1. Background
Maternal near miss (MNM) is defined as any life-threatening event during pregnancy, delivery, or within six weeks after the termination of pregnancy, where a woman narrowly survives but sustains severe complications (1). The World Health Organization (WHO) outlines three steps to address MNM: Baseline assessment of the life-threatening condition, analysis of the situation, and interventions to improve healthcare (2). A WHO systematic review encompassing 30 studies reported that the prevalence of MNM ranged from 0.38% to 8.23% in studies using disease-specific criteria for diagnosis, and was significantly lower in studies utilizing organ failure as criteria (3). Women who have cesarean sections or receive less prenatal care face a higher risk of MNM (4).
Recent research indicates that the prevalence of MNM is 18.67 per 1000 live births, with a higher prevalence observed in low- and middle-income countries (5). A systematic review of 12 articles found that, in Iran, the ratio of overall life-threatening conditions according to WHO criteria was 1.63 per 1000 live births. It has also been determined that potential life-threatening events exceed the instances of MNM (6). Another study in Iran reported a MNM prevalence of 20.6%, which was linked to the duration of labor and the number of prenatal care visits (7). Women with severe obstetric complications during childbirth were found to have lower emotional well-being and a higher incidence of postpartum depression (8).
Women with MNM are at increased risk of diminished quality of life and reduced cognitive function (9). Evidence indicates that women with MNM are more likely to undergo cesarean sections and suffer from previous pathological conditions. Additionally, these women are at higher risk of dyspareunia and delayed onset of sexual activity compared to their healthy counterparts (10). A study by Norhayati and Azman Yacob found that women who experienced severe maternal morbidity (SMM) were significantly older and underwent more cesarean sections, but did not exhibit more sexual dysfunction than healthy women (11). In a cross-sectional study of 110 women with SMM, Alves et al. reported that women with SMM experienced more dyspareunia than those without SMM (12). The rate of cesarean sections in Iran is significantly higher than in other countries, with most MNM cases occurring during the second cesarean section (13, 14).
2. Objectives
Due to the lack of studies on the sexual function of women with MNM in Iran, this study was conducted to compare the sexual function of women with and without MNM in Ahvaz, Southwest of Iran.
3. Methods
This comparative cross-sectional study recruited women with MNM (n = 140) from two educational hospitals in Ahvaz, Iran in 2020, and compared them with a control group of women without MNM (n = 246).
3.1. Inclusion/Exclusion Criteria
Women with MNM and basic literacy who had given birth at least 8 - 12 weeks prior to the study were eligible. According to WHO criteria, life-threatening conditions such as cardiovascular, respiratory, renal, blood and coagulation disorders, liver, and neurological issues, along with severe maternal complications (severe postpartum hemorrhage, severe preeclampsia, eclampsia, sepsis or severe systemic infection, and uterine rupture) occurring during pregnancy up to 42 days post-delivery were classified as MNM (3).
Women with known psychological disorders such as severe depression, stress, and anxiety, who required medication, were excluded from the study (these criteria were verified through self-report). The study design was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Ref. ID: IR.AJUMS.REC.1399.426). All eligible women signed informed written consent before the commencement of data collection.
3.2. Sample Size
The sample size was calculated to be 272 (136 women in each group) based on the findings of a previous study (15), using MedCalc statistical software with an 80% power and a 5% error margin. Accordingly, the software determined a sample size of 272 cases (136 in each group). We recruited 140 women with MNM and 246 women without MNM.
µ1 = 24.39, SD1 = 8.02, µ2 = 22.87, SD2 = 8.47, α1 = 0.05, Z1-α/2 = 1.96, β = 0.2, Zβ = 1.28.
3.3. Setting
We recruited all women with MNM (n = 140) from two educational hospitals (Imam Khomeini and Taleghani) in Ahvaz in 2020. These hospitals were selected because they handle nearly all cases with potential complications in labor or delivery in Ahvaz. Additionally, 246 women without MNM who were admitted to two health centers were chosen as the control group. Women in the control group had delivered their babies without any complications and visited public health centers for postnatal check-ups and vaccinations for their newborns. Data collection began in December 2020 and was completed in March 2021.
3.4. Measures
A demographic questionnaire that included questions about age, age at marriage, educational attainment, occupation, number of children, mode of delivery, spouse's educational attainment and occupation, and economic status was used to collect demographic data. The content validity of this questionnaire was evaluated by presenting it to six faculty members and revising it based on their recommendations.
