1. Background
Today, with the emergence of different epidemic diseases, many countries face new economic, social, political, and especially Health problems (1, 2). COVID-19, a widespread pandemic disease, had a profound impact on People due to its high prevalence and creation of different disabilities in recent years (3).
Human resources are the most important asset of each community (4). Since the COVID-19 pandemic started, this disease spread in different communities across various countries at different time-points (5). More than 6 million people lost their lives to COVID-19 by the end of July 2022 (6). The number of confirmed COVID-19 cases in Iran was more than 7 million by May 2022 (7). Therefore, Iranians are one of the most affected societies and probably have adequate relevant experience to recall their behaviors during the pandemic. With the outbreak of COVID-19 in various communities, the fear of contracting COVID-19 has become another stressful concern for societies (8, 9).
Studying and identifying individual and social behaviors of people in different countries can be very effective in designing and implementing prevention and health programs (10). A more effective and better health plan can be provided by identifying the behaviors of various communities, which will result in greater efficiency of prevention models (11).
Protecting human health and utilizing effective preventive methods before different infections are the most important goals of health specialists in workplaces (12). Although no reliable data have been released on the exact number of Iranian men affected by COVID-19 (up to the time of writing this article), this cannot undermine the importance of designing and implementing preventive health care recommendations in this community
2. Objectives
The current study tries to understand the concepts of COVID-19 preventive behaviors from Iranian Men’s perspective during a pandemic.
3. Methods
3.1. Qualitative Approach
This qualitative study employed the content analysis technique. Content analysis has been defined as a research technique for the reproducible and valid inference of data (13). Standards for reporting qualitative research (SRQR) were observed during the study and reporting of the results.
3.2. Participants
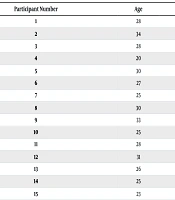
Of the 20 participants enrolled in the study, 5 withdrew from the study at the interview and were thus excluded. Overall, the participants consisted of 15 Persian-speaking Iranian men aged over 20, in Tehran city. Their demographic parameters (age, educational level, field of study, and work experience) are presented in Table 1.
| Participant Number | Age | Educational Level |
|---|---|---|
| 1 | 28 | MSc |
| 2 | 34 | MSc |
| 3 | 28 | MSc |
| 4 | 20 | Associate degree |
| 5 | 30 | MSc |
| 6 | 27 | Associate degree |
| 7 | 25 | Associate degree |
| 8 | 30 | BSc |
| 9 | 33 | BSc |
| 10 | 25 | BSc |
| 11 | 28 | Associate degree |
| 12 | 31 | MSc |
| 13 | 26 | BSc |
| 14 | 25 | BSc |
| 15 | 23 | BSc |
Socio-demographic Characteristics of Participants
3.3. Sampling Strategy
Participants were selected using purposive sampling. Prior to the interview, written and oral consents were obtained from all the participants. The sample size was determined based on saturation, continuing until no new concepts or content emerged from the participants.
3.4. Collecting Data
Data was collected through individual in-depth unstructured interviews with the target population. After conducting the interviews, the qualitative data were analyzed using directed content analysis. Interviews were completed over a period of three months. Each interview was conducted in one day and lasted between 35 - 45 minutes.
At the beginning of each interview, and after receiving written and oral consents from the participants, individuals were first briefed on the purpose of the study. An attempt was made to create a friendly atmosphere before the interview. Demographic information was then collected. The participant was asked how he felt about the COVID-19 disease in general. Subsequent questions were selected using the probing method, based on the purpose of the study.
The interviews were completely noted down by the interviewer. After each interview, the notes were typed, and the contents of the interviews were reviewed regularly to extract codes.
3.5. Data Analysis
The three main stages followed in data analysis in this study included: (1) Theoretical stage: In this stage, the information was prearranged through an early review of the documents; (2) descriptive-analytical stage: The interviews were defined and analyzed, and units of meaning were specified and then coded upon compression; (3) interpretive stage: Qualitative content analysis was used to interpret the interviews according to the categories and subcategories. Each transcript was read and reviewed numerous times by three authors. The authors described the aim of content analysis as confirming the extracted themes, concepts, and their particular meanings (14). The codes were categorized by their conception and similarity, and simultaneously, dissimilarities between them were used to exclude inappropriate groupings (15).
