1. Background
Sociodemographic traits, cultural background, psychosocial factors, and lifestyle choices may influence the severity of menopausal symptoms (1). A study (2) has indicated that North American and European women report higher rates of symptoms compared to Asian women. In Latin America (3) and Australia (4), menopause was linked to hot flushes, followed by sleep disturbances and night sweats. However, in Nigeria (5), joint and muscular discomfort was the most commonly reported symptom. The most prevalent menopausal symptoms were joint pain, fatigue, headache, sleep disturbances, and physical and mental exhaustion among Egyptian (6) and Saudi women (7). Women from the East and South-East Asia (SEA) countries suffered from joint and muscle pain as the most frequent complaint (8). The menopausal symptoms mentioned above are the primary factors contributing to a decline in health-related quality of life (HR-QoL). The Menopause Rating Scale (MRS), an HR-QoL scale, has been used as an instrument to assess the frequency of menopausal symptoms among middle-aged women in Malaysia (9), Northern India (10), Sri Lanka (11), Pakistan (12), and Ecuador (13); one study (14) found in middle-aged Bangladeshi women using the MRS scale. The study participants were the Bihari women of the Mohammadpur Geneva camp (MGC) in Dhaka, Bangladesh. The Biharis, an Urdu-speaking minority group, including the Bihari women of the Geneva camp originally and mainly from the Indian province of Bihar, were the young Muslim refugees who migrated from India to East Pakistan (now Bangladesh) after the partition of 1947 to escape communal unrests and retain their religious identity (15). One clear sign of aging occurs when a woman’s menstrual periods stop permanently. A woman enters this stage in middle age, and these women of our country are not getting enough support due to poor socioeconomic conditions, illiteracy, ignorance, and an inadequate healthcare system (16). During this period, women were not well accepted in society and family and considered themselves a burden. The middle-aged women from the Geneva camp in our country have already been leading wretched lives. The MRS can be used as a screening tool to identify women needing referral to a higher level of care for severe menopausal symptoms. Compared to mainstream Bangladeshi women, Bihari women have significantly less access to health-related interventions.
While research on menopause and QoL has primarily focused on women in mainstream Bangladeshi society (14, 17-21), it is essential to examine the QoL of middle-aged Bihari women.
2. Methods
This descriptive cross-sectional study was conducted from November to March 2019 in the MGC, Dhaka. Considering the inclusion and exclusion criteria, this research used a convenient sampling technique to include 1,200 postmenopausal (PMS) women. Menopausal symptoms are key contributors to the decline in HR-QoL among PMS women. The sample size for this study was determined based on the objective of assessing sleep disturbances, a common menopausal symptom. An estimated prevalence of 52.2% for sleep problems, reported in a previous study (9) among Malaysian PMS women, was used to guide the calculation. The sample size was calculated using the standard formula for estimating a proportion: n = z²pq/d², where n = required sample size, z = standard normal deviate (1.96 for a 95% confidence level), p = estimated prevalence (0.522), q = 1 - p (0.478), and d = margin of error (0.05). Substituting these values yielded the minimum required sample size. The sample size was increased to compensate for