1. Background
Cancer is a disease characterized by uncontrolled cellular growth and the invasion of local and systemic tissues (1). With the advancement of medical science, a cancer diagnosis is no longer synonymous with imminent death; however, the diagnosis itself can cause profound emotional and psychological problems in patients (2, 3). Patients with cancer frequently experience a range of psychological distress beyond anxiety and depression (4). Common psychological complications include fear of death, fear of recurrence, body image issues, guilt, anger, and grief (5). These challenges can significantly impact a patient's quality of life and contribute to a severe psychological crisis. Among these, death anxiety is a particularly prevalent and distressing concern for many cancer patients (6).
Death anxiety is the source of many mental illnesses and is the inevitable result of confronting existential concepts such as death, freedom, choice, isolation, and meaninglessness (7). It arises when we accept the realities of our own mortality, confront suffering and pain, acknowledge our need to struggle for survival, and recognize our own fallibility (8). Patients with cancer frequently experience a heightened level of anxiety compared to healthy individuals. Grassi et al. (9) reported a high prevalence of anxiety and depressive disorders among patients with cancer. Nikoy Kouhpas et al. (10) found that chronic illnesses, such as cancer, are associated with increased stress, rendering patients more susceptible to its effects. Consequently, therapeutic efforts should be directed toward the reconstruction and treatment of anxiety. Some studies have indicated that even in types of cancer for which there are effective treatments, patients, due to misinformation, equate a cancer diagnosis with death, which is one of the critical concepts of existence (11).
Given the importance of death anxiety in patients with cancer, investigating the factors affecting it is of particular significance. One of these factors is mindfulness (12). Mindfulness is defined as the state of heightened attention and awareness of what is happening in the present moment, which allows individuals to respond to events with thought and reflection rather than reacting involuntarily and without contemplation (13, 14). Sheikhzadeh et al. (15) found an inverse relationship between mindfulness and anxiety and depression levels. In patients with cancer, lower mindfulness is also a significant predictor of emotional disturbances and psychological symptoms such as anxiety and depression (16, 17).
Conversely, an important factor that can affect mindfulness in patients with cancer and lead to a reduction in death anxiety is self-efficacy for coping with cancer (18). In this context, the active involvement of the patient in self-management, self-efficacy, and participation in medical counseling is particularly important (19, 20). Self-efficacy is associated with better self-care and management in people with chronic diseases (21). It is one of the key variables in Bandura's social cognitive theory (22). Bandura defined self-efficacy as individuals' beliefs in their abilities to mobilize motivations, cognitive resources, and exert control over a specific event (22). Individuals with high self-efficacy tend to have higher motivation and believe they can use the metacognitive skills necessary to apply these strategies, manage resources effectively to perform tasks, and monitor their progress. However, individuals with low self-efficacy, who do not believe in their abilities to succeed, exhibit low motivation and may delay starting and completing tasks (23, 24).
Overall, cancer is the leading cause of death in developed countries and the second leading cause of death in developing countries, after heart disease (25). Despite advances in the treatment of cancer patients, this disease remains a major cause of death, suffering, and pain. Even for those who recover quickly from the disease, significant psychological distress can persist (6). Overall, cancer continues to be a major cause of death, suffering, and pain worldwide, despite advancements in treatment. Even for those who recover, the psychological distress associated with cancer can have lasting effects.
2. Objectives
Given the significant impact of cancer on patients' well-being, this study aimed to explore the relationship between death anxiety, mindfulness, and cancer self-efficacy in a sample of patients with cancer in Tehran.
3. Methods
The present study was a descriptive correlational study that examined the relationship between variables in the framework of structural equations. The study population comprised all patients with cancer in Tehran who sought care at the Tehran Cancer Association between February and June 2023. A convenience sample of 302 patients with cancer was selected for this study. Participants were provided with an online link to access the study questionnaires and were requested to complete them.
Inclusion criteria included: Being diagnosed with cancer, willingness and ability to participate in the study, and the ability to understand and complete the research questionnaires (written and cognitive ability). Exclusion criteria included: Incomplete questionnaires due to missing data, random responses, or evidence of inattentive responding, and withdrawal of consent at any point during the study.
Regarding the sample size for testing the proposed model and research hypotheses, according to Loehlin and Beaujean (26), and considering the number of research paths and the number of variables, a sample size of 270 subjects is sufficient. However, considering the potential for attrition, a sample size of 315 subjects was selected. In the end, 302 subjects fully responded to the questionnaires and entered the study.
