1. Background
In despite of the promotion of public health and improvement of life style in the recent years, parasitic diseases have remained a public health problem in many parts of the world. Water is a major source for acquiring several pathogenic agents including bacteria, viruses and parasites. These biological agents can be transmitted via non-sanitized water (1, 2). According to World Health Organization reports more than 80 infectious diseases can be transmitted by water (3). Population growth, urbanization, existence of infected animals, climate variations, deficit and elderly of water network system, and hygienic poverty are main factors for the spread of pathogenic parasite agents (1). The World Health Organization has estimated that 40% of the world’s population lives in areas with lack of sanitation (2.4 billion people); 1.1 billion person do not have access to safe water and up to 2.2 million children die annually due to diarrhea (1). Moreover, in developing countries, 60% of the population do not have access to healthy drinking water (3, 4). During 1920 to 2002 in the United States, at least 1870 water born disease outbreaks were reported with an average of 22.5 reports per year (5). In addition during 1991 to 2002, approximately 207 outbreaks were reported due Giardia and Cryptosporidium infection via water in the United States (5). The study on quality and sanitation of water is not only very crucial for public health but also for immunodeficiency individuals in the community (6). There are a few studies on water contamination in Iran, amongst which a study by Ziae reported on water parasite contamination in the Mazandaran province with gastrointestinal protozoan parasites (22). Naeini et al. showed that rivers of Chaharmahal-Bakhtiary province of Iran are contaminated with a variety of parasites (23).
2. Objectives
Unfortunately, water quality problems and massive fecal contamination remain unsolved. Therefore studies of water quality and sanitation should be continually performed in most countries especially in tropical areas with defected water network structures. From July to August 2013, an outbreak of gastrointestinal parasitic disease was reported by a health organization located in the west of Ahvaz city, which indicated an increase in prevalence of gastrointestinal diseases in related areas. Therefore this study was conducted to evaluate the mentioned problems.
3. Materials and Methods
3.1. Sampling
Forty-four water samples (four litters for each sample) were collected from Golestan, western part Ahvaz city, southwest of Iran. The samples were from three different sources including water refiners (home filter), tap water, before and after treated water and water selling stations during July to August 2013. The water samples were transported to the parasitology department of the medical faculty and were left to stay undisturbed for 24 hours at room temperature (7). The supernatant was sucked and removed (6-8). Sediments of each sample were examined microscopically, as a 0.9% saline smear, for parasite cysts, trophozoites and helminth eggs (3, 9). Samples were stained with Lugol’s iodine, modified Ziehl-Neelsen acid-fast stain (hot method) and the trichrome technique (9). Descriptive statistical method was used for data analysis.
4. Results
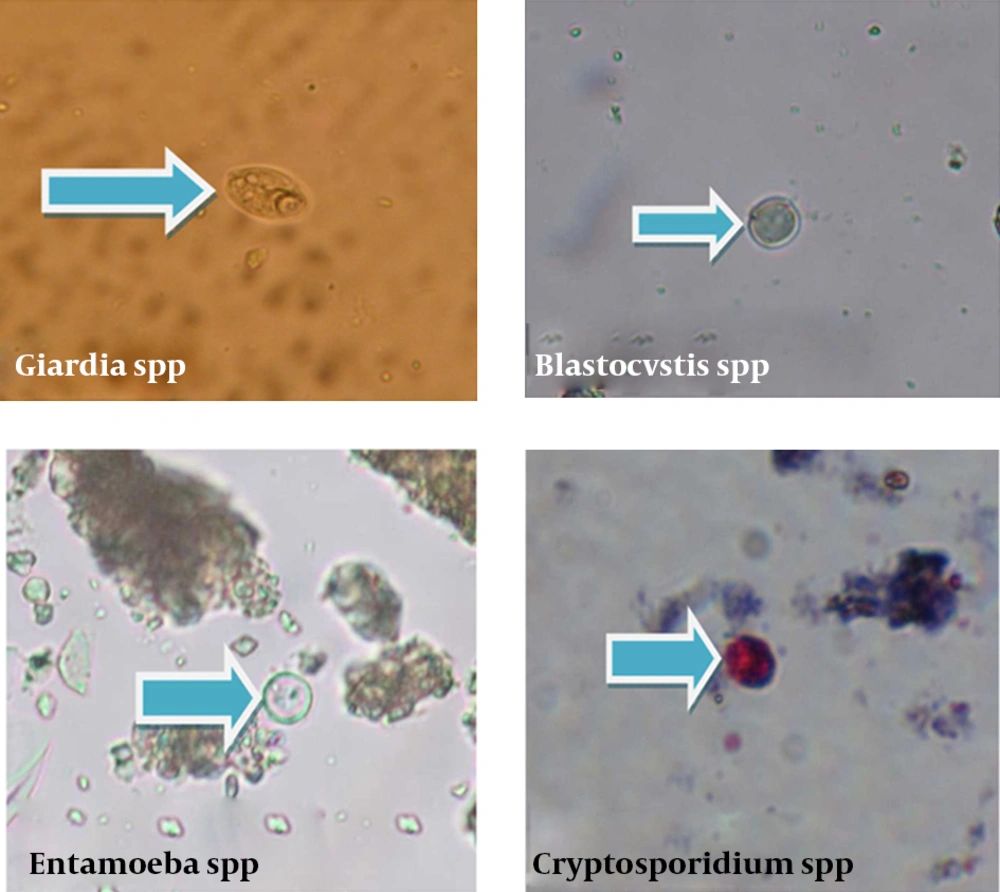