The Female Sexual Function Index (FSFI) was used to assess the sexual function of participants over the past month. The FSFI comprises 19 questions across six components: Sexual desire (two questions), sexual arousal (four questions), lubrication (four questions), pain (three questions), sexual satisfaction (three questions), and orgasm (three questions). To calculate the total score for each domain, the scores for sexual desire, arousal, lubrication, orgasm, sexual satisfaction, and pain were multiplied by factors of 0.6, 0.3, 0.3, 0.4, 0.4, and 0.4, respectively. The total FSFI score ranges from zero to 36, with scores below 26 indicating sexual dysfunction. The validity and reliability of this questionnaire were established by Rosen et al. (16) and further confirmed in Iran by Fakhri et al. (17).
3.5. Procedure
All eligible women with and without MNM were contacted by phone and invited to visit a public health center to complete the demographic questionnaire and FSFI. Researcher SD was available to answer any questions from the participants. Women without MNM were recruited from two public health centers in Ahvaz. Due to the COVID-19 pandemic, all necessary hygiene measures, including the use of face masks and social distancing, were strictly enforced.
3.6. Variables
In this study, MNM was the independent variable and sexual function was the dependent variable. Confounding variables included age, mode of delivery, educational attainment, economic status, and number of deliveries.
3.7. Statistical Analysis
Data were analyzed using SPSS version 22. The Shapiro-Wilk test was employed to check for the normal distribution of continuous data. The independent t-test was used to compare numerical data between the two groups, while the chi-square test was used for categorical data. Linear regression was utilized to evaluate the relationships between sexual function, near-miss incidents, and demographic factors. A P-value of less than 0.05 was considered statistically significant.
4. Results
Table 1 presents the demographic characteristics of the participants. It is clear from the table that the women and their husbands in the MNM group were significantly older than those in the control group. Additionally, women in the MNM group had significantly higher gravidity, and 70% of them underwent cesarean sections (P < 0.05). The most common causes of MNM were preeclampsia (41.43%), followed by placenta accreta (24.29%), and then hypertension and diabetes (17.86%).
| Variables | Women with MNM (n = 140) | Women Without MNM (n = 246) | P-Value |
|---|---|---|---|
| Age (y) | 30.7 ± 6.45 | 27.7 ± 6.62 | < 0.001 b |
| Age of husband (y) | 33.25 ± 6.9 | 31.15 ± 6.8 | 0.004 b |
| Number of deliveries | 2.42 ± 1.40 | 2.01 ± 1.17 | 0.002b |
| Occupation | 0.83 c | ||
| Housewife | 129 (92.1) | 229 (93.1) | |
| Employee | 11 (7.9) | 17 (6.9) | |
| Education | 0.007 c | ||
| Primary | 48 (34.3) | 58 (23.6) | |
| High school | 29 (20.7) | 89 (36.2) | |
| Secondary high school | 44 (31.4) | 76 (30.9) | |
| University degree | 19 (13.6) | 23 (9.3) | |
| Education of husband | 0.35 c | ||
| Primary | 43 (30.7) | 69 (28) | |
| High school | 43 (30.7) | 88 (35.8) | |
| Secondary high school | 40 (28.6) | 75 (30.5) | |
| University degree | 14 (10) | 14 (5.7) | |
| Mode of delivery | 0.007 c | ||
| Normal vaginal delivery | 42 (30) | 109 (44.3) | |
| Cesarean section | 98 (70) | 135 (54.9) | |
| Economic status | 0.01 c | ||
| Weak | 49 (35) | 62 (25.2) | |
| Moderate | 75 (53.6) | 125 (50.8) | |
| Good | 16 (11.4 | 56 (22.8) | |
| Causes of near miss | |||
| Hypertension and diabetes | 25 (17.86) | - | |
| Heart disease | 10 (7.14) | - | |
| Placenta accreta/hemorrhage | 34 (24.29) | - | |
| Preeclampsia | 58 (41.43) | - | |
| Uterine atony/rupture of uterus and cervix | 8 (5.71) | - | |
| Ruptured ectopic pregnancy | 5 (3.57) | - |
Demographic Characteristics of Participants with and Without Maternal Near Miss a
Table 2 displays the scores for different sexual function domains in the groups with and without MNM. According to the table, women with MNM had significantly lower scores in sexual desire, sexual arousal, lubrication, orgasm, sexual satisfaction, and overall sexual function (P < 0.0001). Although pain was more prevalent in the MNM group, the difference between the two groups was not statistically significant (P = 0.864).
