1. Background
Hospitals and healthcare centers are symbols of social progress and essential economic development and stability. They represent one of the country's critical financial resources. Their malfunction can impose a significant economic burden on any nation (1). Therefore, they should be designed, organized, and managed to avoid damage to their structures in the face of disasters and to provide timely, efficient, and effective services (2). Various statistics illustrate the impact of natural disasters on healthcare centers worldwide. For instance, the total effect of the 2014 flood in Serbia and the damage caused by disasters over 15 years in the United States to the health system infrastructure of both countries were estimated at 5.7 million euros and 3.12 billion dollars, respectively (3, 4). A retrospective study in 2013 reported that 119 natural disasters and hazards were registered across 25 provinces of Iran from 2001 to 2011, leading to the failure of 1,401 primary healthcare centers. The severity of structural, non-structural, and functional damages was reported as 40.6%, 56.6%, and 91.9%, respectively (5).
Risk assessment, including recognizing hazards, vulnerability, and capacity, is the first step to reducing risk and ensuring resilience and continuity of operations in emergencies. Continuous assessment provides necessary information for system improvement and can be conducted across three domains: Structural, non-structural, and functional. Structural elements refer to parts of the building that support it and resist pressures (6). Serious monitoring during the construction phase, performing concrete tests, inter-organizational cooperation such as with road and urban development organizations, municipality, and engineering systems, and obtaining approvals from relevant organizations are essential during hospital construction (7).
Non-structural elements include facilities, equipment, and architectural factors of the hospital, which are crucial for the daily operations of medical centers. If damaged, their function is disrupted and may even cause physical harm to patients and personnel (3). The non-structural part accounts for at least 80% of hospital construction costs. However, its retrofitting costs are much lower. Given the safety costs incurred by personnel and patients, transportation costs, damages caused by service failures, and the costs of making non-structural elements safe are fully justified (8). The functional dimension also includes management and a disaster response plan. Despite the importance of structural and non-structural resilience, past experiences suggest that the most significant impact of disasters is on a hospital's ability to meet functional needs. Technology, measures, and performance management of hospitals are among the significant challenges of health strategies in dealing with disasters (6). In a study by Mehrabi et al., defects in short-term and long-term planning were identified as the highest priority in hospital preparedness (9).
In the US, the 2019 National Health Security Preparedness Index, which assesses the capability to provide health care in large-scale public threats, indicates only a moderate overall preparedness level with a score of 7.6 out of 10. However, the criterion assessing the capability to maintain the quality of health care during and after the event scored 9.4, indicating a significant gap in preparedness (10). Studies conducted in Japan (11), China (12), India (13), Iran (14), Pakistan (15), and Korea (16) have evaluated the level of disaster preparedness in all studied hospitals as poor and inadequate. Hatami et al. reported the operational, structural, and non-structural preparedness levels in Ahvaz at 51.48%, 54.82%, and 97.33%, respectively. They also reported the risk level for Ahvaz at 58.62% (17). Therefore, a correct and comprehensive assessment before an incident enables the estimation of medical centers' efficiency during crises, facilitates preventive measures, and increases crisis preparedness. Under these conditions, the planning and organization of facilities, workforce, and expected resources are conducted more purposefully and accurately (11).
The Hospital Safety Index (HSI) serves as a quick screening and assessment tool and an educational guide for the risk management team (18). Analysis of published studies on disaster situations from regions such as the Caribbean, Africa, North America, Europe, Pakistan, and Japan demonstrates that real experience supports the content and value of this toolkit, which encompasses the six primary functions of the World Health Organization (WHO) health system framework. The studies suggest that using an internationally valid tool such as the HSI is beneficial and allows for standardized comparisons (15).
2. Objectives
Since no study has been conducted in Khuzestan Hospitals and safety assessments in hospitals are limited to the annual accreditation of the deputy of treatment, this study investigates the safety status of selected hospitals in Ahvaz city in the face of disasters.