an anticipated 10% nonresponse rate. This adjustment ensured adequate statistical power even with participant attrition or exclusion. Ultimately, the sample size was rounded to 1,200 to maintain statistical validity and operational feasibility. The study included women aged 45 to 75 who experienced menopause within the last two years. Exclusions were made for women with other medical complications, recent antibiotic use, undergoing hormone replacement therapy (HRT), or unable to answer basic sociodemographic questions. We divided the questionnaire into three sections. Section 1 outlined the sociodemographic data, including age, marital status, educational level, occupation, and average household income. Section 2 included the time since menopause, BP, and women's body weight. Section 3 included the MRS questionnaire for assessing menopausal symptoms in this study. The MRS scale (22) is a self-administered instrument, and this scale is validated. Eleven items are present in the MRS scale, and it has three subscales: (1) Somatic-hot flushes, heart discomfort/palpitation, sleeping disorder, and muscle and joint problems; (2) psychological-depressive mood, irritability, anxiety, and physical and mental exhaustion; and (3) urogenital-sexual problems, bladder problems, and dryness of the vagina. Each item was graded by the PMS women from 0 (not present) to 4 (1 = mild, 2 = moderate, 3 = severe, 4 = very severe). A group of experienced health workers and language experts first translated the questionnaire into the local language (Bangla) and then back to English to validate the language validation. Thirty women participated in a pilot study to validate the translated MRS questionnaires. Finally, the reliability analysis was done on the modified MRS questionnaires with Cronbach's alpha. MRS questionnaires with Cronbach's alpha of somatic subscale was 0.71, psychological subscale 0.73, and urogenital subscale 0.82, respectively, in this study. Trained health personnel asked women about their experiences regarding the menopausal symptoms in the previous month (30 days); however, it has been noted from the earlier study (9) that the women did not seem able to rate the scale by themselves. To minimize these difficulties, we conducted face-to-face interviews. We calculated the frequency for descriptive analysis. We performed multivariable regression analysis to identify the predictors of QoL among PMS women. Statistical tests were considered significant at P-values ≤ 0.05. We conducted all statistical analyses using the software SPSS 22.0 for Windows (SPSS, Inc., Chicago, IL, USA). The Ethics and Research Review Committees of the BUHS (BUHS/BIO/EA/19/183) approved the study ethically.
3. Results
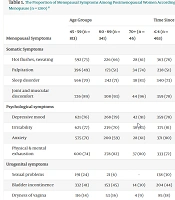
Table 1 shows somatic symptoms were experienced among women in the form of hot flushes, sweating (73%), palpitation (74%), sleep disorder (83%), and joint and muscular discomfort (96%) during the age of 45 - 59, 60 - 69, and 70+ years old respectively. The highest number of women (91%) experienced depressive mood at the age of 70+. Anxiety (71%) was high in the 45 - 59 age-old. About 83% felt irritability in the 70+ age group, and 82% suffered from physical and mental exhaustion at 60 - 69 years old. Regarding the urogenital problem, 45% had bladder incontinence between the ages of 60 and 69. At the time since ≤ 4, 5 - 10, 11 - 15, and 16+, somatic symptoms were experienced among women in the form of hot flushes, sweating (78%), palpitation (51%), sleep disorder (75%), and joint and muscular discomfort (91%) respectively. The highest number of women who experienced depressive mood (81%) and exhaustion (85%) had menopause of 16+.