| Variables | Women with MNM (n = 140) | Women Without MNM (n = 140) | P-Value b |
|---|---|---|---|
| Sexual desire | 3.24 ± 0.91 | 3.75 ± 1.05 | 0.0001 |
| Arousal | 3.04 ± 1.51 | 3.73 ± 1.39 | 0.0001 |
| Lubrication | 2.48 ± 1.36 | 3.37 ± 1.33 | 0.0001 |
| Orgasm | 3.52 ± 1.97 | 4.12 ± 1.51 | 0.001 |
| Satisfaction | 3.78 ± 1.77 | 4.42 ± 1.6 | 0.0001 |
| Pain | 3.97 ± 1.83 | 3.95 ± 1.65 | 0.864 |
| Total score of sexual function | 20.05 ± 8.21 | 23.27 ± 6.84 | 0.0001 |
Sexual Function of Women in the Maternal Near Miss and Control Groups Before Intervention a
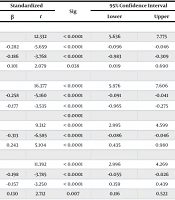
Table 3 depicts the relationship between sexual function, MNM, and demographic factors. This table shows that older women had significantly lower scores in the following components: Sexual satisfaction (β = -0.071, 95% CI: -0.096, -0.046, P < 0.0001), orgasm (β = -0.066, 95% CI: -0.091, -0.041, P < 0.0001), lubrication (β = -0.066, 95% CI: -0.086, -0.046, P < 0.0001), arousal (β = -0.043, 95% CI: -0.055, -0.026, P < 0.0001), sexual desire (β = -0.040, 95% CI: -0.055, -0.026, P < 0.0001), and overall sexual function (β = -0.352, 95% CI: -0.459, -0.244, P < 0.0001). Conversely, women without MNM had significantly higher scores in sexual satisfaction (β = 0.355, 95% CI: 0.019, 0.690, P = 0.035), lubrication (β = 0.707, 95% CI: 0.435, 0.980, P <0.0001), sexual arousal (β = 0.394, 95% CI: 0.116, 0.522, P = 0.007), sexual desire (β = 0.319, 95% CI: 0.116, 0.522, P = 0.002), and total sexual function (β = 1.768, 95% CI: 0.306, 3.230, P = 0.018).
| Variables | Unstandardized | Standardized | Sig | 95% Confidence Interval | |||
|---|---|---|---|---|---|---|---|
| β | Standard Error | β | t | Lower | Upper | ||
| Sexual satisfaction | |||||||
| Constant | 6.706 | 0.544 | 12.332 | < 0.0001 | 5.636 | 7.775 | |
| Age of participants | -0.071 | 0.013 | -0.282 | -5.659 | < 0.0001 | -0.096 | -0.046 |
| Mode of delivery | -0.646 | 0.172 | -0.186 | -3.768 | < 0.0001 | -0.983 | -0.309 |
| Near miss | 0.355 | 0.171 | 0.101 | 2.079 | 0.038 | 0.019 | 0.690 |
| Orgasm | |||||||
| Constant | 6.791 | 0.415 | 16.377 | < 0.0001 | 5.976 | 7.606 | |
| Age, female | -0.066 | 0.013 | -0.258 | -5.160 | < 0.0001 | -0.091 | -0.041 |
| Mode of delivery | -0.620 | 0.175 | -0.177 | -3.535 | < 0.0001 | -0.965 | -0.275 |
| Lubrication | < 0.0001 | ||||||
| Constant | 3.797 | 0.408 | 9.312 | < 0.0001 | 2.995 | 4.599 | |
| Age, female | -0.066 | 0.010 | -0.313 | -6.585 | < 0.0001 | -0.086 | -0.046 |
| Near miss | 0.707 | 0.139 | 0.243 | 5.104 | < 0.0001 | 0.435 | 0.980 |
| Arousal | |||||||
| Constant | 5.280 | 0.464 | 11.392 | < 0.0001 | 2.996 | 4.269 | |
| Age, female | -0.043 | 0.011 | -0.198 | -3.785 | < 0.0001 | -0.055 | -0.026 |
| Mode of delivery | -0.473 | 0.146 | -0.157 | -3.250 | < 0.0001 | 0.159 | 0.439 |
| Near miss | 0.394 | 0.146 | 0.130 | 2.712 | 0.007 | 0.116 | 0.522 |
| Sexual desire | |||||||
| Constant | 3.633 | 0.324 | 11.216 | < 0.0001 | 2.996 | 4.269 | |
| Age, female | -0.040 | 0.007 | -0.263 | -5.464 | < 0.0001 | -0.055 | -0.026 |
| Economic status | 0.299 | 0.071 | 0.200 | 4.197 | < 0.0001 | 0.159 | 0.439 |
| Near miss | 0.319 | 0.103 | 0.150 | 3.096 | 0.002 | 0.116 | 0.522 |
| Total score of sexual function | |||||||
| Constant | 34.490 | 2.378 | 14.504 | < 0.0001 | 29.813 | 39.166 | |
| Age, female | -0.352 | 0.055 | -0.313 | -6.419 | < 0.0001 | -0.459 | -0.244 |
| Mode of delivery | -3.181 | 0.750 | -0.205 | -4.243 | < 0.0001 | -4.655 | -1.707 |
| Near miss | 1.768 | 0.744 | 0.114 | 2.377 | 0.018 | 0.306 | 3.230 |
The Relationship of Sexual Function and Its Components with Maternal Near Miss and Demographic Variables Using Linear Regression
Women who had undergone cesarean sections reported lower sexual satisfaction (β = -0.646, 95% CI: -0.983, -0.309, P < 0.0001), orgasm (β = -0.620, 95% CI: -0.965, -0.275, P < 0.0001), sexual arousal (β = -0.473, 95% CI: -0.159, -0.439, P = 0.001), and overall score of sexual function (β = -3.181, 95% CI: -4.655, -1.707, P < 0.0001).