3. Methods
This cross-sectional and descriptive study was conducted in three hospitals in Ahvaz city during 2020 and 2021. These included hospital 1, chosen for its diversity of specialties, comprehensiveness of departments, and size; hospital 2, selected because it was newly built with modern safety considerations; and hospital 3, noted for being non-teaching and affiliated with the Social Security Organization. The assessment of the functional dimension was conducted under the guidance of the crisis committee directors, the non-structural dimension with the active participation of facility forces, and the structural dimension by structural engineers and the technical office in the hospitals and the University of Medical Sciences. The entry criteria involved interviewing past and current officials of the units, followed by involving individuals who could provide valuable information during the investigation. The HSI was used to assess the safety status across three dimensions: Functional, non-structural, and structural. This assessment includes five sections examining 145 indicators: General information about the hospital, identifying hazards, functional safety, non-structural safety, and structural safety. The assessment form, standardized by Ardalan et al. (6), was completed by the researcher through interviews, observations, and document review. To determine the overall weight of the three primary parts of the checklist, weights of 0.2, 0.3, and 0.5 were assigned to functional, non-structural, and structural safety, respectively. Each index received a score of zero, 0.5, or 1 based on low, moderate, and high evaluations. In addition to determining the safety status of each hospital based on 145 questions, the challenges and deficiencies related to each dimension were examined and recorded in the description section of the checklist.
4. Results
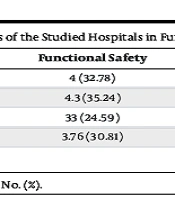
Tables 1 and 2 present the demographic characteristics and safety levels of the studied hospitals in functional, non-structural, and structural dimensions.
| Hospital | Establishment (Reconstruction), y | Organizational Affiliation | Number of Approved Beds | Number of Active Beds | Bed Occupancy Rate, % |
|---|---|---|---|---|---|
| 1 | 2001 | Government-educational | 714 | 684 | 70 |
| 2 | 2018 | Government-educational | 284 | 269 | 60 |
| 3 | 2017 | social security | 100 | 123 | 61 |
Demographic Information of the Studied Hospitals in 2021
| Hospital | Functional Safety | Non-structural Safety | Structural Safety | Overall Safety |
|---|---|---|---|---|
| 1 | 4 (32.78%) | 10.05 (48.55%) | 3.25 (50%) | 17.3 (43.90%) |
| 2 | 4.3 (35.24%) | 12.9 (62.31%) | 5.5 (84.61%) | 22.7 (57.61%) |
| 3 | 3 (24.59%) | 13.8 (66.66%) | 5.25 (80.76%) | 22.05 (55.96%) |
| Overall | 3.76 (30.81%) | 12.25 (59.17%) | 4.66 (71.69%) | 20.68 (52.48%) |
The Safety Status of the Studied Hospitals in Functional, Non-structural, and Structural Dimensions, and the Overall Safety Level
Table 2 presents the safety levels of the studied hospitals across functional, non-structural, and structural dimensions, as well as the overall safety level for each hospital. Based on the number of answered questions in each dimension, the maximum scores for the three hospitals are as follows: 12.2 in the functional dimension, 20.7 in the non-structural dimension, and 6.5 in the structural dimension. The maximum score for overall safety was set at 39.4.
In functional safety, hospital 1 scored 4, hospital 2 scored 3.4, and hospital 3 scored 3 out of a possible 12.2. In non-structural safety, hospital 1 scored 10.05, hospital 2 scored 12.9, and hospital 3 scored 13.8 out of 20.7. In structural safety, hospital 1 scored 3.25, hospital 2 scored 5.5, and hospital 3 scored 5.25 out of 6.5. Regarding overall safety, hospital 1 scored 17.3, hospital 2 scored 22.7, and hospital 3 scored 22.05 out of 39.4.
The functional safety level is 32.78% for hospital 1, 35.24% for hospital 2, and 24.59% for hospital 3, placing all three in category C according to the WHO definition. In the non-structural safety dimension, hospital 1 achieved 48.55%, hospital 2 achieved 62.31%, and hospital 3 achieved 66.66%, categorized in B, B, and A respectively.
