1. Background
Self-care encompasses learned, conscious, and purposeful actions performed by individuals for themselves, their children, and families to stay healthy, maintain good mental and physical health, meet social and psychological needs, prevent diseases or accidents, provide care for chronic illnesses, and support health after an acute illness or hospital discharge (1, 2). The most important health-promoting self-care behaviors include healthy eating, physical activity, stress management, interpersonal communication, spiritual growth, and taking responsibility for one's health (3, 4).
Self-care plays a crucial role in improving the national health system (1, 5). To reduce the burden on health systems, individuals need to adopt self-care behaviors (6). Studies indicate that about three-quarters of medical visits are unnecessary (2, 7), and self-care can address individuals' problems. Evidence from the UK shows that self-care support can reduce general practitioner visits by up to 40%, outpatient visits by up to 17%, and days of absence from work by 50% (2, 7).
Several factors influence individuals' self-care behavior. Studies indicate that age, social class (8), gender, literacy level (9), and individuals' attitudes and beliefs can significantly impact the adoption of self-care behaviors (10, 11). Previous studies on self-care have highlighted its unfavorable condition in Iran (12). However, in the present study, the average self-care behavior is higher in women than in men and higher in married employees than in single employees. Additionally, higher levels of education and economic status correlate with higher average self-care behavior. Teaching a healthy lifestyle and self-care is an appropriate and efficient way to achieve health and prevent disease (13, 14). People have the ability to take care of themselves and can be supported through direct compensatory and educational-supportive care whenever their ability is impaired, helping to restore their capacity for self-care. Creating health and self-care behavior is at the core of education and health promotion programs (15). Health education experts believe that choosing a model for health education is the first step in the "design or development" of educational interventions, ensuring that the program starts in the right direction and stays on track. The Health Belief Model (HBM), selected as the educational framework for the present study, is a highly accurate model specifically designed for health-related behaviors and is instrumental in developing and designing preventive programs.
This model includes six constructs: Perceived susceptibility, perceived severity, perceived benefits, perceived barriers, perceived self-efficacy, and cues to action. These constructs are defined as follows: (1) perceived susceptibility: A person's belief about the likelihood of contracting a disease or experiencing a harmful state as a result of certain behaviors; (2) perceived severity: A person's belief about the extent of harm that can be caused by an illness or harmful condition resulting from specific behaviors; (3) perceived benefits: Beliefs about the advantages of the proposed methods for reducing the risk or severity of the disease or harmful state caused by particular behaviors; (4) perceived barriers: Beliefs about the actual and perceived costs of adopting a new behavior; (5) perceived self-efficacy: Confidence in one's ability to successfully perform a behavior; (6) cues to action: Triggers or forces that prompt the individual to take action (16, 17). Studies on self-care primarily focus on medicine and patients (2, 18); however, little attention is paid to self-care in healthy individuals who have not yet become ill. This is especially true for health workers who are expected to model a healthy lifestyle in society and provide self-care training at individual, organizational, and social levels according to the executive instructions of health education and promotion programs. Given that the HBM is a comprehensive model widely used for disease prevention, it effectively focuses on individual motivation for action (17, 19).
2. Objectives
The present study aimed to determine the effect of training based on the HBM on the adoption of self-care behaviors, including physical activity, nutrition, spiritual growth, interpersonal relationships, health responsibility, and stress management, among health staff at comprehensive health centers in Rudbar city, Gilan.
3. Methods
3.1. Design, Procedure and the Study Sample
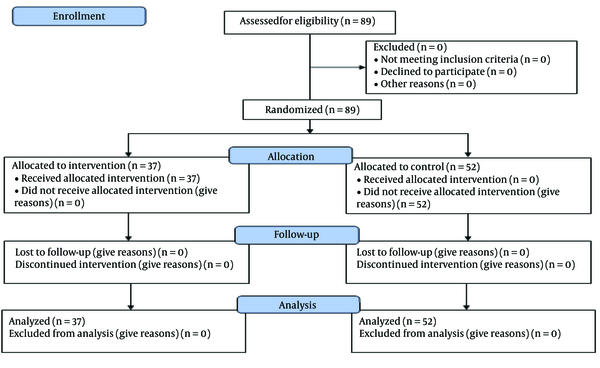
In the present quasi-experimental study, the research population consisted of health workers (midwives and healthcare providers) from comprehensive urban health service centers in Rudbar city, Gilan, Iran. Using a cluster randomized sampling method, all 7 comprehensive urban health centers in Rudbar were listed and each center was assigned a number from 1 to 7. In the next step, half of the centers (Rudbar, Manjil, and Rostamabad) were randomly assigned to the intervention group, and the other half (Lowshan, Barehsar, Jirandeh, and Tutkabon) were assigned to the control group. Due to the low sample size, all workers of comprehensive health centers who met the inclusion criteria (N = 37 for the intervention group and N = 52 for the control group) were included in the study (Figure 1). The inclusion criteria consisted of employment in the health field in comprehensive urban health services centers of Rudbar during the implementation of the project, at least one year of work experience, and signing a written consent form to participate in the study. The exclusion criteria were incomplete questionnaires and non-participation in at least one training session.
