1. Background
In today’s rapidly changing and unpredictable world, organizations often encounter unexpected events such as natural disasters, epidemics, and terrorist attacks (1). For example, the COVID-19 pandemic has caused substantial financial losses for many organizations (2). Resilience is defined as “the inherent ability of a healthcare system, such as a clinic, department, hospital, or country, to adjust its functioning before, during, or after events (e.g., changes, disruptions, and opportunities)” (3) . The literature on workforce resilience emphasizes that efforts should not only focus on absorbing unexpected shocks from emerging health needs, but also on ensuring continuity in health improvement, maintaining gains in system functioning, and reinforcing a people-centered approach while delivering high-quality care (4).
The concept of sustainable human resource management began in the late 1990s in Germany, Switzerland, and Australia (5). Many examples show that the term resilience readily applies across multiple sectors. It soon evolved into a benchmark for an increasing number of actors and areas. Research on resilience has been documented extensively, particularly in the fields of engineering, ecology, and developmental psychology (6).
This emerging approach in management emphasizes the design of organizational processes and human resources to embrace resilience principles, thereby enhancing working conditions and employee welfare (7). The connection between resilience and workforce management promotes both organizational stability and the resilience of workforce management practices (3).
Increased workload, stress, and lack of accountability among healthcare workers contribute to inefficiencies in medical services, leading researchers to focus on sustainable human resources as a solution (8). Over the past three decades, human resources have gained prominence due to the strategic role they play in improving organizational performance through cost-benefit analyses and the economic interests of shareholders and owners (9). In the health sector, human resource sustainability costs account for 65 to 80% of the overall health system budget, underscoring the critical role of human resource management from both clinical and financial standpoints (10). However, resilience in health systems remains a broad concept, encompassing multiple disciplines (health, social sciences, economics, etc.), levels (micro/individual, meso/organizational, macro/political, and national), and populations (individuals, communities, decision-makers, professionals, scientists, etc.) (6).
The aim is to make resilience a measurable operational indicator: "Resilience-related research is shifting from purely conceptual frameworks to a pursuit of practical methods for building resilience” (11). Currently, resilience indicators are primarily derived from individual psychological approaches, but there is an urgent need "to address gaps and strengthen global capacity to rapidly detect and respond to health crises" (6). In 2017, Kruk et al. proposed an initial resilience index, calling for its testing to refine the proposed indicators (12). Panels of experts have also emphasized the importance of bolstering health system resilience to effectively manage health crises. Despite growing research on resilience, inconsistencies remain in its conceptual definitions. Furthermore, resilience in human resources often exists only as a theoretical term, a political tool, or a "mode," which may detract from its true meaning in terms of sustainability (3).
2. Objectives
This study seeks to answer the question: What is the model of health system resilience in the context of human resources within the Ministry of Health and Medical Education (MOHME)?
3. Methods
3.1. Study Design
This study, conducted in 2023, utilized a mixed-method approach, integrating both quantitative and qualitative methodologies. The study was divided into two main parts: Qualitative and quantitative.
In the qualitative phase, a conceptual review of relevant articles was conducted to extract key dimensions and indicators. To finalize the dimensions and indicators for the model, the fuzzy Delphi technique was applied over two rounds.
The quantitative phase evaluated the effectiveness of the main components proposed in the model using the fuzzy DEMATEL method and the interpretive structural modeling (ISM) technique for the secondary components.
The DEMATEL method is a well-regarded, comprehensive approach to developing a structural model that illustrates interrelationships among complex real-world factors. It surpasses techniques like the analytic hierarchy process (AHP) because it captures interdependencies between a system’s factors through a causal diagram, which traditional methods often overlook. The ISM method, in turn, is used to identify and structure relationships among a set of factors, indicators, or variables. Unlike DEMATEL, ISM’s exploratory approach also addresses the hierarchical leveling of indicators, which adds an additional dimension to understanding relationships. This method helps researchers design an initial model after identifying underlying factors in the studied phenomenon through qualitative methods.
Given the nature of this research, content validity was used to assess the validity of the questionnaire. Reliability measures were not applicable, as the paired comparison questionnaires used in the DEMATEL method are standardized and pre-approved.