The structural safety levels are 50% for hospital 1, 84.61% for hospital 2, and 80.76% for hospital 3, each falling into categories B, A, and A respectively. The overall safety levels are 43.90% for hospital 1, 57.61% for hospital 2, and 55.96% for hospital 3, with all three hospitals placed in category B.
Regarding functional safety, the highest score is associated with hospital 2 and the lowest with hospital 3. In the non-structural safety dimension, the highest score is attributed to hospital 3, and the lowest to hospital 1. In terms of structural safety, the highest score is attributed to hospital 2, and the lowest to hospital 1. For overall safety, hospital 2 scored the highest, while hospital 1 scored the lowest.
The overall safety levels of the selected hospitals in Ahvaz city are 30.81% in the functional dimension, 59.17% in the non-structural dimension, 71.69% in the structural dimension, and 52.48% overall, categorized as C, B, A, and B respectively (19) (Table 3).
| Safety Level | Group Type | Necessary Actions |
|---|---|---|
| 0 - 0.35 | C | Immediate measures to support the lives of patients and personnel |
| 0.35 – 0.65 | B | Necessary measures in the short term to reduce damages |
| 0.66 - 1 | A | Preventive measures to maintain and improve safety |
Definition of Different Levels of Hospital Safety Based on the World Health Organization Guide
4.1. Results Related to the Most Significant Safety Challenges in the Functional, Non-structural, and Structural Dimensions, Separated by Their Components
The findings from the assessment of the most significant safety challenges facing disasters in three dimensions—functional, non-structural, and structural—in selected hospitals in Ahvaz during 2020 and 2021 are as follows:
In the functional safety assessment, it was observed that hospital 3 had not delegated specific responsibilities to the members of its Crisis Committee, nor had it provided a space for the emergency operations center (EOC). Meanwhile, hospital 2 was situated in a location deemed insecure and lacked an alternative communication system. Concerning the “operational plan to respond to internal and external risks,” none of the studied hospitals had defined a contingency plan for the activation and deactivation of operational plans. This includes the execution of payments to personnel, emergency purchasing of essentials within the first 72 hours following a disaster, allocation of necessary financial resources for emergency conditions, admission of patients in the emergency department, protection of patients' medical files, triage, resuscitation, registration, and treatment of patients, tracking of patients admitted and referred to other hospitals, transfer and admission to or from other hospitals, expansion of critical hospital services, epidemiological care system, preparation of a temporary storage place for corpses, provision of food for personnel in emergency situations, description of duties for auxiliary personnel and volunteers during emergencies, necessary measures to ensure their well-being and health, written agreements based on coordination with local crisis management, communication with media and public during emergencies, response to emergencies during evening, night, weekend, and holiday shifts, evacuation of the building, and regular drills and maneuvers.
In hospitals 1 and 3, there was no operational plan defining the necessary functions before, during, and after the occurrence of disasters that would cover critical areas of the hospital and determine space for capacity expansion. Regarding “probable plans for medical operations,” none of the studied hospitals had an operational plan for the treatment and psychosocial support of patients, families, and personnel in emergencies. The social work department was primarily focused on providing economic support to patients and offering counseling.
The evaluation of non-structural safety revealed that none of the studied hospitals had an alternative system for the local supply of electricity outside the hospital in terms of “electrical systems.”
Regarding the “electrical system” in the studied hospitals, an alternative communication system includes mobile phones, landline phones, paging devices, and intranet, which sometimes face internet disconnection issues. The lack of a wireless device was identified as a significant shortcoming. Hospital 1 was in poor condition regarding its internal communication system. The Panasonic TDE 600 paging device had very low quality and was not applied in newly-developed units. There is a unit where the hospital’s paging system will be interrupted if it breaks down. The “water storage system,” which should meet the hospital's needs for three days, has a much smaller capacity in hospital 3.