| Menopausal Symptoms | Age Groups | Time Since Menopause (y) | |||||
|---|---|---|---|---|---|---|---|
| 45 - 59 (n = 813) | 60 - 69 (n = 341) | 70+ (n = 46) | ≤ 4 (n = 463) | 5 – 10 (n = 392) | 11 - 15 (n = 150) | 16+ (n = 195) | |
| Somatic Symptoms | |||||||
| Hot flushes, sweating | 592 (73) | 226 (66) | 28 (61) | 363 (78) | 273 (70) | 96 (64) | 114 (59) |
| Palpitation | 396 (49) | 173 (51) | 34 (74) | 238 (51) | 199 (51) | 70 (47) | 96 (49) |
| Sleep disorder | 566 (70) | 242 (71) | 38 (83) | 340 (73) | 255 (65) | 112 (75) | 139 (71) |
| Joint and muscular discomfort | 726 (89) | 308 (93) | 44 (96) | 359 (78) | 347 (89) | 132 (88) | 178 (91) |
| Psychological symptoms | |||||||
| Depressive mood | 621 (76) | 268 (79) | 42 (91) | 359 (78) | 299 (76) | 116 (77) | 157 (81) |
| Irritability | 625 (77) | 239 (70) | 38 (83) | 375 (81) | 275 (72) | 110 (73) | 142 (73) |
| Anxiety | 575 (71) | 200 (59) | 28 (61) | 371 (80) | 230 (59) | 87 (58) | 115 (59) |
| Physical & mental exhaustion | 600 (74) | 278 (82) | 37 (80) | 333 (72) | 287 (73) | 130 (87) | 165 (85) |
| Urogenital symptoms | |||||||
| Sexual problems | 191 (24) | 21 (6) | - | 138 (30) | 58 (15) | 10 (7) | 6 (3) |
| Bladder incontinence | 332 (41) | 153 (45) | 14 (30) | 204 (44) | 155 (40) | 58 (39) | 82 (42) |
| Dryness of vagina | 116 (14) | 53 (16) | 4 (9) | 85 (18) | 50 (13) | 20 (13) | 18 (9) |
The Proportion of Menopausal Symptoms Among Postmenopausal Women According to Their Age Group and Time Since Menopause (n = 1200) a
We conducted multivariable linear regression analyses to identify the factors that might predict PMS women’s QoL (Table 2). All eight parameters, namely, age, occupation, education, marital status, time since menopause, monthly income, systolic blood pressure (SBP), and diastolic blood pressure (DBP) were included simultaneously in the regression model. Time since menopause, education, occupation, monthly income, marital status, SBP, and DBP showed significant association with MRS subscale scores; three individual models were fitted separately for each considerable parameter. Predictions of the total somatic scores with sociodemographic and clinical characteristics achieved an R² of 0.023; P = 0.0001; respondents who were economically solvent had a significant negative association (P = 0.03; 95% CI: -0.672 to -0.019) with the hot flushes, palpitation, sleeping problem, and muscle and joint pain. SBP was positively and significantly (P = 0.008; 95% CI: 0.083 to 0.556) associated with somatic symptoms. Regression analysis also found significant predictions of respondents’ psychological scores with sociodemographic and clinical parameters (R² = 0.081; P = 0.0001). Occupation (P = 0.0001; 95% CI: 0.450 to 1.000) and marital status (P = 0.001; 95% CI: 0.220 to 0.872) had a positive significant association with psychological symptoms. Education (P = 0.0001; 95% CI: -2.284 to -0.913) and time since menopause (P = 0.0001; 95% CI: -0.607 to -0.188) were negatively significantly associated with depressive mood, irritability, anxiety, physical and mental exhaustion. However, SBP (P = 0.0001; 95% CI: 0.438 to 0.963) had a significant positive effect on the psychological scores, and in contrast, DBP (P = 0.05; 95% CI: -0.416 to 0.008) was significant and negatively associated with the scores after adjustment. The significant predictions of respondents’ urogenital scores with sociodemographic and clinical parameters (R² = 0.034; P = 0.0001). Occupation (P = 0.017; 95% CI: 0.031 to 0.319) and education (P = 0.001; 95% CI: 0.265 to 0.983) significantly positively affected the urogenital scores. Marital status (P = 0.001; 95% CI: -0.458 to -0.117), SBP (P = 0.007; 95% CI: 0.051 to 0.326), and DBP (P = 0.032; 95% CI: -0.232 to -0.011) were significantly and negatively associated with the urogenital score after adjustment.