The respondents for the structural-interpretive modeling phase were experts with years of experience and advanced education, including heads, managers, and senior staff at medical science hospitals. Due to their expertise, conventional reliability measures like Cronbach’s alpha or composite reliability were deemed unnecessary for this type of questionnaire.
The methodology of this study involved four main steps: (1) identifying primary dimensions and indicators through a comprehensive review; (2) finalizing indicators and dimensions using the fuzzy Delphi technique; (3) applying the fuzzy DEMATEL method to assess the strength of relationships between dimensions; and (4) utilizing the structural interpretive modeling method to determine the intensity of relationships between indicators.
3.2. Identification of Dimensions and Indicators of Workforce Resilience
To identify the factors influencing workforce resilience, an expert review was first conducted in the fields of health and medical services. Following this, a primary research question was formulated to focus on workforce resilience factors.
3.2.1. Research Question
The scoping review addressed the following research question: “What is known from the literature about the concept of workforce resilience and its influencing factors?”
3.2.2. Literature Identification
A conceptual review was conducted across Scopus, Science Direct, and PubMed for publications from 2017 to 2023. Additional studies were sourced from Google Scholar. The search terms used included “workforce resilience,” “coping strategies,” “system responsiveness,” and “system adaptation” (Appendix 1 in the Supplementary File). To define the concept and factors affecting workforce resilience in health systems, Daigneault & Jacob's (13) conceptual analysis framework was used, which identifies three essential dimensions of a concept: Term, sense, and referent.
3.2.3. Quality Assessment of Included Studies
To ensure the quality of included studies, only articles from reputable journals were considered. After screening, duplicate and irrelevant articles were removed, leaving only relevant, high-quality studies for inclusion.
3.2.4. Inclusion and Exclusion Criteria
Studies were included if they met the following criteria: (a) the term "resilience" was used in the title, abstract, or keywords; and (b) health systems were the main focus of the study. Studies were excluded if they (a) centered on specific thematic areas (e.g., climate change, training processes) or specific groups (e.g., doctors, nurses, service managers) or (b) were unavailable in full-text versions.
Experts eligible for study participation were required to have theoretical expertise, practical experience, a willingness to participate, and accessibility. Based on these criteria, 20 experts completed the study process. Participants were excluded if they expressed unwillingness to participate, lacked time to complete the questionnaire, or left it incomplete.
3.2.5. Data Collection Procedures
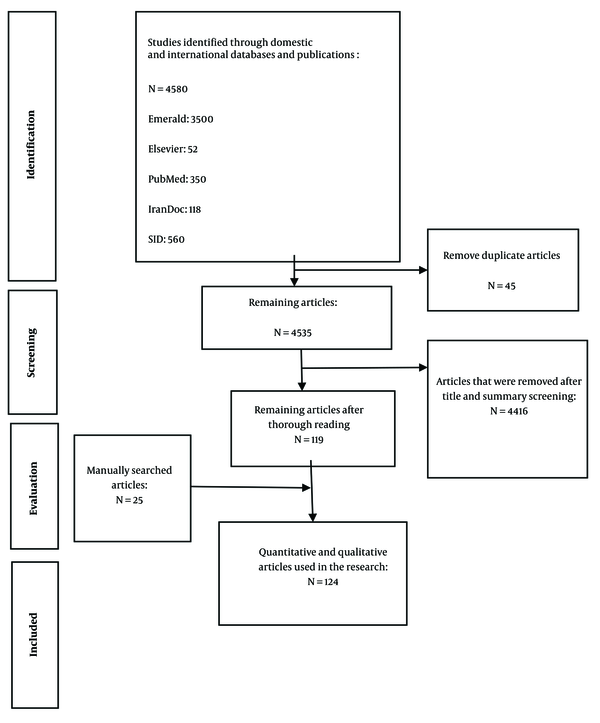
A purposeful sampling method was used to select the expert panel for this study. During the scoping review, studies obtained from databases were initially screened for eligibility by two reviewers, with duplicates removed using EndNote software. The remaining studies were then independently screened based on titles and abstracts. Articles that met the inclusion criteria were reviewed in full by the same reviewers. An additional reviewer was consulted to resolve any discrepancies at each stage of the screening process.
