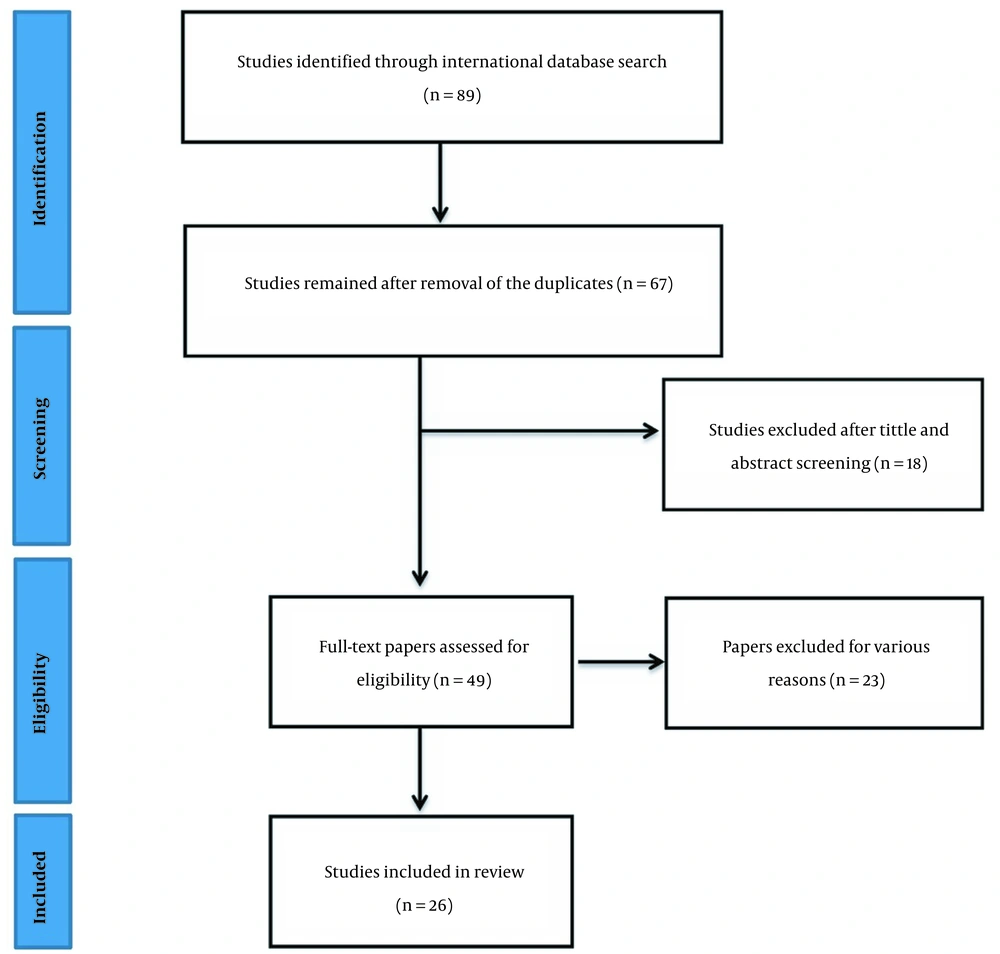
After searching different databases, 89 studies were considered in the first stage, and duplicate studies were removed. Then, in the second stage, 67 studies were reviewed in terms of title and abstract; at this stage, 49 studies were selected, and finally, after reviewing the full text of the studies, 26 studies were analyzed. Figure 1 shows the study flow chart. From the studies that entered the analysis process, 20 had been conducted in the United States (5, 36, 39-56), two in Brazil (57, 58), one in China (30), one in Nepal (59), one in Argentina (31), and one in Canada (28).
3.2. Heterogeneous Results
During the data analysis, the researchers observed a high level of heterogeneity in the findings. This value was obtained for suicide attempts (I2 = 96%) and suicide ideation (I2 = 97%). Due to the highly heterogeneous nature of the results, random effects were reported based on the model.