| Predictor Variables | B a ± SE | Beta b | P-Value | 95% CI for B | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Somatic score c | |||||
| Present age (y) | 0.0001 ± 0.17 | 0.0001 | 0.997 | -0.336 | 0.337 |
| Occupation | -0.038 ± 0.12 | -0.01 | 0.764 | -0.286 | 0.210 |
| Level of education | -0.330 ± 0.32 | -0.03 | 0.295 | -0.948 | 0.288 |
| Marital status | 0.245 ± 0.15 | 0.05 | 0.103 | -0.049 | 0.538 |
| Time since menopause (y) | -0.013 ± 0.096 | -0.004 | 0.889 | -0.202 | 0.175 |
| Monthly income (BDT) | -0.346 ± 0.16 | -0.06 | 0.03 | -0.672 | -0.019 |
| SBP (mmHg) | 0.320 ± 0.121 | 0.104 | 0.008 | 0.083 | 0.556 |
| DBP (mmHg) | 0.120 ± 0.09 | 0.048 | 0.218 | -0.071 | 0.311 |
| Psychological score d | |||||
| Present age (y) | 0.153 ± 0.19 | 0.023 | 0.423 | -0.221 | 0.526 |
| Occupation | 0.725 ± 0.14 | 0.16 | 0.0001 | 0.450 | 1.000 |
| Level of education | -1.59 ± 0.35 | -0.128 | 0.0001 | -2.284 | -0.913 |
| Marital status | 0.546 ± 0.166 | 0.099 | 0.001 | 0.220 | 0.872 |
| Time since menopause (y) | -0.398 ± 0.11 | -0.104 | 0.0001 | -0.607 | -0.188 |
| Monthly income (BDT) | 0.029 ± 0.185 | 0.005 | 0.877 | -0.334 | 0.391 |
| SBP (mmHg) | 0.701 ± 0.134 | 0.199 | 0.0001 | 0.438 | 0.963 |
| DBP (mmHg) | -0.204 ± 0.108 | -0.071 | 0.05 | -0.416 | 0.008 |
| Urogenital score e | |||||
| Present age (y) | -0.088 ± 0.10 | -0.026 | 0.38 | -0.28 | 0.11 |
| Occupation | 0.175 ± 0.073 | 0.076 | 0.017 | 0.031 | 0.319 |
| Level of education | 0.624 ± 0.183 | 0.098 | 0.001 | 0.265 | 0.983 |
| Marital status | -0.287 ± 0.087 | -0.102 | 0.001 | -0.458 | -0.117 |
| Time since menopause (y) | -0.053 ± 0.056 | -0.027 | 0.343 | -0.163 | 0.057 |
| Monthly income (BDT) | -0.003 ± 0.097 | -0.001 | 0.977 | -0.192 | 0.187 |
| SBP (mmHg) | -0.189 ± 0.07 | -0.105 | 0.007 | 0.051 | 0.326 |
| DBP (mmHg) | -0.121 ± 0.057 | -0.083 | 0.032 | -0.232 | -0.011 |
Multivariable Regression Analysis of the Total Somatic, Psychological, and Urogenital Scores as Dependent Variables with Sociodemographic and Clinical Characteristics Among Postmenopausal Women (n =1200)
4. Discussion
The most stated symptoms among a sample of Bihari PMS women in the present study were hot flushes, sweating, palpitation, sleep disorder, joint and muscular discomfort, depressive mood, anxiety, physical and mental exhaustion, and bladder incontinence according to the age group and time since menopause. Ahmed et al. (21) reported that tiredness, dizziness, depression, hot flushes, osteoporosis, sweating at night, irritability, palpitation, and headache had the worst impact on QoL among early and late menopausal Bangladeshi women. Women in India (23, 24), Pakistan (25), and Saudi Arabia (7, 26) were also experiencing the symptoms mentioned above. However, PMS women from other Asian populations (8, 11) were similar to our results. It is important to note that although all women in the study were symptomatic, the QoL decreased when the severity of symptoms increased. Consequently, the severity of symptoms correlates with the QoL in reverse. Hot flushes and night sweats are related to hormonal changes during menopause, and menopause has changed the female reproductive system mainly by changing hormone levels. Joint and muscular discomfort occurred due to the deficiency of a balanced and calcium-rich diet.