3.6. Trustworthiness
The trustworthiness of the extracted data was ensured based on earlier studies. To guarantee the quality of results, Lincoln et al.’s criteria were considered (16). The four strategies used for trustworthiness included prolonged engagement with data, member checking, peer debriefing, and external checking. Investigators' involvement: The researchers were continuously engaged in reviewing, discussing, coding, and revising processes to enhance the depth and breadth of data collection and interpretation. Data collection lasted about three months, during which the researchers maintained a focused and thorough approach; member checking: The target population was asked to review, revise, or approve the units of meaning and extracted codes to ensure harmony between the collected data and the participants' experiences; peer debriefing and external checking: All interviews, units of meaning, extracted codes, themes, categories, and sub-categories were reviewed and revised by several health professional colleagues until trustworthiness was established (17). To enhance transferability, a comprehensive description of the full research procedure was provided, and participants were quoted directly.
3.7. Ethical Approval
This project was conducted in accordance with the ethical principles and national norms and standards for conducting medical research in Iran (approval ID: IR.AJAUMS.REC.1400.146). Participants were informed about the study, and verbal and written informed consents were obtained from them individually. To maintain the participants’ confidentiality, their real names were not used; instead, aliases were assigned for the quotations.
4. Results
In this study, a total of 15 men with an average age of 27.53 ± 3.61 years and a mean work experience of 25.26 ± 21.69 months were included (Table 1). Overall, 939 primary codes (including repeated codes) were extracted from the interviews after data analysis. Subsequently, 5 themes, 13 categories, and 38 sub-categories were identified based on the collected codes (Table 2).
| Themes and Categories | Sub-categories |
|---|---|
| Emotional perception of COVID-19 | |
| Negative feelings toward COVID-19 | Perceived sense of danger toward COVID-19 |
| Fear of the COVID-19 Outbreak | |
| No worries about COVID-19 | No fear of COVID-19 |
| Readiness to confront the disease | |
| COVID-19 awareness | |
| The nature of the disease | Contagious/speed of spreading |
| General features of COVID-19 | |
| Hypersensitivity of high-risk groups | |
| Infection and mortality rates | |
| Stability of COVID-19 | |
| Recovering from the disease | Features of the recovery period |
| Attitudes toward treatment strategies | |
| Disease symptoms | Respiratory symptoms |
| Non-respiratory symptoms | |
| Routes of transmission | Transmission through contact with contaminated surfaces |
| Transmission through non-compliance with personal hygiene | |
| Transmission through non-observance of social distancing | |
| Airborne transmission | |
| Diagnostic methods | Diagnosis through laboratory testing |
| Diagnosis through symptoms | |
| Perceived barriers to COVID-19 prevention | |
| Individual barriers to COVID-19 prevention | Negligence |
| Misconceptions | |
| Lack of awareness toward COVID-19 | |
| Fear and anxiety | |
| Social barriers to COVID-19 prevention | Non-organizational barriers |
| Barriers resulting from social determinism and the necessities of life | |
| Perceived social measures to prevent COVID-19 | |
| Improving social skills and behaviors | Raising awareness and information about COVID-19 prevention |
| Strengthening role modeling in the society | |
| The necessity of creating a platform and culture for social distancing | |
| Revising rules and reforming infrastructure | Imposing restrictions |
| Providing facilities | |
| Individual steps taken to prevent COVID-19 | |
| Using personal protective equipment | Using masks |
| Using shields | |
| Using disinfectants | |
| Vaccination | |
| Prevention by following healthcare principles | Increased hand washing and cleaning |
| Proper nutrition | |
| Exercise | |
| Early detection of disease | |
| Observance of personal hygiene principles |
Themes, Categories, and Sub-categories Extracted from Data Analysis
The themes are described below.
4.1. Emotional Perception of COVID-19
Based on the interviews, the sub-category of fear of the COVID-19 outbreak had the most repeated codes in the negative feelings toward COVID-19 theme. The most repeated code in this sub-category was "being afraid of COVID-19 at the beginning of the epidemic," which appeared six times.
In addition, a perceived sense of danger toward COVID-19 was reported by two participants. One of the participants (#10) expressed his anxiety about the danger of COVID-19 as follows:
“…. Honestly, when I hear something about COVID-19, I think I should go into quarantine, not travel, and be cautious, not just for myself, but for my family, and even others. I don’t have a good feeling about it. I think nobody is happy about it. I mean, we are afraid of it”.
On the other hand, No fear of COVID-19 was the sub-category of no worries about COVID-19 with the most repeated codes in this category. Two participants declared that they were not worried about COVID-19 as much as before. One participant (#15) mentioned:
“If a person infected with COVID sits next to me, I'm no longer afraid of him…”.