Regarding the “fuel distribution system,” the tanks had less than three days of reserve in hospitals 1 and 3. Regarding the “cooling, heating, and air conditioning systems,” the performance of heating, ventilating, and air conditioning (HVAC) system equipment, as well as the condition of pipes, connections, and valves, and strengthening of heating equipment in hospital 1 were poor. Regarding “office equipment,” the safety status of computers and printers in the studied hospitals was poor. In the dimension of “medical, laboratory, diagnostic, and treatment equipment,” the safety status of laboratory equipment in hospital 1 and the safety status of medical equipment in the sterilization department in hospital 2 were poor. Evaluating the structural safety of hospitals showed that in the area of “safety of the structural system and the type of materials used in the building,” hospital 1 was in a poor state regarding the connection of non-structural components to the structure and the redundancy of the structure.
5. Discussion
In the present study, all three hospitals were classified in group C (requires urgent measures to support the lives of patients and personnel) in terms of functional safety. In the non-structural and structural safety dimensions, the lowest scores were related to hospital 1, which can be attributed to the old structure and high cost to reduce structural and non-structural vulnerability, shortage of beds in normal status, the existence of old medical equipment and facilities with high depreciation, and shortage of easy-to-use medical equipment in times of crisis. Mohtadi stated that “the fifth round of accreditation report card, which is based on multiple axes of service delivery and 19 criteria, showed that this hospital could obtain the first accreditation rank” (20). Thus, this hospital should be re-evaluated to observe the principle of impartiality and fairness. In the overall safety dimension, all three hospitals were placed at level B (measures necessary in the short term to reduce damages), consistent with the study conducted in 35 hospitals in Gilan province (21).
Evaluating the functional safety showed that hospital 3 had the lowest score. The results of “each committee member's knowledge of his dedicated responsibilities” showed that responsibilities had been developed, but members in hospitals 1 and 2 were unfamiliar with them. This finding is consistent with the studies by Paganini et al. (22) and Mirzaei et al. (1). Regarding the “existence of a space for the EOC,” the results revealed that a space was designated for this purpose in hospital 1, but it was not active under normal conditions. However, a space was not designated in hospital 3. This finding aligns with studies conducted in Saudi Arabia (23) and Jordan (24). The safety status concerning the “deployment of the EOC in a protected and safe place” was low in hospital 2. However, in the study by Zaboli et al., 47.6% of respondents considered a safe and accessible place with complete facilities necessary for this center (25), which does not align with the results of this study and the reason for the difference could be the method of work.
In hospital 2, the operational plan developed to respond to high-probability risks was non-standard and had more of a documentary aspect. The lack of prior testing further reduced the guarantee of its operationalization during activation. Nonetheless, our country performs well in response levels, and international institutions also emphasize this (26). This is a reactive reaction, while globally there is a focus on prevention and reducing damage (27). The study's results showed “the lack of financial resources in emergencies,” consistent with the findings from selected hospitals in western Ethiopia (28). According to the head of financial affairs of the studied hospitals, no budget is allocated specifically for emergencies, and decisions are made on the spot. Hospitals 1 and 2 had considered places to increase admission capacity during crises. However, no accurate design and capacity measurement has been done for their use, consistent with the results of the study by Sadeghi et al. (29).
A significant point regarding the hospitals was the same processes in normal and emergency conditions. In dealing with unexpected events, the hospital faces different people, problems, and resources compared to normal daily activities. Thus, it is necessary to develop a system that is responsive and aware of the current challenges with a firm determination to solve them, paving the way for successful crisis management (5). The studied hospitals had no defined protocol for managing corpses in a mass casualty incident. The lack of a unique and equipped place for the mortuary of corpses and the lack of unprincipled and incorrect planning and predicting of needs in hospital 1 caused a shortage of mortuary facilities during the pandemic. This is not inconsistent with the results of a study by Al-Shareef et al. (23). The reason may be differences in the periods and the hospitals studied.