Twenty-eight out of 44 water samples were positive for parasitic contamination with cyst and oocysts of four parasitic protozoans including: 50% Entamoeba spp (22 out of 44 samples), 27.27% Cryptosporidium spp (12 out of 44 samples), 13.63% Blastocystis spp (6 out of 44 samples) and 9.09% Giardia spp (4 out of 44 samples). Table 1 and Figure 1 show the collected parasites from each water sample. There were differences amongst positive samples according to clearance, from low to high turbidity. Table 2 presents the rate of parasitic contamination in the studied samples.
There was not helminthes contamination in the studied water samples. In 28 positive samples the most frequent parasitic contamination was related to Entamoeba spp Cysts, and the least frequent parasitic contamination was related to Giardia spp Cysts. The observed parasitic contaminations included the following infection agents; Entamoeba spp (eight samples), Cryptosporidium spp (three samples) and Blastocystis spp (one sample). There was no parasitic contamination in all three samples from the three water-selling stations. In 20 out of 31 tap water samples, cysts and oocysts of protozoan parasites were detected.
| No. | Kind of Sample | Result |
|---|---|---|
| 1 | raw water | Entamoeba spp |
| 2 | raw water | Entamoeba spp |
| Cryptosporidium spp | ||
| 3 | raw water | Entamoeba spp |
| 4 | treated water | Entamoeba spp |
| 5 | treated water | - |
| 6 | raw water | Entamoeba spp |
| Cryptosporidium spp | ||
| 7 | raw water | Entamoeba spp |
| 8 | treated water | - |
| 9 | raw water | Entamoeba spp |
| 10 | raw water | Entamoeba spp |
| Blastocystis spp | ||
| Cryptosporidium spp |
Parasites in Ten Samples of Water Refiners of Golestan District
| Parasite | Water refiner | Tap water | Water Selling station (3) | |||
|---|---|---|---|---|---|---|
| Raw water (River) (7) | Treated water (3) | Shahrak Daneshgah district (10) | Pardis district (11) | Mojahed district (5) | ||
| Entamoebaspp | 7 | 1 | 6 | 7 | 1 | 0 |
| Cryptosporidium spp | 3 | 0 | 4 | 4 | 1 | 0 |
| Blastocystisspp | 1 | 0 | 1 | 3 | 1 | 0 |
| Giardia spp | 0 | 0 | 3 | 0 | 1 | 0 |
| Number of samples without parasitic contamination | 0 | 2 | 6 | 3 | 2 | 3 |
Parasitic Infection Frequency of Water Samples Collected From Rivers, Treated Water, Tap Water and Water Selling Stations During July to August 2013
5. Discussion
There are many researches on evaluation of parasitic contamination of water sources in the world. Recently, Robertson in Norway (11, 12), Ono in Japan (13), Briancesco in Italy (14), Azman in Malaysia (15), Gracenea in Spain (10), Khouja in Tunisia (7), Ayaz in Pakistan (3), Bakir in Ankara (9), Hajdu in Sweden (17), Basualdo in Argentina (18), Farias in Brazil (19), Plutzer in Hungary (20), and Nichols in United Kingdom (21) have conducted studies for detection of parasitic contamination of water. In Iran, several studies have been performed in different provinces and cities, Mazandaran (Ziae) (22), Chahrmahal va bakhtyari (Naeini) (23), Ouroomieh (Nanbakhsh) (24) and Kashan (Rasti) (25). The current study indicates that Entamoeba spp cysts were predominant in all district water samples of Ahvaz which is consistent with the study of Ziae (22) from mazandaran and Ayaz (3) from Pakistan. These findings were positively correlated with clinical laboratory reports from Ahvaz, according to which Entamoeba histolytica were more predominant than other protozoan pathogens in gastrointestinal tract of patients. The second most frequent infection was that caused by Cryptosporidium spp that was detected in most positive samples. The results were in agreement with Ayaz and Robertson studies from Pakestan and Norway (3, 12) yet were not in agreement with the results of Ziae’s