4.1.1. COVID-19 Awareness
The non-respiratory symptoms sub-category of the disease symptoms category contained the most repeated codes in the COVID-19 awareness theme. The most repeated codes in this sub-category were fever as one of the main symptoms of COVID-19, severe bodily pain, and different signs in different people. Some participants were aware of the elderly’s greater susceptibility to COVID-19 compared to others. The COVID-19 awareness theme also highlighted that people are aware of the lack of specific treatment for COVID-19 and that consuming soup and fresh fruits is beneficial when affected by the disease.
Some of the participants’ declarations are presented below:
Participant 9: “…. Symptoms such as cough, sneezing, sore throat, and fever are the main symptoms of COVID-19.”
Participant 12: “…. When I got COVID-19, I had all the symptoms of body ache, headache, diarrhea, etcetera.”
Participant 13: “…. It has different symptoms. Symptoms can range from fever and chills to sore throat, headache, and dizziness.”
Moreover, in the non-respiratory symptoms sub-category, participant 2 mentioned the following, which could be a sign of underestimating the disease:
“…. COVID didn’t knock me down when I got it”.
4.2. Perceived Barriers to COVID-19 Prevention
Misconceptions and barriers resulting from social determinism and the necessities of life were the sub-categories with the most repeated codes in the categories of Individual Barriers to COVID-19 prevention and social barriers to COVID-19 Prevention, respectively. Resistance toward receiving the COVID-19 vaccine was mentioned twice in the sub-category of misconceptions. Additionally, the expensive price of the COVID-19 test was reported twice in the sub-category of barriers resulting from social determinism and the necessities of life.
Participant 2: “…. Some people are afraid of the COVID-19 vaccine and say it has side-effects, but we did not experience anything special. It was only a mild fever. Some say it has no effect”.
Participant 5: “…. Well, the COVID test is expensive, so many may not be willing to perform it…”.
4.3. Perceived Social Measures to Prevent COVID-19
Improving social skills and behaviors and revising rules and reforming infrastructure were the sub-categories of the necessity of creating a platform and culture for social distancing and providing facilities, which contained the most repeated codes in these categories.
Participants indicated that staying at home during infection with COVID-19 is one of the most important social behaviors for preventing the spread of COVID-19. Additionally, the need to lower the price of masks for affordability was emphasized by two participants.
Participant 1: “…. If we are infected, we should stay at home so we don’t pass the disease on to others. Many people infected with COVID-19 don’t care about resting and leave home and infect other people. This is how the incidence of COVID increases”.
Participant 4: “…. The price of masks should also be lowered so that people can afford to buy them”.
4.4. Individual Steps Taken to Prevent COVID-19
Using masks (repeated 105 times) and increased washing and cleaning (repeated 104 times) were the most repeated codes in the sub-categories of using personal protective equipment and prevention by following healthcare principles.
Washing hands to prevent COVID-19 was repeated seven times in the sub-category of prevention by increased Washing and Cleaning.
Participant 3: “…. We must wear masks and have them with us wherever we go. I try to wear a mask wherever I go”.
Participant 7: “…. As soon as the hands are washed, the coronavirus, if it is on the hands, will be washed away and removed from the hands. So, it is necessary to wash our hands”.
5. Discussion
In this study, five themes with different categories and sub-categories related to the concept of COVID-19 were extracted through individual in-depth unstructured interviews with Iranian men. This study indicated that while some participants were afraid of COVID-19, others were not.
A study conducted on the knowledge, attitudes, practices, and fear of COVID-19 among adult Iranians from April to May 2020 demonstrated that fear of COVID-19 was associated with the use of social media as a source of information (18). Another study on COVID-19 anxiety reported that fear of COVID-19 decreased with knowledge about the pandemic, educational status, and age in Chilean adults from middle- and high-income levels between 10th July 2020 and 10th August 2020 (19). Moreover, it has been hypothesized that childhood experiences of severe acute respiratory syndrome (SARS) have an imprinting effect on the fear of COVID-19 in general undergraduate students in Chinese universities (20). Furthermore, a study conducted in 2021 in a central region of Iran showed that the majority of the participants were worried about their family and friends contracting COVID-19 (21). On the other hand, the reduction in anxiety toward COVID-19 over time could be a sign of adaptation and normalization of the disease (22).
Here, some participants believed that cough was more common than other symptoms of COVID-19. Although this inference could be the result of the participants’ personal experiences with the disease, they should be informed that symptoms vary among individuals. In the features of the recovery period sub-category, some participants reported dissimilar recovery periods. The recovery times mentioned varied between 10 days, 2 weeks, and 2 to 3 weeks. Thus, participants needed to be informed that there is no definite recovery time for COVID-19. Another significant code that emerged in the features of the recovery period sub-category was the perception of a boosted immune system caused by contracting COVID-19. This could lead to the misconception that exposing oneself to the virus intentionally might improve immunity, which requires correction and proper awareness.