3.3. Findings
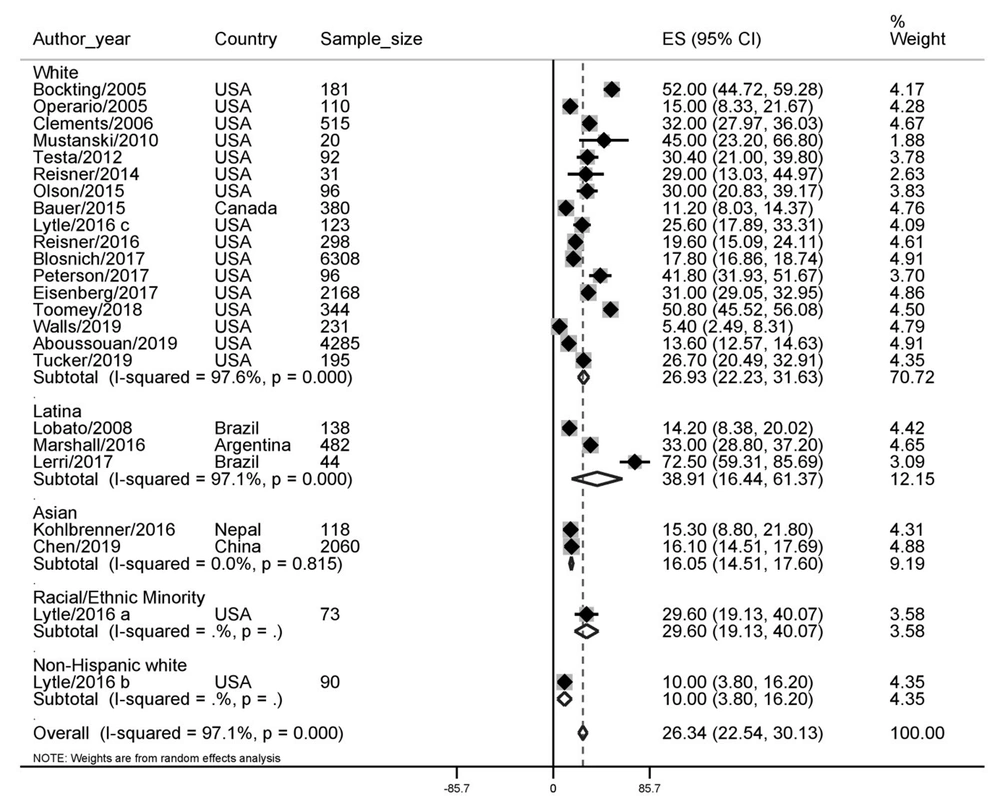
3.3.1. Suicide Attempt
The prevalence of suicide attempts in transgender people was 26.34% (95% CI for 22.54 - 30.13). This finding separately showed that the highest prevalence was in Latina (38.91) and the lowest in the non-Hispanic white race (10%). The prevalence of suicide attempts in transgender people is shown in Figure 2.
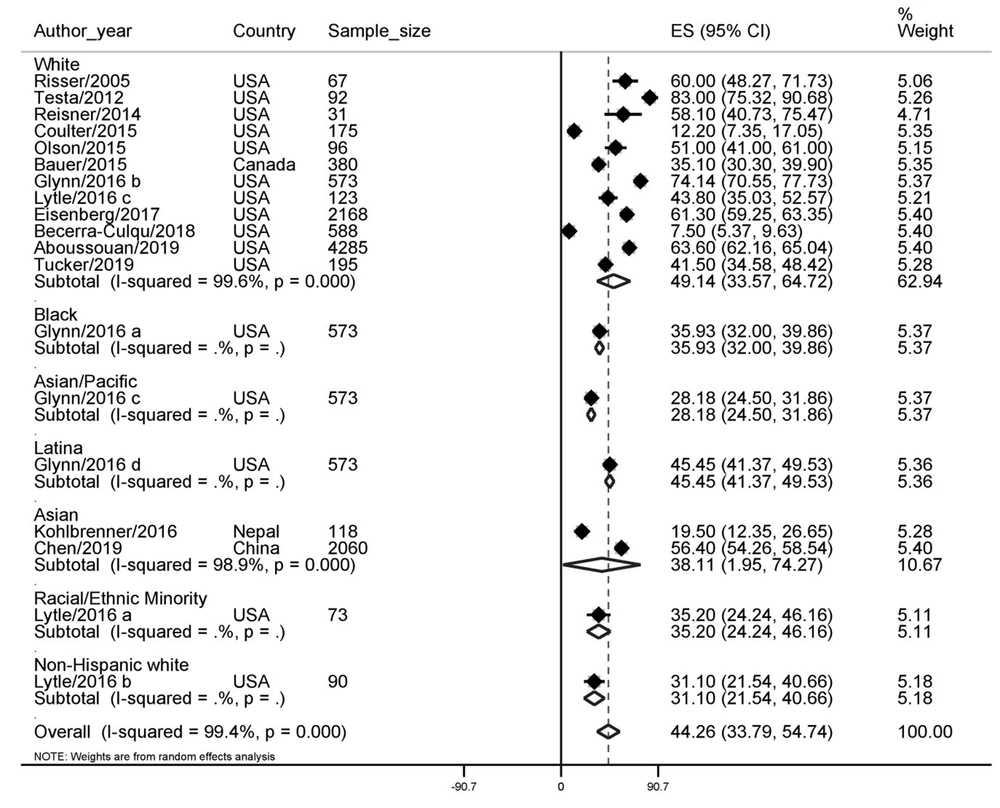
3.3.2. Suicide Ideation
The prevalence of suicide ideation in transgender people was 44.26% (95% CI for 33.79 - 54.74). This finding, by race, showed that the highest prevalence was in the White race (49.14%) and the lowest in the Asian/Pacific race (28.18%). The prevalence of suicide ideation in transgender people is shown in Figure 3.