In the hospitals studied, cancelling leave and calling in on-call staff were among the strategies for increasing workforce, yet the operational plan to summon off-duty personnel was not anticipated. In contrast, a study in Canadian trauma centers reported that 39% of the centers had designed mechanisms to recruit and train additional staff as needed (30), which is inconsistent with the results of our study. This discrepancy can be attributed to differences in research tools and environments. In the studied hospitals, there was no guarantee that the space and welfare measures would meet the needs for more than 72 hours. However, Farabi Hospital in Tehran had developed an operational plan to ensure the welfare and health of auxiliary personnel and volunteers in emergencies (31), which did not align with the results of this study. This may be due to differences in times and hospitals studied. The safety status of the studied hospitals was reported as low regarding “the existence of written memorandums of coordination between the hospital and local competent authorities.” In Los Angeles, of the 45 hospitals studied, only 20% had written memorandums (32), which contrasts with the results of this study. This may relate to the materials and methods used.
In the study by Hosseini, the status of the 12 studied hospitals in terms of better informing and quickly and accurately communicating with the mass media, and the preparation and strengthening of external telecommunications systems, was considered moderate. Only the public relations departments of five hospitals in this study (42%) had completed preparatory courses in crisis conditions (33). This was inconsistent with our study results, possibly due to differences in materials and methods. The emergency evacuation process of the hospital is complex and challenging, with the transfer of patients and the continuity of providing medical services posing significant challenges, especially in the intensive care unit (34). However, the safety status of the studied hospitals in this area was evaluated as low. A study conducted in 10 Asian and Latin American countries revealed that 65% of hospital dysfunctions during the last four decades occurred following hazards (low intensity and high frequency) (35). The practical importance of this finding underscores the need to include such hazard scenarios in hospital preparedness exercises.
Based on an interview with a prominent professor in this field, several challenges were identified: The General Directorate of Accident and Disaster Management, primarily focused on pre-hospital services, lacks the necessary authority for decision-making in the area of treatment. There is also a lack of stringent follow-ups by the health policy-making council, and a weakness in continuously evaluating the performance of crisis committee secretaries due to the absence of a dedicated monitoring department at the headquarters. Furthermore, these evaluations are limited to the annual accreditation by the treatment deputy, which lacks experts specialized in this area. Additionally, there is insufficient monitoring of the performance of the crisis management departments in hospitals regarding the responsibilities of the pre-hospital incident management center. Finally, this department and its related issues are not prioritized by hospital managers. At the level of the Ministry of Health and the University, there is no disaster expert with recognized authority, and hospital managers tend to prioritize clinical issues and differential diagnoses over forming committees and developing preparedness, response, and recovery plans.
According to the statement from the fire department official at hospital 1, management neglects issues of disaster risk assessment and the development of plans and requirements to address it. The law mandates that one percent of the budget should be allocated to non-operational crisis defense. This oversight is due to the mindset of senior managers who typically allocate the budget towards the development of the hospital’s revenue-generating departments. As each physician assumes a management position, they begin to reconstruct and develop their service department since this increases their income. This situation has resulted in each department of the hospital operating without any standards. Even the municipality allows them to modify the interior decor according to their preference, although they cannot change the exterior structure. One of the criteria in the annual accreditation is to be fed from at least two urban power transmission networks so that one can be utilized in times of blackout (36). Due to the inefficiency and deterioration of the power input cable and the high wear of generators at hospital 1, it was decided to add another line from Bagh-e Moein with the cooperation of the Electricity Organization to increase the reliability factor. However, this issue has been overlooked in the other two hospitals due to the installation of new electricity cables. The lack of alternative communication systems and the poor state of internal communication systems in hospital 1 led to a low safety status, consistent with the findings of the study by Lapcevic et al. (3) and Irannejad et al. (37).
The results of a study by Ardalan et al. in Ahvaz teaching hospitals showed that the level of communication preparedness is moderate, and Imam Khomeini Hospital has a better status in the area of communication systems (38), which does not align with the results of the present study. This difference might be related to the tools used in the study. Koka et al. reported the existence of an alternative communication system in only three hospitals (12%), and it was found that standard communication systems (telephone, mobile), normal transportation routes, and infrastructure facilities are not capable of functioning normally in current unforeseen events (39). Since the first component in crisis planning is communication and information exchange among organizations and hospitals, developing guidelines for alternative communication in emergencies is crucial. Resources and facilities should be allocated to this area since poor communication causes a lack of coordination between organizations and multiplies the effects of the crisis by causing disorder and chaos (40). In the studied hospitals, the available water sources are intended for daily use and are not considered alternatives. A study in the Greek islands indicated that only half of the hospitals had water storage for at least three days, and lower-level health centers were less likely to have emergency water supplies (41).