In connection with COVID-19 awareness, a study on the knowledge, attitude, and practice toward COVID-19 in a general population of Iranians indicated that the most common symptoms of this disease were shortness of breath, dry cough, and fever or headache (23). Another study by Mukhlis et al. reported that Indonesians identified fever, dry cough, and fatigue as the primary symptoms of COVID-19 infection (24). In a qualitative study on Iranian health professionals and experts, participants agreed that people aged over 50 were more susceptible to COVID-19 (21).
Concerning food consumption during the COVID-19 pandemic, some participants claimed that they consumed more healthy foods and fruits during the pandemic. In relation to this, Caso et al. reported that, with the increase in healthy food intake and cooking, junk food consumption decreased during the lockdown caused by the COVID-19 outbreak in Italy (25). This shift could indicate increased awareness of the positive effects of healthy foods, such as soups and fruits, for COVID-19 prevention.
High transmission of the disease through communication with infected people was another code extracted under COVID-19 awareness. This code demonstrated that participants had an acceptable level of awareness regarding the social transmission of the disease. In fact, person-to-person transmission is one of the most significant sources of the disease (26).
The participants had a particular impression of the PCR tests for COVID-19 diagnosis. Although before 2022, people in different countries were uncertain about the reliability of PCR tests when experiencing COVID-19-like symptoms (27), this study, along with others, showed that most people used PCR tests for COVID-19 diagnosis (28).
Previous studies have shown that there are various public misconceptions about COVID-19 among people. For instance, a study by Carlson et al. revealed that both policymakers and citizens held incorrect beliefs about how climate influences exposure to and transmission of COVID-19 (29).
Additionally, other studies reported misconceptions such as the deadly nature of the novel coronavirus, the belief that hand sanitizers can completely destroy the virus, the notion that drying hands with a hand dryer prevents infection, and the perception of the COVID-19 vaccine as unsafe (30, 31).
This study highlighted some important administrative determinants in preventing COVID-19. While some participants expressed satisfaction with managerial policies in their centers, the high cost of the COVID-19 test and the insufficient supply of masks were the most commonly cited barriers by several participants.
In the individual barriers to COVID-19 prevention category, some participants admitted to going out with friends despite being infected with COVID-19. In the social barriers to COVID-19 prevention category, one participant noted that insufficient information had been provided about the COVID-19 vaccines produced in different countries.
These findings emphasize the necessity of designing and implementing comprehensive health education programs to address these gaps and promote better preventive behaviors among the population.
Similar to the complaints made by our participants about the high price of COVID-19 diagnostic tests, people from other countries have also expressed this concern (32, 33). Therefore, governments are expected to provide adequate facilities to support the detection and prevention of COVID-19.
Regarding the use of personal protective equipment, some participants believed that N95 masks should be used to prevent COVID-19. However, it has been established that N95 masks are not necessary for everyone to prevent COVID-19 (34, 35). Additionally, some participants thought face masks should be changed and replaced every other day, whereas most health organizations recommend changing or washing face masks daily (36). In the sub-category of vaccination prevention, one participant believed he wouldn’t be infected with COVID-19 because he had already received the COVID-19 vaccine. However, various studies have shown that COVID-19 vaccines are not 100% effective (37). These observations once again underscore the importance of implementing comprehensive health education programs to address these misconceptions and educate the public effectively.
Earlier studies indicate that improving social prevention skills through various educational plans, particularly via media, has a significant impact on reducing the number of new COVID-19 cases (38, 39). On the other hand, while social media can effectively raise public awareness about COVID-19, it can also contribute to creating panic during the pandemic. Thus, there is a critical need to monitor social media programs to ensure accurate and balanced information is disseminated (40).
5.1. Conclusions
This study revealed that the perceived challenges of COVID-19 prevention exhibit significant variety and complexity at both individual and social levels. Certain managerial determinants were identified as critical among the personnel concerning COVID-19 prevention. The necessity of creating a platform and fostering a culture for social distancing emerged as another barrier, closely tied to governmental rules and the need for infrastructure reform. Furthermore, a lack of awareness among people about COVID-19 prevention was evident. Therefore, it is essential for policymakers and health educators to acknowledge and address the diversity and complexity of these challenges when designing and implementing health education programs.
The results of this study, along with earlier research, can play a crucial and effective role in the design and implementation of health empowerment plans for COVID-19 prevention. Accordingly, there should be a strong emphasis on raising awareness, addressing and removing barriers, and creating incentives to promote preventive behaviors.
This study was conducted during the COVID-19 pandemic, which, to some extent, limited the planning and coordination of participant contributions.