Ethical considerations for this study include obtaining informed consent from participants, ensuring voluntary participation, protecting participant confidentiality, and addressing the specific needs of the vulnerable cancer patient population.
3.1. Instruments
3.1.1. The Death Anxiety Scale
The Death Anxiety Scale is a 15-item self-report measure designed to assess various aspects of death anxiety. This multidimensional scale utilizes a yes-no response format to evaluate individuals' thoughts about death, preoccupation with death, fear of a shortened lifespan, and anxieties regarding the future. The scale includes items such as "I am very afraid of dying," "I am afraid of the thought of having an operation," and "I am often worried about time passing quickly." Scores on the scale range from 0 to 15, with higher scores indicating greater death anxiety (27). Sharif Nia et al. (28) reported good psychometric properties for the scale, with internal consistency (alpha) of 0.89 and test-retest reliability of 0.91. In the present study, Cronbach's alpha was used to determine the reliability of the scale, which was 0.86.
3.1.2. Five Facet Mindfulness Questionnaire
The Five Facet Mindfulness Questionnaire (FFMQ) was developed by Baer et al. (29) and consists of 15 items that assess mindfulness. Mindfulness is defined as the non-judgmental or accepting focus of attention on the present moment. Mindfulness can be contrasted with states such as rumination, worrying, or automatic behavior, in which attention is focused elsewhere. The FFMQ is scored on a 6-point Likert Scale, with 1 being "almost never" and 6 being "almost always." Sample items from this scale include "I am good at finding words to describe my feelings," "I understand my feelings and emotions without needing to react to them," and "I think some of my feelings are bad and inappropriate, and I should not feel them." The total score ranges from 15 to 90, with higher scores indicating greater mindfulness. The internal consistency of the FFMQ has been reported as 0.86 (30). In the present study, Cronbach's alpha was used to determine the reliability of the FFMQ, which was 0.85.
3.1.3. Cancer Behavior Inventory
The Cancer Behavior Inventory (CBI) was developed by Merluzzi et al. (31) to assess self-efficacy for coping with cancer. The 33-item CBI is used to measure self-efficacy for coping with cancer. This form of the questionnaire has four subscales: Independence, participation, stress management, and emotion management. The CBI is scored on a 9-point Likert Scale. Sample items from this scale include "I maintain my independence," "I accept the physical limitations and changes due to cancer treatment," and "I control my negative feelings about cancer." The total score of the CBI is calculated by summing the scores of all 33 items, with a minimum score of 33 and a maximum score of 297. A higher total score indicates greater self-efficacy. The internal consistency of the CBI has been reported as 0.75 (32). In the present study, Cronbach's alpha was used to determine the reliability of the CBI, which was 0.81.
3.2. Data Analysis
Pearson correlation coefficients were used to examine the relationships between the variables. The proposed model of the study was evaluated using structural equation modeling (SEM) with SPSS-27 and AMOS-25 software.
4. Results
The mean age of the patients with cancer was 46.04 ± 10.23 years. In terms of marital status, 88 (29.14%) patients were single, and 214 (70.86%) were married. Regarding gender, 153 (50.66%) patients were female, and 149 (49.34%) patients were male. In terms of education level, 23 (7.61%) patients had a middle school education, 64 (21.19%) patients had a high school education, 195 (64.57%) patients held a bachelor's degree, 17 (5.63%) patients had a master's degree, and 3 (1.00%) patients held a Ph.D. degree.
Table 1 presents the means, standard deviations (SD), and Pearson correlation coefficients of the study variables. The mean score for death anxiety was 8.35, with a standard deviation of 2.83. For mindfulness, the mean was 52.10, with a standard deviation of 6.84. Finally, the mean score for cancer self-efficacy was 156.13 ± 29.12.
The results of the Pearson correlation analysis revealed a significant negative correlation between mindfulness and death anxiety (r = - 0.31, P < 0.01), indicating that higher levels of mindfulness were associated with lower levels of death anxiety. Additionally, a significant negative correlation was found between cancer self-efficacy and death anxiety (r = - 0.55, P < 0.01), suggesting that individuals with higher cancer self-efficacy tended to experience lower levels of death anxiety. Finally, a significant positive correlation was observed between mindfulness and cancer self-efficacy (r = 0.39, P < 0.01), implying that higher levels of mindfulness were associated with greater cancer self-efficacy.