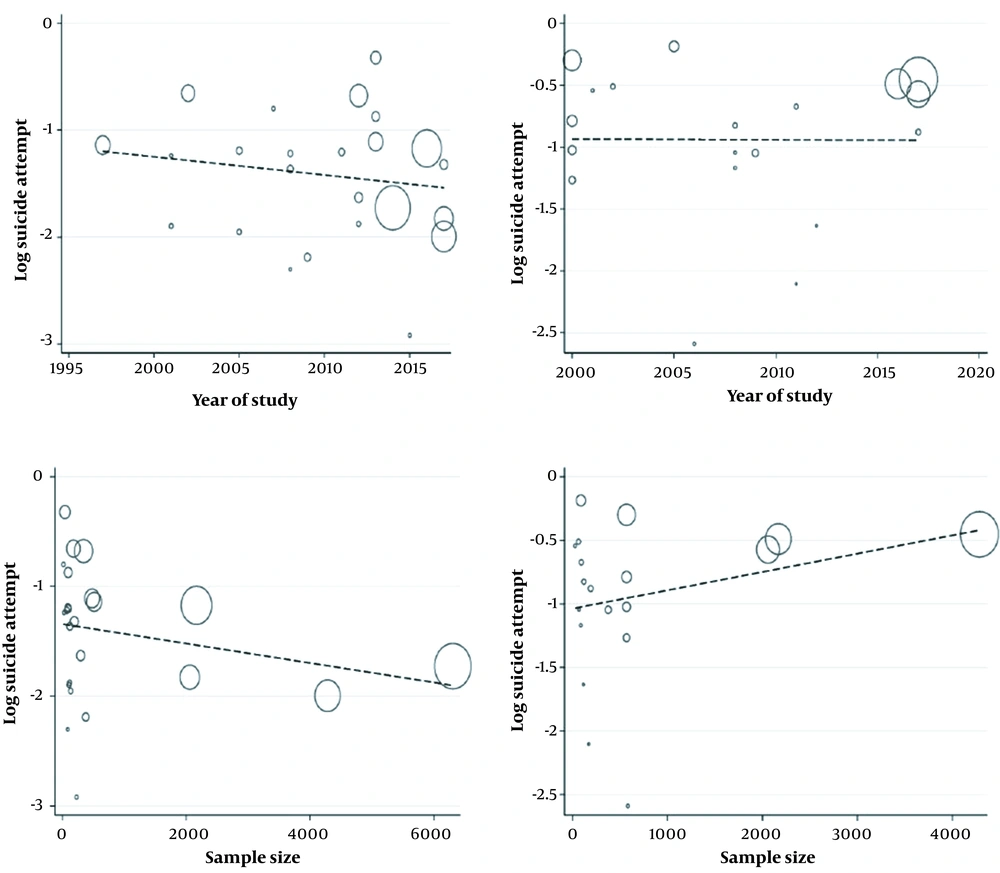
3.4. Meta-regression
The results of a study on suicide prevalence in recent years showed that a declining trend had been observed, but the finding was not statistically significant (P = 0.446). Based on the sample size, the results showed that the larger sample size was associated with a lower prevalence of suicide, but this finding was not statistically significant (P = 0.262). These findings showed no association with suicide ideation based on the year of the study (P = 0.997). Based on the sample size of the studies, a larger sample size was associated with a higher prevalence of suicide ideation, but this finding was not statistically significant (P = 0.285) (Figure 4).