study from Mazandaran (22). Moreover we found Blastocystis spp in six samples from 44 (13.63%). There was no information about Blastocystis contamination in water samples from Iran. Low percentage of water samples were contaminated by Giardia cysts, which does not agree with other investigations from Iran and other parts of the world (22). In this study all samples from Karoon river were contaminated by protozoan parasites. Although no Giardia cysts were isolated from river samples yet in some tap water samples, Giardia cysts were detected. Briancesco from Italy, found a few Giardia cysts in raw water samples (14). This discordance may be due to low number of collected samples in this study. According to this research water entering into water refiners had a low sanitary quality. Three samples of treated water were infected by parasites, which indicated that treatment methods used for refining water was not adequate. Trophozoites are susceptible to most disinfectants but cysts and oocysts remain resistance to chlorination and ozone treatment. Thus the physical removal of Giardia, Entamoeba cysts and Cryptosporidium oocysts by multiple barriers is very important (8). In Ahvaz, most drinking water sources are obtained from surface water, which could be more easily contaminated with parasitic protozoa from animals and human. On the other hand, nearness of the water distributary system to the sewage system, water piped network older than 30 years of age, and using water pumps to raise pressure of water in many houses induced vacuum and drew sewage water from broken water pipe system. In addition, Karoon River is contaminated with industrial sewage materials and wastewater from hospitals. Contamination of drinking water with parasitic agents has not been shown by Briancesco from Italy (14), Bakir from Ankara (9) and researchers of other developed countries yet Ayaz reported drinking water infection in Pakistan (3). Parasitic agents were not seen in market supplied water because of appropriate filter techniques. Helminthes infection was not seen in all studied water samples and this finding agrees with Ziae’s study from Mazandaran (22), Khouja from Tunisia (7), Ayaz from Pakistan (3), and Bakir from Ankara (9). The report of helminthes infection by a local medical laboratory showed a significant decrease of this infection in Ahvaz during the recent years. The current findings are correlated with recent waterborne parasite outbreak reports, which show that the majority parasites were protozoans (97.7%) (6, 26). This study indicated that hygienic quality of water in the studied area is not satisfactory. A number of studies have demonstrated that both Giardia and Cryptosporidium are not only dispersed in tap water but also in bottled water (4). The Entamoeba cyst, a waterborne pathogenic parasite, has been identified to be responsible for serious outbreaks in this area. Giardia spp, Cryptosporidium spp, Entamoeba spp and Blastocystis spp in water samples, are a potential risk for infection in humans.
The current study showed that the rate of parasitic infections in drinking water is considerably high. The refractory system of water organization should be promoted by using effective disinfect techniques while the reconstruction of pipe water network should be considered. Until the achievement of these goals, personal protection should be done by using house filter systems. Furthermore, to find a seasonal pattern for water contamination, using molecular techniques for precise identification of parasites is recommended.