3.2. Measures
The data collection tool included three questionnaires: (1) Demographic Information Questionnaire: This included age, gender, work experience, education level, marital status, and economic status; (2) HBM Questionnaire: This was prepared based on related similar studies (20-23) with minor modifications (Table 1). The content validity of the questionnaire was confirmed by 9 faculty members from medical sciences universities with expertise in health education (4 members), nutrition (1 member), social medicine (2 members), and epidemiology (2 members). Its reliability was determined by testing it on 12 residents of comprehensive urban health centers who were not part of the main study. Validity results showed a content validity index of 0.73 for the entire questionnaire. Cronbach's alpha coefficients were 0.68 for perceived sensitivity, 0.81 for perceived severity, 0.76 for perceived benefits, 0.76 for perceived barriers, and 0.78 for guides for action; (3) Self-Efficacy Questionnaire: To measure perceived self-efficacy, the self-rated abilities for health practice (SRAHPS) was used. This tool was initially designed by Becker et al. in 1993 (24). The content validity and reliability of the questionnaire were evaluated and confirmed by Tanjani et al. in Iran (25). In the present study, the reliability of the questionnaire was confirmed with a Cronbach's alpha coefficient of 0.73; (4) Self-Care Questionnaire: The Health-Promoting Behavior Index II was used to measure health-promoting self-care behaviors (26). The validity and reliability of the tool were confirmed by Mohammadi et al. in Iran (27). In the current study, the reliability of the self-care questionnaire was confirmed with Cronbach's alpha coefficients of 0.84 for physical activity, 0.79 for a healthy diet, 0.81 for spiritual growth, 0.71 for interpersonal relationships, 0.82 for health responsibility, and 0.81 for stress management (Table 1).
| Variables | Number of Questions | Acquired Values | |
|---|---|---|---|
| Minimum | Maximum | ||
| Constructs of Health Belief Model | |||
| Perceived susceptibility | 3 | 3 | 15 |
| Perceived severity | 6 | 6 | 30 |
| Perceived benefits | 5 | 5 | 25 |
| Perceived barriers | 5 | 5 | 25 |
| Guides for action | 4 | 4 | 20 |
| Perceived self-efficacy | 28 | 28 | 140 |
| Dimensions of self-care behavior | |||
| Nutrition | 9 | 9 | 36 |
| Physical activity | 8 | 8 | 32 |
| Responsibility for health | 9 | 9 | 36 |
| Stress management | 8 | 8 | 32 |
| Interpersonal relationships | 9 | 9 | 36 |
| Spiritual growth | 9 | 9 | 36 |
Acceptable Values of Health Belief Model Constructs and Dimensions of Self-Care Behavior in Research Questionnaires
3.3. Intervention
In the educational program, greater emphasis was placed on the structures with a low mean score in the HBM, except for the structure of perceived barriers, where a higher score was considered. To increase perceived sensitivity, available statistics and risk factors associated with not performing self-care behaviors were noted. To increase perceived severity, the number of deaths due to not adopting self-care behaviors was mentioned. To highlight perceived benefits, the advantages of health-promoting self-care behaviors were discussed, and employees were given the opportunity to discuss barriers to the use of these behaviors. To enhance self-efficacy, methods to increase the ability to successfully perform self-care behaviors and successful experiences of employees in maintaining health were shared.
The educational methods used in the training sessions included a combination of lectures, question and answer sessions, group discussions, and brainstorming. Additionally, short videos about the benefits of self-care behaviors and the consequences of not engaging in them were shown, along with educational slides (PowerPoint) and pamphlets. After selecting the participants, stating the research objectives, and obtaining the written consent forms, the pre-test questionnaire was completed by both the intervention and control groups. Following the analysis of the pre-test data, the educational intervention was designed based on the HBM.