3.2.6. Data Extraction
Data extraction forms were created in Excel to capture both macro-data (descriptive characteristics of included studies) and micro-data (definitions, resilience dimensions, implementation methods, and authors’ recommendations) from the selected literature.
3.3. Fuzzy Delphi Technique for Screening
The fuzzy Delphi method was applied to identify and evaluate the importance of components and indicators (14).
3.4. Analytical Procedure of Fuzzy DEMATEL
Step 1: Define the decision goal and establish a committee
A decision goal was set, and a committee was formed to gather group knowledge for addressing the problem.
Step 2: Establish evaluation criteria and design
In this step, a set of criteria for evaluation was established. Since these criteria involve causal relationships and multiple complex aspects, the comparison scale of the crisp DEMATEL method was discarded to reduce ambiguities in human assessment.
Step 3: Assessment of decision-makers
Step 4: Normalized direct-relation fuzzy matrix (Table 1)
| Variables | Behavior | Empowerment | Motivational |
|---|---|---|---|
| Behavior | 1.848531 | 2.289289 | 2.087913 |
| Empowerment | 1.9162282 | 1.775851 | 1.885004 |
| Motivational | 2.203338 | 2.328252 | 1.849347 |
De-fuzzification of Dimensions
Step 5: Establish and analyze the structural model
3.5. Interpretive structural modeling
Step 1: Form the structural self-interaction matrix (SSIM)
Experts compared candidates in pairs and completed pairwise comparisons.
Step 2: Obtain the initial reachability matrix
The symbols of the SSIM matrix were converted to 0 and 1, producing the initial reachability matrix.
Step 3: Adjust the reachability matrix
For example, if the behavioral dimension is related to the motivational dimension and the motivational criterion is related to the empowerment criterion, then the behavioral criterion must also relate to empowerment.
Step 4: Determine the levels of variables
In this step, the input (prerequisite) and output (achievement) sets for each criterion were evaluated. Common factors were then identified. Once variables were specified, the center and centroid were removed from the table, and the process was repeated for the remaining criteria.
4. Results
4.1. Descriptive Statistics of Respondents
This section presents the demographic characteristics of respondents to the paired comparison questionnaire, including gender, age, and work experience (Tables 2 and 3).
| Questionnaire Type | N | Objective | Audience Type | Sampling Method |
|---|---|---|---|---|
| Fuzzy Delphi | 20 | Approval and finalization of indicators | Experts (heads, managers, metros of medical science hospitals) | Purposeful judgment |
| Fuzzy dimetal | 20 | Determining the intensity of the relationships between the main dimensions and indicators in explaining the model of human resource resilience and completing the fuzzy Dimetal tables | Experts (heads, managers, metros of medical science hospitals) | Purposeful judgment |
Sampling Characteristics
| Variables and Category | No. (%) |
|---|---|
| Age, y | |
| 30 - 40 | 5 (25) |
| 40 - 50 | 10 (50) |
| < 50 | 5 (25) |
| Work experience, y | |
| 5 - 10 | 2 (10) |
| 10 -15 | 8 (40) |
| < 15 | 10 (50) |
Frequency Distribution by Age and Work Experience
4.2. Scoping Review Results
The search strategy yielded a total of 4 605 articles (4 580 from scientific databases and 25 from manual searches). After removing 45 duplicate records, 4 416 articles were selected for title and abstract screening. A full-text review was conducted on 144 articles, of which 124 were excluded. Ultimately, 20 articles met the inclusion criteria and were included in the study (Figure 1 and Table 4).