Multivariable regression analysis also showed that the increase in the time since menopause significantly impacted the QoL. About sixty-five percent of women included in the present study have experienced menopause for approximately a decade. Our results are in harmony with the Iranian studies (27) but did not match with other studies (28). This controversy happened because of the different data analysis methods and the study population. However, women became habituated to the menopause stage as time passed since menopause. Poor education led to depressive mood, irritability, anxiety, physical and mental exhaustion, and sexual problems. In contrast, different studies (23, 27) showed opposite results. The probable reasons are that educated people tend to have improved lives through their healthy behavior and positive lifestyles. Living conditions in the camps are unhygienic, water and sanitation systems are inadequate, and they have little chance to explore a better lifestyle. Economic conditions are equally important as education in one’s professional and social life, which could also improve QoL. A cross-sectional survey in India by Kakkar et al. (10) indicated that non-working and sedentary women significantly suffer from higher psychosomatic and urogenital disorders, which is in line with our study findings. The PMS women who were homemakers in our study suffered from hot flushes, palpitation, sleeping disorder, depressive moods, irritability, anxiety, bladder incontinence, and dryness of the vagina. Nazarpour et al. (27), Fallahzade et al. (1), and Haghi et al. (29) found similar results in their studies. The probable cause is that employed women tend to have better mental health than stay-at-home ones. Given their time in social settings outside the home, they are better able to resist the symptoms of menopause; a job or responsibility in an organization increases confidence levels among middle-aged women and helps to improve their QoL. On the other hand, homemakers are less exposed to the social environment outside their homes. They are mainly occupied with household chores, personally carrying out many of the tasks employed, financially secured independent women often assign to others. Therefore, the side effects of menopause might be associated with the burdens of household chores, which further complicate matters and reduce QoL. Marital status had a significant (P = 0.002) positive association with QoL among women. Loneliness and lack of intimacy in relations with the partner can extend and prolong the time of experiencing depression. The belief that one is loved, important, understood, and surrounded by care may improve the symptoms experienced by enabling more effective coping with them and thus contribute to well-being. Women with psychological symptoms fail to recognize their symptoms of menopause. As we know, in any third-world country, women are the most vulnerable group, constantly fighting to find their feet. In addition, women's condition is exaggerated if supplemented by diasporic notions like statelessness, displacement, migration, and refugee identity. These psychological symptoms may result from physical and mental stress due to living experiences in the MGC during midlife. Therefore, the women might have overrated their symptoms when MRS administered them.
The present findings indicate potential declines in physical health due to menopausal symptoms, increased vulnerability to mental health issues like depression and anxiety, and impaired social functioning stemming from stigma or limited support. Early identification of health issues can significantly improve HR-QoL in PMS women, who spend about one-third of their lives in this stage. Post-menopause technically begins after menstruation ends, with endocrine changes stabilizing within ten years, after which aging effects dominate. Many women in Geneva Camp experienced early menopause due to prolonged birth control use and were unaware of their last menstruation. They and their families often lack knowledge about the importance of a balanced diet, calcium, and sunlight. These factors, along with physiological changes, may lower their QoL. Providing proper nutrition and timely medical referrals could help them manage menopause better.
The findings of this study are subject to certain limitations in terms of generalizability. As the research was conducted within a single refugee camp in Dhaka, the results may not be representative of all PMS women living in other camps or marginalized settings across Bangladesh. The unique socio-cultural, economic, and environmental conditions of MGC could differ significantly from those of different refugee camps or underprivileged communities. To enhance the external validity of this research, future studies should consider replicating this investigation in other refugee settlements, urban slums, and marginalized populations in Bangladesh. Comparative studies across different camps could provide a more comprehensive understanding of the factors influencing QoL among PMS women and help design more targeted and culturally sensitive interventions.
The cross-sectional design did not account for the confounding effects of aging on symptom experience. An interviewer-administered questionnaire was used, leading to unavoidable recall bias. While this method was necessary due to the high illiteracy rate among participants, it introduced potential limitations discussed earlier in the method section. Additionally, participants' illiteracy resulted in a wide age range. The widespread illiteracy within the study population contributed to challenges in precisely determining participants' ages. Many respondents could not provide official documentation or exact birth dates, resulting in a broad and somewhat inconsistent age range among the study sample. These factors may have affected the precision of the data. A further limitation was the lack of comparable research involving women from other refugee camps.
The study found that the most commonly reported symptoms among PMS women were hot flushes, excessive sweating, palpitations, sleep disturbances, joint pain, depression, anxiety, fatigue, and bladder incontinence. QoL was significantly associated with factors such as education, occupation, income level, and marital status. Community-based health education programs focusing on menopause awareness, symptom management, and mental health support could empower women with knowledge and coping strategies. Training community health workers to address the specific needs of PMS women and integrating menopause care into existing primary healthcare systems can also make a noteworthy impact. These measures would improve health outcomes and promote dignity and well-being among this underserved population. Further research is recommended to enhance the well-being of PMS women across different Bihari communities in Bangladesh. In particular, future studies should adopt longitudinal designs better to explore the causal relationships between menopausal symptoms and QoL.