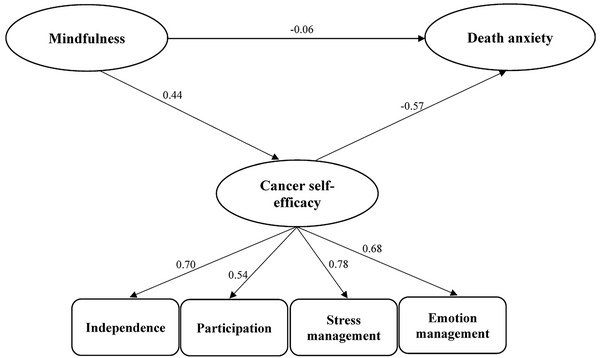
Figure 1 presents the initial proposed model for explaining death anxiety based on mindfulness and cancer self-efficacy.
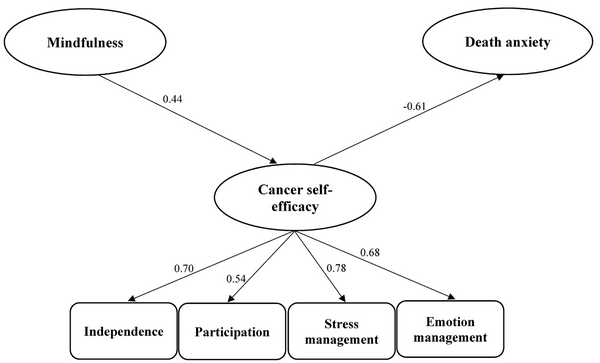
According to the data presented in Table 2, all fit indices, except for the RMSEA, were within the acceptable range. Therefore, the model required modification. To improve the model fit, the relationship between mindfulness and death anxiety was removed. This adjustment resulted in satisfactory fit indices. As shown in Table 2, all fit indices, including the chi-square value (χ2 = 61.54), the normed chi-square (χ2/df = 2.18), the Tucker-Lewis Index (TLI = 0.95), the Comparative Fit Index (CFI = 0.96), the Incremental Fit Index (IFI = 0.91), the Normed Fit Index (NFI = 0.94), and the root mean square error of approximation (RMSEA = 0.065), indicated an acceptable fit of the final model to the data. The final model is presented in Figure 2.
| Fit Indicators | Initial Model | Final Model |
|---|---|---|
| χ2 | 60.26 | 61.54 |
| df | 26 | 27 |
| (χ2/df) | 2.31 | 2.18 |
| TLI | 0.95 | 0.95 |
| CFI | 0.96 | 0.96 |
| IFI | 0.91 | 0.91 |
| NFI | 0.94 | 0.94 |
| RMSEA | 0.086 | 0.065 |
Fit Indicators in the Initial and Final Models
The results of the direct and indirect path coefficient estimates are presented in Table 3. The analysis revealed a significant negative correlation between mindfulness and cancer self-efficacy, as well as between cancer self-efficacy and death anxiety (P < 0.001). Interestingly, no significant direct association between mindfulness and death anxiety was observed. However, a significant indirect effect of mindfulness on death anxiety emerged when mediated by cancer self-efficacy (P < 0.001).
| Path | Initial Model | Final Model | |||
|---|---|---|---|---|---|
| Path Type | β | P | β | P | |
| Mindfulness to death anxiety | Direct | -0.06 | 0.258 | - | - |
| Mindfulness to cancer self-efficacy | Direct | 0.44 | 0.001 | 0.44 | 0.001 |
| Cancer self-efficacy to death anxiety | Direct | -0.57 | 0.001 | -0.61 | 0.001 |
| Mindfulness to death anxiety through cancer self-efficacy | Indirect | -0.104 | 0.001 | -0.112 | 0.001 |
Path Coefficients of Direct and Indirect Relationship Between Research Variables
5. Discussion
This study aimed to investigate the relationship between mindfulness and death anxiety in patients diagnosed with cancer. Specifically, we explored the potential mediating role of cancer self-efficacy in this association. The first finding of our study indicated that the relationship between mindfulness and death anxiety in patients with cancer was not significant. This finding is inconsistent with the results of previous studies by Salmani and Zoghi (33) and Narimani et al. (34).
It is worth noting that in the aforementioned studies (33, 34), the relationship between mindfulness and death anxiety was examined using correlation and regression analyses, which yielded significant results. In contrast, the present study employed SEM to test the hypotheses. While the Pearson correlation test in our study revealed a significant relationship between mindfulness and death anxiety, the structural model showed that the total effect of mindfulness on death anxiety was mediated by the intervening variables. In other words, mindfulness did have an impact on death anxiety, but this effect was indirect.