| Row | Author | Year | Indicator |
|---|---|---|---|
| 1 | Macini et al. (15) | 2022 | Transparency-justice and equality-employee welfare-profitability |
| 2 | Chams and García-Blandón (16) | 2019 | Supportive culture - flexible work style - transparency - voluntary behavior - acquired skills - altruism - empathy - social reward - accountability - social participation sustainable management of allocation resources |
| 3 | Macke and Genari (5) | 2018 | Recruiting and retraining talents - developing employees' skills - maintaining a healthy and productive workforce - recruiting professionals - training and development - compensation - diversity management - organizational supervision and support - career management - occupational health and safety management - promotion of voluntary work - internal communication |
| 4 | Haldane et al. (4) | 2022 | Financing - health manpower - provision of health services - community participation |
| 5 | Anlesiny et al. (17) | 2019 | Values and attitudes - competencies of managers - availability of resources - perceived benefits - values and social cultures - stakeholder requests |
| 6 | Macchi Silva and Ribeiro (8) | 2021 | Accountability - individual competencies - risk management - preparedness for response - human resource management - risk management |
| 7 | Mossadegh Rad et al. (18) | 2020 | Governance and leadership - financing - manpower - requirements and equipment - information - adaptation - learning - response - change - planning - recruiting - forecasting and communication |
| 8 | Pedayi et al. (19) | 2021 | Joining support networks (insurance) - sustainable investment - self-esteem - emotion management - flexibility - optimism, hope - realism - empathy - maintaining religious beliefs - nutrition - personal health - exercise - lifestyle change - controlled communication |
| 9 | Etamadi et al. (20) | 2020 | Awareness - diversity - self - regulation - integration - adaptation |
| 10 | Martini et al. (7) | 2023 | Improvement of working conditions and welfare of employees |
| 11 | Cusack et al. (21) | 2016 | Mindfulness - self-efficacy - coping-neuroticism |
| 12 | Lim et al. (22) | 2020 | Psychological – organizational – social - economic resilience |
| 13 | Yu et al. (23) | 2020 | Job demands (stress, job burnout, post-traumatic stress disorder and workplace bullying) and job resources (coping skills, self-efficacy, social support, job satisfaction, job retention and general well-being) |
| 14 | Huey and Palaganas (24) | 2020 | work-life balance - having social support - metacognitive processes of coping and reframing - having a higher purpose - ability to take care of oneself - workplace culture - self-determined with positive thinking |
| 15 | Sood et al. (25) | 2020 | Personal competence - trust your instincts - reinforcement with stress - positive acceptance of change - control - spiritual effects |
| 16 | Bartone et al. (26) | 1989 | Commitment - control - change |
| 17 | Robertson et al. (27) | 2015 | Interactions between people, their learning, their organizations, and ultimately their developmental outcomes |
| 18 | Friborg et al. (28) | 2003 | Personal competence - social competence - family cohesion - social support - personal structure |
| 19 | Winwood et al. (29) | 2013 | Rest, physical health, flexibility in work |
| 20 | Mallak (30) | 2017 | Active problem solving - team efficiency - creating a sense of confidence - creating an immediate solution |
Dimensions and Indicators of Human Resource Resilience
4.3. Fuzzy Delphi Results
Using the fuzzy Delphi method, 34 factors were identified: Work experience, strengthening the culture of creativity, accepting suggestions, flexibility, justice, equality, transparency, work commitment, accountability, efficiency, job design, attracting professionals, risk management, promoting voluntary work, proactivity, adaptability, information sharing, autonomy, on-the-job training, strengthening religious beliefs, sports activities, personal hygiene, lifestyle changes, self-esteem, empathy, self-control, happiness creation, interaction with the surrounding environment, continuous performance evaluation, employee welfare, rewards, career advancement, compensation for damages, timely handling of complaints, and job security (Table 5).