5. Discussion
This study aimed to evaluate sexual function in women with and without MNM. The results revealed that the most prevalent causes of MNM were preeclampsia, placenta accreta, hypertension, and diabetes. According to the WHO, these conditions are similar to those that cause maternal mortality, including hemorrhage, hypertensive disorders, sepsis, and obstructed labor (18). In our study, placenta accreta and hemorrhage, often associated with previous cesarean sections, were the second most common causes of MNM. A study by Kasraeian et al. on 198 women with placenta accreta, with an average gestational age of 26 weeks, found that 163 of these women underwent hysterectomies and the average blood loss during surgery was 2446 mL (19).
Our findings showed that 80.7% of women with MNM experienced sexual dysfunction, compared to 68.4% of women without MNM. This rate of sexual dysfunction is much higher than in other studies. For instance, a cross-sectional study by Alves et al. on 110 women, both with and without SMM, reported that 44.5% of participants experienced sexual dysfunction, including 48.7% of those who had SMM (12). The higher rate of sexual dysfunction in our study, compared to Alves et al.'s findings (12), may be attributed to the generally lower sexual function of Iranian women in the postpartum period, as indicated by Rezaei et al., where approximately 76.3% of Iranian women experienced sexual dysfunction during this time (20).
Additionally, the present study indicated that scores for all sexual function domains, except for pain, were lower in women with MNM compared to those without. Although the MNM group reported higher pain levels, the difference was not statistically significant. This may be because, in Iran, more than 50% of primiparous women undergo episiotomy during delivery, resulting in a low rate of severe lacerations (21).
Norhayati and Azman Yacob conducted a study involving 145 women with SMM and 187 women without SMM. They discovered that women with SMM were significantly older and more likely to have undergone cesarean sections. However, after adjusting for demographic variables, there was no significant difference in sexual function between the two groups (11). Our findings diverge from those of Norhayati and Azman Yacob (11), as we observed that women with MNM and those who had undergone cesarean sections exhibited significantly lower sexual function. This discrepancy may be attributed to the higher rate of cesarean sections in Iran compared to other countries, coupled with the likelihood that women who have one cesarean section will often require the procedure in subsequent pregnancies. Not surprisingly, the rate of complications in recurrent cesarean sections is much higher. In our study, 70% of the women in the MNM group had undergone a cesarean section.
Ferreira et al. conducted a study on 384 women with SMM and 419 women without, finding that although the quality of life was significantly lower in the SMM group, sexual function remained similar between the two groups (22). Additionally, von Rosen et al. carried out a systematic review involving 15 studies and 31 559 participants, both with and without MNM. They found that MNM led to a lower quality of life and negative economic consequences but was not associated with sexual dysfunction (9). This discrepancy might again be related to the generally lower postpartum sexual function among Iranian women compared to their counterparts in developed countries.
5.1. Strengths and Limitations of the Study
This is the first Iranian study to assess sexual function in women with MNM. Despite its strengths, the study has several limitations. First, the participants were not recruited randomly; therefore, they do not represent all women with MNM, affecting the generalizability of the results. Second, discussing sexual issues is considered taboo in Iranian culture, which may have influenced the women's candor in expressing their experiences. Finally, participants were enrolled 8 - 12 weeks post-delivery, which might be too soon for them to have recovered from complications such as episiotomies and to have resumed sexual activity. Further studies with longer post-delivery periods are needed to evaluate sexual function in women with MNM more accurately.
5.2. Conclusions
The results of this study indicate that all components of sexual function, except for pain, were lower in women with MNM compared to those without. A significant number of women who had undergone cesarean sections experienced both MNM and sexual dysfunction. Health policymakers should focus more attention not only on the causes of MNM, particularly cesarean sections, but also on assessing the sexual function of women with MNM.