3.5. Bias Risk in Studies
Table 1 lists the qualitative evaluation of the papers submitted to this study in accordance with the Joanna Briggs Institute critical appraisal checklist.
| Author Name | Year | The Sample Was Representative. | Participants Appropriately Recruited. | The Sample Size Was Adequate. | Study Subjects and the Setting Is Described. | Data Analysis Conducted | Objective, Standard Criteria, Reliably Used | Appropriate Statistical Analysis Used | Confounding Factors/ Subgroups/Differences Identified and Accounted for | Subpopulations Identified Using Objective Criteria |
|---|---|---|---|---|---|---|---|---|---|---|
| Bockting et al. (39) | 2005 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Operario and Nemoto (40) | 2005 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Risser et al. (42) | 2005 | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes |
| Clements-Nolle et al. (41) | 2006 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Lobato et al. (57) | 2007 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Mustanski et al. (43) | 2010 | No | Unclear | No | Unclear | Yes | Yes | Yes | No | Yes |
| Testa et al. (44) | 2012 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Reisner et al. (45) | 2014 | No | Yes | No | Yes | Yes | Yes | Yes | No | Yes |
| Olson et al. (46) | 2015 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Bauer et al. (28) | 2015 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Coulter et al. (54) | 2015 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Lytle et al. (47) | 2016 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Kohlbrenner et al. (59) | 2016 | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Unclear | Yes |
| Glynn et al. (55) | 2016 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Marshall et al. (31) | 2016 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Reisner et al. (48) | 2016 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Blosnich et al. (49) | 2013 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No |
| Peterson et al. (5) | 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Eisenberg et al. (50) | 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No |
| Lerri et al. (58) | 2017 | No | Yes | No | Yes | Yes | Yes | Yes | No | Yes |
| Toomey et al. (36) | 2018 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Becerra-Culqui et al. (56) | 2018 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Walls et al. (51) | 2019 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Chen et al. (30) | 2019 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | No |
| Tucker et al. (53) | 2019 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Aboussouan et al. (52) | 2019 | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | No |
Joanna Briggs Institute Critical Appraisal Checklist Applied for Included Studies
4. Discussion
Sexual orientation in sexual minorities is not only associated with mental disorders, but the community’s view of these people leads to behaviors such as suicide and suicidal ideation. In the present study, the prevalence of suicide attempts in transgender people was estimated to be 26.34% (22.55 to 30.13%), and the idea of suicide in transgender people was estimated to be 26.44% (33.79 to 54.74). In this regard, Aboussouan et al., in their study, showed that self-injury behaviors and suicide and suicidal ideation are more common in transgender people (52). Another study found that suicidal ideation was more common among persons with gender identity disorders (49). A study also showed that the prevalence of clinical depression in transgender people is more than 44%, so this statistic is important considering the relationship between depression and suicide (21). A study in the Ontario, Canada community found that suicidal thoughts accounted for more than 35 percent and suicide attempts for about 11 percent among transgender people. The study also found that factors such as social support, reduced fear of transgender people, and changing teachers’ identities based on the appropriate gender can effectively reduce suicidal ideation (28). A study in China showed that the prevalence of suicidal ideation and suicide in transgender people is 56.4% and 16.1%, respectively, which is much higher than the general population of China (30). A study in American society showed that the prevalence of suicide among transgender people is 32% that with the social acceptance of these people by society can reduce the suicide attempt of these people (41). Another study in the United States found that the prevalence of suicide attempts in these individuals is about 14% (36). Another study on more than 81,000 students shows that the prevalence of transgender in the study population was 2.7%, and about 61% of them had suicidal ideation, 3 times more than suicidal thoughts in cisgender people (50). A study also found that suicidal ideation was more prevalent among ethnic minorities; transgender is more prevalent in the United States than non-Hispanic whites (47). In a study conducted in Brazil, more than 14% of transgender people attempted suicide, and the prevalence of HIV in these patients was reported to be 17.6% (57). A study in Argentina found that the prevalence of suicide in transgender people was about 10 times higher than in the general population, estimated at 0.4 to 4.4 percent in international studies (31). But a study looked at suicide attempts and suicidal ideation in transgender people from a different perspective and found that more than 40 percent of transgender people were in contact with people who had attempted suicide, and 32 percent lived with people that have died by suicide (53). This may be one of the reasons for suicide attempts and suicidal ideation in transgender people. Another study found that the prevalence of partner violence was higher in transgender people than in others associated with suicide attempts (51). A study also found that unsafe sex and substance use are more common in this group (40).
Systematic review studies have certain limitations, and this study is no exception. One of them was the lack of full access to the information of some studies. We contacted the study’s authors, but in some cases, no response was received. One of the limitations of this study was that the prevalence results were not examined separately for different subgroups, including age groups and gender.
5. Conclusions
Transgender people have higher suicide attempts and suicide ideation rates than the general population. This study showed that the rate of suicide attempts in this group of people has decreased in recent years; also, statistical analyses indicate an increase in the rate of suicide ideation among transgender persons. Although these findings were insignificant in clarifying this issue, studies with more statistical samples are required.