| Row | Indicator | Fuzzy Average of the Second Stage | The Definitive Average of the First Stage | The Definitive Average of the Second Stage | Difference | ||
|---|---|---|---|---|---|---|---|
| 1 | Experience | 0.768 | 1.125 | 1.411 | 1.101 | 1.101 | 0 |
| 2 | Strengthening the culture of creativity | 0.411 | 0.750 | 1.089 | 0.750 | 0.750 | 0 |
| 3 | Accepting offers | 0.482 | 0.839 | 1.143 | 0.821 | 0.821 | 0 |
| 4 | Flexibility | 0.875 | 1.232 | 1.375 | 1.161 | 1.161 | 0 |
| 5 | Justice and equality | 0.911 | 1.268 | 1.393 | 1.190 | 1.190 | 0 |
| 6 | Transparency | 0.393 | 0.732 | 1.071 | 0.732 | 0.732 | 0 |
| 7 | Commitment | 0.964 | 1.321 | 1.393 | 1.226 | 1.226 | 0 |
| 8 | Responsiveness | 0.571 | 0.929 | 1.214 | 0.905 | 0.905 | 0 |
| 9 | Speed | 0.500 | 0.821 | 1.143 | 0.821 | 0.821 | 0 |
| 10 | Career design | 0.446 | 0.768 | 1.071 | 0.762 | 0.762 | 0 |
| 11 | Recruitment of professionals | 0.768 | 1.143 | 1.375 | 1.101 | 1.101 | 0 |
| 12 | Sympathy | 0.518 | 0.875 | 1.179 | 0.857 | 0.857 | 0 |
| 13 | Risk management | 0.929 | 1.268 | 1.411 | 1.208 | 1.208 | 0 |
| 14 | Promotion of voluntary work | 0.375 | 0.732 | 1.054 | 0.720 | 0.720 | 0 |
| 15 | Being an activist | 0.429 | 0.768 | 1.071 | 0.756 | 0.756 | 0 |
| 16 | Adaptation | 0.875 | 1.232 | 1.339 | 1.149 | 1.149 | 0 |
| 17 | Information sharing | 0.714 | 1.071 | 1.339 | 1.042 | 1.042 | 0 |
| 18 | Have freedom of action | 0.696 | 1.054 | 1.339 | 1.030 | 1.030 | 0 |
| 19 | On-the-job training | 0.786 | 1.125 | 1.339 | 1.083 | 1.083 | 0 |
| 20 | Strengthening religious beliefs | 0.518 | 0.857 | 1.179 | 0.851 | 0.851 | 0 |
| 21 | Sport activities | 0.339 | 0.696 | 1.054 | 0.696 | 0.696 | 0 |
| 22 | Personal hygiene | 0.821 | 1.179 | 1.429 | 1.143 | 1.143 | 0 |
| 23 | Changing life style | 0.661 | 1.018 | 1.339 | 1.006 | 1.006 | 0 |
| 24 | Self-esteem | 0.768 | 1.125 | 1.411 | 1.101 | 1.101 | 0 |
| 25 | Strengthening self-control | 0.500 | 0857 | 1.214 | 0857 | 0.857 | 0 |
| 26 | Creating happiness | 0.607 | 0.964 | 1.321 | 0.964 | 0.964 | 0 |
| 27 | Interaction with the surrounding environment | 0.589 | 0.946 | 1.268 | 0.935 | 0.935 | 0 |
| 28 | Continuous performance evaluation | 0.732 | 1.089 | 1.339 | 1.054 | 1.054 | 0 |
| 29 | Staff welfare | 0.643 | 1 | 1.304 | 0.982 | 0.982 | 0 |
| 30 | Reward | 0.911 | 1.268 | 1.429 | 1.202 | 1.202 | 0 |
| 31 | Promotion | 0.571 | 0.929 | 1.250 | 0.917 | 0.917 | 0 |
| 32 | Compensation for damages | 0.607 | 0.964 | 1.304 | 0.958 | 0.958 | 0 |
| 33 | Timely handling of complaints | 0.607 | 0.946 | 1.250 | 0.935 | 0.935 | 0 |
| 34 | Job security | 0.679 | 1.036 | 1.375 | 1.030 | 1.030 | 0 |
Results of the Second Round of Fuzzy Delphi
4.4. Integration Matrix Results
After normalizing expert opinions regarding health system resilience dimensions in human resources, the integration matrix was calculated for each limit (U, M, and L). By combining three fuzzy matrices, the final relationships of matrix T were obtained (Table 6).