This finding can be explained by the definition of mindfulness as the intentional and non-judgmental awareness of the present moment, without being caught up in mental narratives or intrusive thoughts. This type of mindset is typically associated with reduced stress and anxiety, as individuals focus on experiencing the present instead of dwelling on unpleasant past or future thoughts (33). Numerous studies have demonstrated that mindfulness practices can effectively reduce anxiety and stress levels. In the context of death anxiety, focusing on the present moment can help individuals cope better with this challenging experience. Many patients with cancer grapple with death anxiety, as a significant part of the cancer experience involves various concerns about the future and the end of life. Research has shown that mindfulness can help reduce death anxiety in patients with cancer (12). Mindfulness is a method based on focusing on the present moment and accepting current experiences (34). By practicing mindfulness, patients can better manage their unpleasant emotions, negative thoughts, and stress, and focus on the present instead of ruminating about the past or worrying about the future.
Furthermore, the results showed a significant negative relationship between cancer self-efficacy and death anxiety. In other words, higher levels of cancer self-efficacy were associated with lower levels of death anxiety. This finding is consistent with the results of studies conducted by Khamoshi Darmarani and Moradi (35) and Karatas et al. (36).
Individuals with high self-efficacy have higher motivation and believe they can employ the necessary metacognitive skills to utilize coping strategies, manage resources effectively for task completion, and monitor their performance. In contrast, individuals with low self-efficacy lack confidence in their abilities to succeed, have lower motivation, and may procrastinate in starting or completing tasks (36). Self-efficacy can act as a crucial personality factor in dealing with life's challenges and pressures. It can influence how much individuals strive and exhibit resilience in the face of life's adversities and stressors, ultimately reducing their susceptibility to anxiety and death anxiety. High self-efficacy facilitates a sense of ease and accomplishment when approaching challenging tasks or actions, and these successes contribute to the formation of strong beliefs in one's own competence (35).
Furthermore, the results revealed a significant mediating role of cancer self-efficacy in the relationship between mindfulness and death anxiety. To the best of our knowledge, no previous study has examined this specific mediation model. While the first hypothesis indicated no direct relationship between mindfulness and death anxiety, the indirect pathway showed that mindfulness was associated with increased cancer self-efficacy, which in turn led to reduced death anxiety in patients. These findings suggest that cancer self-efficacy effectively mediates the relationship between mindfulness and death anxiety.
Mindfulness can be defined as the intentional and non-judgmental awareness of the present moment. It involves focusing on the present, accepting experiences and emotions without judgment, and fostering a deeper connection with oneself and others. Mindfulness can help individuals better cope with stress, anxiety, and pain. Self-efficacy, on the other hand, refers to one's belief in their ability to handle challenges and achieve their goals. Increased self-efficacy can enhance one's determination and motivation to endure the challenging treatments of cancer. Considering these two factors, studies have shown that mindfulness can increase self-efficacy in patients with cancer and expedite the acceptance of difficult treatments. Through mindfulness practices, individuals can confront the stress and concerns associated with cancer, thereby enhancing their self-efficacy and promoting overall well-being. Since cancer is often accompanied by fear and uncertainty about the future, many patients with cancer experience death anxiety. By practicing mindfulness, individuals can strengthen their self-efficacy and discover optimal coping mechanisms to deal with the most challenging situations, ultimately reducing death anxiety.
The generalizability of the findings is a potential limitation. The sample was restricted to cancer patients in Tehran, Iran, which may limit the applicability of the results to patients with other chronic diseases or in different geographic regions. Furthermore, the use of self-report measures introduces the possibility of self-report bias. Social desirability bias, where participants may overreport positive attributes or underreport negative ones, could have influenced the results. While self-report measures are a common tool in psychological research, it is essential to consider the potential limitations of this approach. Future studies could address these limitations by including a more diverse sample and employing a combination of self-report and objective measures to enhance the validity of the findings.
5.1. Conclusions
The findings revealed that mindfulness did not directly influence death anxiety. However, a significant indirect effect of mindfulness on death anxiety emerged when mediated by cancer self-efficacy. These results suggest that mindfulness interventions may benefit patients with cancer by enhancing their self-efficacy in managing their disease, which in turn could lead to reduced death anxiety. Future research should explore the specific mechanisms by which mindfulness fosters cancer self-efficacy and reduces death anxiety. Additionally, longitudinal studies examining the long-term effects of mindfulness interventions on these outcomes are warranted. By elucidating the interplay between mindfulness, cancer self-efficacy, and death anxiety, this research can inform the development of more effective psychological interventions to improve the well-being of patients with cancer.