One week after the pre-test, the training program was conducted exclusively for the intervention group, consisting of five training sessions lasting 60 to 75 minutes each, facilitated by the researcher (a master's student in health education). Meetings were held twice a week with intervals of 3 to 4 days. The educational content of the sessions focused on the dimensions of self-care behaviors and employed a combination of training methods aligned with HBM constructs.
To address perceived susceptibility and severity, the training utilized speeches, statistical presentations in educational slides, and short film screenings. Group discussions were held to influence the perceived benefits construct, while brainstorming, group discussions, questions and answers, and addressing real or imagined obstacles by employees were used to target the perceived barriers construct. After a speech, group discussion, and finally a question-and-answer session were used to enhance the employees' self-efficacy. Questionnaires were completed for both groups three months after the training intervention to evaluate the effect of the training program (27).
3.4. Data Analysis
All data were analyzed using SPSS software version 21.0 (IBM Corp., Armonk, NY). Data are presented as frequency and percentage or mean and standard deviation. To compare qualitative characteristics between groups, the chi-square test was used. The Kolmogorov-Smirnov test indicated that most of the quantitative outcomes were not normally distributed. Therefore, the Mann-Whitney U test was performed to compare the quantitative measurements between groups. A P-value lower than 0.05 was considered statistically significant. Trial registration number: IRCT20191023045204N1. Registered 2019/12/03.Ethics approval and consent to participate;
all participants were informed about the study and confidentiality protocols. Written informed consent was obtained from all participants. Guilan University of Medical Sciences (IR.GUMS.REC.1398.240) confirmed the morality and ethics of this study.
4. Results
The age range of most participants (43%) was 30 - 39 years, with 86% being female and 13.5% male. The economic situation of most employees participating in the study was moderate (69%). Job status for most employees was contracted (41%). The level of education for most employees was a bachelor's degree (73%). The chi-square test indicated that both intervention and control groups were comparable on demographic characteristics (gender, marital status, education level, job status, economic status, age, and work experience) and there were no significant differences between the two groups at pretest (Table 2). Additionally, there were no differences between groups on the outcomes measured at pretest, including all constructs of the HBM and aspects of health-promoting self-care behavior (P > 0.05) (Table 3).
| Variables | Intervention Group (N = 37) | Control Group (N = 52) | P-Value |
|---|---|---|---|
| Gender | 0.924 | ||
| Female | 32 (86.5) | 45 (86.5) | |
| Male | 5 (13.5) | 7 (13.5) | |
| Marital status | 0.628 | ||
| Unmarried | 11 (29.7) | 18 (34.6) | |
| Married | 26 (70.3) | 34 (65.4) | |
| Education | 0.892 | ||
| Associate degree | 8 (21.6) | 10 (19.2) | |
| Bachelor | 27 (73) | 38 (73.1) | |
| Master's degree | 2 (5.4) | 4 (7.7) | |
| Job status | 0.971 | ||
| Design period | 9 (24.8) | 13 (25) | |
| Contractual | 15 (41.5) | 22 (42.3) | |
| Employment | 13 (33.7) | 17 (32.7) | |
| The economic situation | 0.545 | ||
| Weak | 3 (8.1) | 3 (5.8) | |
| Medium | 27 (73) | 34 (65.4) | |
| Good or great | 7 (18.9) | 15 (28.8) | |
| Age (y) | 0.481 | ||
| 20 - 29 | 10 (27.1) | 22 (42.3) | |
| 30 - 39 | 19 (51.3) | 20 (38.5) | |
| 40 - 49 | 5 (13.5) | 9 (17.3) | |
| 50 - 59 | 3 (8.1) | 1 (1.9) | |