| Variables | Behavioral | Empowerment | Motivational | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Behavioral | 0.54 | 1.25 | 4.33 | 0.87 | 1.67 | 4.93 | 0.77 | 1.52 | 4.52 |
| Empowerment | 0.68 | 1.36 | 4.25 | 0.51 | 1.19 | 4.20 | 0.68 | 1.35 | 4.14 |
| Motivational | 0.83 | 1.58 | 4.80 | 0.88 | 1.68 | 5.06 | 0.54 | 1.25 | 4.33 |
Integration Matrix T
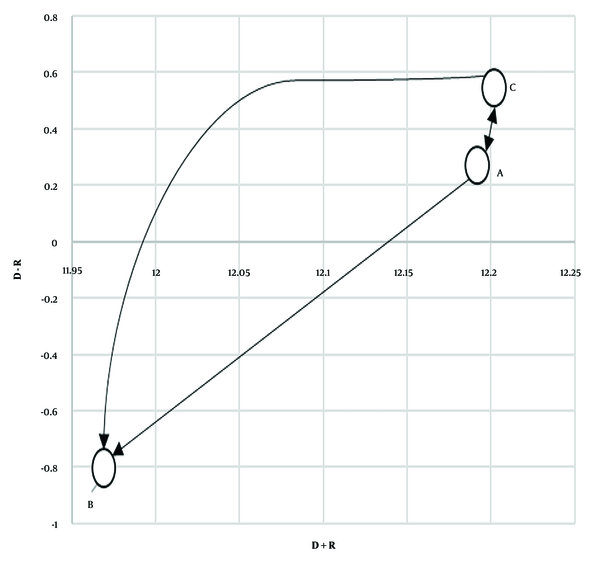
4.5. De-fuzzification of Model Dimensions Results
In this section, the D (sum of rows) and R (sum of columns) were calculated and de-fuzzified using the Central Region method. The values for D + R and D - R are shown in Table 7.
| D | R | D + R | D - R |
|---|---|---|---|
| 6.22 | 5.96 | 12.19 | 0.25 |
| 5.57 | 6.39 | 11.97 | -0.81 |
| 6.38 | 5.82 | 12.20 | 0.55 |
De-fuzzified D and R Calculations
Based on expert opinions on the relationships among the dimensions of health system resilience in human resources and the data in Table 6, a cause-and-effect relationship between dimensions was mapped in Figure 2. Additionally, Table 1 shows the de-fuzzification of the T matrix, illustrating the effectiveness and influence of each dimension.
The first step in performing calculations for the fuzzy DEMATEL technique involves identifying an appropriate linguistic spectrum for data collection. Various spectrums have been suggested based on the conventional DEMATEL scoring scale. Among these, two fuzzy spectrums are particularly popular, both of which are listed in Table 8.
| Linguistic Term | Numerical Value |
|---|---|
| Very high impact (VH) | (0.75, 1, 1) |
| High impact (H) | (0.5, 0.75, 1) |
| Low impact (L) | (0.25, 0.5, 0.75) |
| Very low impact (VL) | (0 ,0.25, 0.5) |
| No effect (NO) | (0, 0, 0.25) |
Linguistic Expressions and Fuzzy Numbers
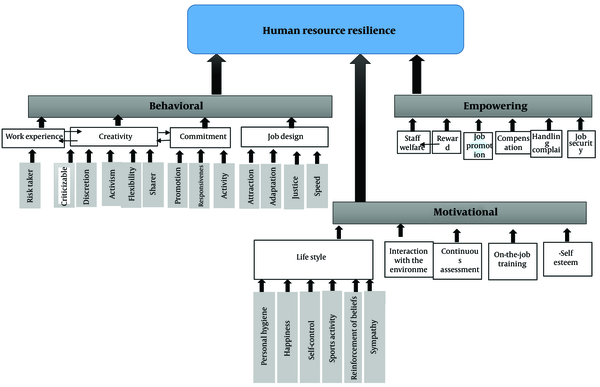
4.6. The Final Model for Improving Human Resource Resilience in the Health System
After analyzing the data obtained from the qualitative portion of the research, the final model was developed. It includes three main dimensions—behavioral, motivational, and empowering—along with 16 indicators and 18 sub-indicators. Following two rounds of expert review and necessary revisions, the model was formulated. Using the fuzzy modeling technique, a Level 1 model (including the behavioral, motivational, and empowering dimensions) was established. The ISM technique was then applied to define the relationships between the indicators and dimensions (Figure 3).
5. Discussion
The findings of this study align with those of prior research, including studies by Mancini et al. (15), Chams and García-Blandón (16), Macke and Genari (5), Anlesinya et al. (31), Macchi Silva and Ribeiro (8), and Haldane et al. (4) These studies each examined aspects of human resource resilience within health systems.
For instance, Mancini et al. (15) identified factors such as justice, equality, transparency, and employee welfare as indicators of human resource resilience, which were similarly included in our model. However, to enhance the effectiveness of these concepts, they were incorporated as indicators within the behavioral dimension in this study, ensuring they could be applied to the strategic and operational plans of health systems.