The safety status of hospitals 1 and 3 regarding fuel reserves was reported to be at a low level. In a study by Chamani Cheraghtapeh et al. (31), fuel tanks had a reserve of 5 days or more, which is inconsistent with the results of this study. Although such resources should be considered during the construction of hospitals, experience suggests that the unforeseen events plan should provide for these alternative resources. Hospital managers should obtain the necessary information to evaluate and assess the state of these infrastructures and take the necessary measures while identifying potential weaknesses and planning corrections. Although the ventilation system in some departments was not as effective as expected in the studied hospitals, all departments were equipped with central heating, chillers, and ventilation systems. This was consistent with the results of a study by Rahmanian et al. at Farabi Hospital in Tehran. Studies suggest that 10% of nosocomial infections are airborne, and generally, 75% of microbes have the potential to be transmitted through the air. Thus, inadequate ventilation can increase the spread of diseases (42).
Poor maintenance, weak supervision, financial and workforce limitations, low-quality and worn-out parts, non-standard design of air blow and suction valves, high water salts, and technical defects may be the primary causes of poor performance of the HVAC system in the studied hospitals. Mirzaei et al. reported that all office equipment, including shelves, computers, and office furniture, was not in good condition in all the studied hospitals (1). This finding does not align with the results of this study. In the studied hospitals, one of the reasons for this challenge is the lack of a dedicated budget, neglect, and low priority given to the issue by hospital managers, and failure to estimate the project's cost of fixing office equipment and facilities by relevant experts.
The safety status of the studied hospitals in the structural dimension was estimated to be high based on the technical knowledge and experience of the structural engineer from the university and the impossibility of field studies due to the need for specialized investigations. Two studies conducted at Farabi Hospital in Tehran revealed that the structural safety of the hospital is at a moderate level, and it is not reasonable to expect uninterrupted and complete services during a crisis. Thus, renovation is recommended (31, 42). Severe damage to Heris Hospital after the Varzeghan earthquake, the inefficiency of the newly-built Sarpol Zahab Hospital after the Kermanshah earthquake, the explosion incident at the Sina Athar Clinic in Tehran, and the death of a significant number of people showed that the lack of structural and equipment safety and the lack of sufficient supervision and precision in the construction of new hospitals are too serious. Unfortunately, the quantitative measurement of structural safety in annual accreditations has not been taken very seriously for several years, and the opinions are not scientific (43).
Hospitals 1 and 2 are among the high-traffic referral hospitals of the province, and a serious decision needs to be taken to examine their structure to avoid imposing personal opinions. In hospitals 2 and 3, issues such as long construction time, which may be due to unrealistic budget estimates or inaccurate studies, the high level of groundwater and its impact on the foundation, and the lack of observance of maintenance standards can have severe impacts on the structure of these newly-built hospitals. The age of the hospital structure is not related to the quality of its medical services, and this reduces the motivation to spend many financial resources on renovation. The old age of hospitals leads to an increase in costs, a decrease in efficiency, and an increase in dissatisfaction among employees and patients. In a study in Iran, investment in the physical safety of hospitals led to significant improvements in this area and increased the mean score from 34 to 43 from 2012 to 2015 (15).
5.1. Conclusions
The results revealed that the safety of the studied hospitals in the functional, non-structural, and structural dimensions was low, moderate, and high, respectively. Also, the overall safety of the above hospitals was evaluated at a moderate level. However, according to some experts, even 99% preparedness is insufficient to cope with such incidents. Thus, it is recommended to assess the safety level of hospitals annually using the hospital safety tool of the WHO. Holding continuous training courses regarding safety standards for all managers and employees, paying particular attention to the results of annual accreditation and safety issues, and allocating sufficient funds to develop an operational plan to improve safety in the functional, non-structural, and structural dimensions are among other solutions recommended for the mentioned hospitals.