| Work experience (y) | 0.285 | ||
| 0 - 10 | 21 (56.7) | 40 (77) | |
| 11 - 20 | 12 (32.4) | 6 (11.5) | |
| 21 - 30 | 4 (10.8) | 6 (11.5) |
Demographic Characteristics of the Employees Studied in the Control and Intervention Group a
| Dimensions of Self-Care Behavior | Intervention Group | Control Group | P-Value of Between Groups Comparison | |||||
|---|---|---|---|---|---|---|---|---|
| Before Intervention | After the Intervention | P-Value | Before Intervention | After the Intervention | P-Value | Before Intervention | After the Intervention | |
| Nutrition | 24.1 ± 4.85 | 27.67 ± 3.27 | 0.001 | 23.86 ± 3.71 | 23.82 ± 3.69 | 0.157 | 0.701 | 0.010 |
| Physical activity | 16.51 ± 4.42 | 19.78 ± 4.45 | 0.001 | 17.19 ± 4.45 | 17.07 ± 4.33 | 0.182 | 0.296 | 0.005 |
| Responsibility for health | 22.24 ± 4.41 | 25.56 ± 4.15 | 0.001 | 22.38 ± 4.01 | 22.32 ± 3.95 | 0.180 | 0.491 | 0.010 |
| Stress management | 22.24 ± 4.41 | 25.56 ± 4.15 | 0.001 | 22.38 ± 4.01 | 22.32 ± 3.95 | 0.180 | 0.710 | 0.010 |
| Interpersonal relationships | 23.35 ± 4 | 26.08 ± 3.15 | 0.001 | 23.71 ± 3.75 | 23.67 ± 3.72 | 0.159 | 0.312 | 0.010 |
| Spiritual growth | 24.27 ± 5.02 | 27.82 ± 3.81 | 0.001 | 25.28 ± 4.19 | 25.30 ± 4.17 | 0.659 | 0.302 | 0.004 |
| Self-care behavior | 128.4 ± 22.73 | 148.37 ± 18.27 | 0.001 | 131.76 ± 19.9 | 131.42 ± 19.61 | 0.180 | 0.176 | < 0.001 |
Comparison of Mean Scores of Health Belief Model Constructs in the Intervention and Control a
As shown in Table 3, three months after the designed educational intervention, the mean scores of the constructs of the HBM (perceived sensitivity, perceived severity, perceived self-efficacy, and cues to action) except for perceived benefits improved significantly in the intervention group compared to the control group. Additionally, three months after the training, the mean score of all aspects of health-promoting self-care behavior (physical activity, spiritual growth, healthy diet, stress management, health responsibility, and interpersonal relationships) in the intervention group was significantly higher than in the control group (P < 0.05, Table 4). The average score of self-care behavior in the intervention group increased from 128.4 before the intervention to 148.37 after the intervention.
| Constructs of Health Belief Model | Intervention Group | P-Value | Control Group | P-Value | P-Value of Between Groups Comparison | |||
|---|---|---|---|---|---|---|---|---|
| Before Intervention | After the Intervention | Before Intervention | After the Intervention | Before Intervention | After the Intervention | |||
| Perceived susceptibility | 9 ± 3.35 | 11.27 ± 2.65 | 0.001 | 7.96 ± 3.59 | 8.17 ± 3.39 | 0.481 | 0.192 | < 0.001 |
| Perceived severity | 20.35 ± 5.77 | 22.7 ± 4.98 | 0.03 | 19.8 ± 6.05 | 19.69 ± 5.63 | 0.514 | 0.811 | 0.010 |
| Perceived benefits | 20.51 ± 2.97 | 21.1 ± 3.19 | 0.173 | 20.28 ± 2.93 | 20.25 ± 2.2 | 0.592 | 0.986 | 0.183 |
| Perceived barriers | 14.67 ± 3.87 | 12.45 ± 3.47 | 0.001 | 14.75 ± 4.49 | 14.51 ± 4.18 | 0.998 | 0.917 | 0.030 |
| Perceived self-efficacy | 93.81 ± 16.84 | 105.89 ± 14 | 0.001 | 97.53 ± 14.81 | 97.21 ± 15.09 | 0.215 | 0.272 | 0.007 |
| Guides for action | 14.72 ± 2.23 | 15.43 ± 1.95 | 0.04 | 14.92 ± 3.02 | 14.90 ± 2.83 | 0.682 | 0.426 | 0.001 |
Comparison of the Mean Scores of the Dimensions of Self-Care Behavior Promoting Health in the Intervention and Control Group Before and After the Training Intervention in the Study Staff a
5. Discussion
The results of the present study, which aimed to determine the effect of an educational intervention based on the HBM on adopting self-care behaviors among health workers, indicated that the training program improved dimensions of self-care behavior in the intervention group based on constructs of the HBM.