In the model by Chams and García-Blandón (16), human resource resilience factors such as flexibility, transparency, voluntary behavior, and rewards were highlighted. Although both models share similarities, this study applied factor-leveling techniques (indexing) and classification (dimension separation and indicators) to introduce a two-level, multi-dimensional model, making the model more operational.
Additionally, in the model by Macke and Genari (5), factors such as the recruitment of professionals, training and development, and compensation for damages were proposed as influences on human resource resilience. These factors were also considered in the current model to provide a comprehensive view of resilience factors impacting health system human resources.
Anlesinya et al. (31) introduced human resource resilience as a mediator for organizational legitimacy and performance. They emphasized developing competencies and values associated with human resource resilience as essential for creating resilient workforces, a notion that our study supports. However, the model by Anlesinya et al. (31) does not directly address specific dimensions and indicators of human resource resilience, which diverges from our findings. In contrast, Macchi Silva and Ribeiro (8) examined macro competencies for organizational resilience, proposing four main dimensions: Human resource management, development of individual competencies, risk management, and accountability. These factors were also investigated in our study, but they were categorized within the three main dimensions of our model: Behavior, motivation, and empowerment.
Haldane et al. (4) analyzed key resilience factors within the health system framework, identifying governance and financing, health service delivery, workforce, products, medical technology, and public health as core dimensions. While Haldane et al. (4) viewed human resource resilience as a subset of overall health system resilience, our study considered it as a broader field with multiple dimensions and indicators.
Luthans (32) defined resilience as a "developable capacity to recover or bounce back from adversity, conflicts, and failures," associating resilience with positive personal attitudes and behaviors such as acceptance, adaptability, and flexibility. In the current study, these aspects are explored within the behavioral dimension, particularly through indicators of job design and creativity. We also examined other related indicators—such as speed, justice and equality, freedom of action, and openness to suggestions—to create a comprehensive model of resilience.
Nishii and Paluch (33) highlighted the role of the behavioral dimension in shaping and implementing human resource systems within organizations. They suggested that the behavioral dimension of human resources significantly influences employees' perceptions of human resource management practices. This aligns with our focus on the behavioral dimension's impact within our resilience model.
The results of the current study confirmed the behavioral dimension as a key aspect of human resource resilience. This research comprehensively investigated the behavioral dimension of human resources, examining relevant indicators and components such as job design and creativity. According to Guest et al. (34), effective human resource practices lead to positive outcomes for employees. One notable outcome is employee engagement, which has been reported to yield various benefits, including increased voluntary work, life satisfaction, work participation, happiness, general well-being, and transparency. Wikhamn (35) emphasized the importance of attracting and retaining resilient human resources by providing a healthy work environment. Our study examined this issue in detail within the motivational dimension, particularly through the lifestyle change index, which includes components such as personal health and sports activities. In contrast, Wikhamn's study (35) did not reference the specific components of a healthy work environment, treating it solely as an independent variable.
5.1. Limitations
This study has several limitations. First, a questionnaire was used for data collection, which may have led some participants to provide unrealistic responses instead of accurate ones. Second, since this study was conducted cross-sectionally, generalizing the results should be approached with caution.
5.2. Conclusions
Based on the results, three dimensions were identified: The behavioral dimension, the motivational dimension, and the empowerment dimension. By accurately measuring these dimensions and their indicators, it becomes possible to assess the resilience of human resources in the health sector across various health and treatment areas in the country. Additionally, this study identified key indicators of the behavioral dimension, such as work experience, commitment, creativity, and job design. For the motivational dimension, key indicators included lifestyle, empathy, interaction with the environment, continuous evaluation, on-the-job training, and self-esteem. Finally, the empowerment dimension was characterized by key indicators like well-being, rewards, compensation, timely resolution of complaints, and job security.
The dimensions identified in the model can be considered overall goals for formulating the strategic and operational plans of health and treatment sectors, enabling the operationalization of goals related to the resilience of human resources in the health field. Additionally, the indicators and sub-indices identified in this model can serve as measures, activities, and checklists for assessing and evaluating initiatives related to human resource resilience (strategic and operational plans) to ensure the efficiency and effectiveness of these measures.