In this study, the mean scores of self-care behavior in the intervention group showed a significant increase after the training program, with notable improvements seen in self-care behaviors such as a healthy diet, physical activity, stress management, health responsibility, spiritual growth, and interpersonal relationships compared to the control group. The research results were consistent with several studies in which training based on the HBM was able to increase mean self-care behavior (2, 28-30). In a study by Torshizi et al. (31), training had no effect on calcium intake to prevent osteoporosis, likely due to the individuals' economic status. Similarly, Anderson et al. (32) indicated that despite providing necessary information to pregnant women, their eating behaviors did not improve. To explain the ineffectiveness of the training, the researchers cited factors such as lifestyle, social beliefs, and economic issues. Since self-care is effective in improving the quality of life and reducing the medical costs for societies, its implementation can prevent diseases or delay their side effects (1, 18). Educational interventions like the present study should be designed and implemented to increase individuals' participation in self-care. In the present study, the mean scores of susceptibility and perceived severity constructs in the post-educational intervention group were significantly higher than in the control group. This result indicates that training strengthens the belief in individuals that if self-care behavior is not adopted, they are exposed to diseases and their complications. Today, awareness alone is not enough to perform health behaviors; individuals' beliefs about a phenomenon or disease are crucial factors in adopting or not adopting health-oriented behaviors such as self-care. Therefore, increasing the perceived threat through educational intervention is an important result of the present study. Consistent with our findings, previous studies (17, 19) have also proven an increase in the mean score of the perceived threat construct after training. However, contrary to our findings, Heydari et al. (33) and Pirzadeh and Sharifirad (34) did not find any significant increase in the mean score of perceived susceptibility after educational intervention. The discrepancy may be due to the short duration of the training program (two one-hour sessions) in the above studies.
In the present study, the mean score of perceived benefits in the intervention group did not increase significantly after training. Given the mean score of the perceived benefits construct at the beginning of the study, it can be argued that the participants, who were health workers, had a high perception of benefits of adopting self-care behaviors. The lack of effect of training on increasing the mean score of perceived benefits construct was also observed in studies by Gursoy et al. (35), Torshizi et al. (31), and Asadzandi et al. (36). However, the results of several studies indicated the effect of training on increasing the mean score of the perceived benefits construct (2, 17, 37). In the present study, a significant decrease in mean scores of perceived barriers after the educational intervention between the two groups indicated the positive effect of training on the reduction of perceived barriers in the intervention group. This result was consistent with studies by So et al. in Hong Kong (38), Lee et al. in Taiwan (29), and Cyr A et al. in the United States (39). Contrary to our findings, Abood et al. (40) indicated that the mean score of perceived barriers did not significantly decrease after the intervention. Abood suggested that the inconsistency might be due to lower pursuit and social and cultural determinants outside individual control, which can impact the effectiveness of educational interventions in reducing perceived barriers. Since the perceived benefits and barriers in the HBM pave the way for adopting behavior, special attention should be paid to training programs to encourage participation in self-care programs and influence their beliefs. The results of the present study indicated an increase in the mean score of self-efficacy in the intervention group compared to the control group. This finding was consistent with studies by Zamani-Alavijeh et al. (14) and Jadgal et al. (41). Previous studies have also emphasized the importance of increasing individual confidence and self-efficacy as key factors and important preconditions for self-care and the promotion of health behaviors (1, 18). Cegala and Lenzmeier Broz believes that training and applying effective strategies to create self-efficacy in employees can lead to self-satisfaction and customer satisfaction (42). Therefore, it seems that using self-efficacy improvement strategies can be useful in fostering health-promoting behaviors such as self-care.
Data collection through self-report was a limitation of the present study. To address this limitation, it is essential to reassure employees about the confidentiality of their information.
Educational interventions alone (i.e., not supplemented by behavior change techniques) are weakly effective in changing behaviors; the level of exposure to the intervention (i.e., the number of sessions attended) could have contributed to the limited improvement in the outcomes; the delivery of the intervention (issues of fidelity and competence) may not have been optimal, resulting in minimal improvement in the outcomes.
5.1. Conclusions
Educational interventions alone (i.e., not supplemented by behavior change techniques) are weakly effective in changing behaviors. The level of exposure to the intervention (i.e., the number of sessions attended) could have contributed to the limited improvement in the outcomes. Additionally, the delivery of the intervention (issues of fidelity and competence) may not have been optimal, resulting in minimal improvement in the outcomes. However, it seems that educational interventions and programs designed based on the HBM (HBM) do improve self-care behaviors in health workers. Therefore, it is suggested to implement similar training programs based on behavioral models in health centers to promote health among health workers. The results of the present study can help healthcare policymakers design and implement appropriate intervention programs to promote mental and physical health and strengthen self-care among staff.