1. Background
The skin, the largest human organ, serves as an interface between an individual’s internal and external environments. As a highly visible organ, any physical changes to the skin are also socially observable. The clinical course of a wide range of skin diseases stems from a complex and often reciprocal interaction between biological, psychiatric, psychological, and social factors that can predispose, exacerbate, or perpetuate skin disorders, leading to both intrapersonal and interpersonal difficulties (1, 2). In this context, adolescence is a particularly sensitive stage of life (3), marked by significant physiological and psychological changes. These changes, coupled with hormonal fluctuations, can manifest in a variety of skin conditions (4), impacting adolescents’ self-image and well-being. While acne is a common concern during this period (5), adolescents may also experience other skin diseases such as alopecia, vitiligo, and psoriasis, each with its own unique challenges (6).
Skin diseases can significantly impact individuals’ overall well-being. The subjective nature of "quality of life" makes it difficult to define precisely (7). According to the World Health Organization, quality of life is an individual’s personal perception of their life circumstances, considering cultural factors, personal goals, and expectations (8). Therefore, self-reported quality of life is the primary indicator in research studies (9). It’s important to note that the impact of a skin condition can vary greatly among individuals, with some experiencing severe distress while others may only experience minor inconveniences (10).
The psychological and social factors influencing skin diseases remain understudied. Perceived stress plays a significant role in both the onset and exacerbation of these conditions and can also be a consequence of living with them (11, 12). Stress can contribute to the development or worsening of skin conditions through various physiological pathways, such as influencing immune system reactivity, potentially leading to inflammation and other skin issues (13, 14). Conversely, the presence of a skin condition can itself be a significant stressor, as visible skin changes may lead to self-consciousness, social anxiety, and feelings of stigmatization, all of which can increase perceived stress (15). This bidirectional relationship underscores the complex interplay between psychological and physical well-being in individuals with skin diseases. Perceived stress reflects an individual’s subjective appraisal of the severity of a stressor (16). Research suggests a strong association between skin diseases and stress, with a substantial proportion of cases potentially triggered or exacerbated by stress (17). The higher prevalence of skin diseases among adolescents may be partially attributable to the increased stress levels characteristic of this developmental period.
Contemporary research on the dynamic nature of parent-child relationships has refined psychological understanding of these bonds and their association with adolescent psychopathology (18). The parent-child relationship serves as a foundational interpersonal experience, crucial for establishing security and attachment (19). This relationship is characterized by a unique interplay of behaviors, emotions, and expectations specific to parents and their children. Research has demonstrated the significant influence of parental attachment and parent-child interactions on adolescent mental health, with positive relationships serving as a protective factor associated with improved psychological well-being (20). Adolescent skin conditions can impact the entire family system. Parents may experience stress, anxiety, and feelings of guilt or helplessness related to their child’s condition (21). Family routines may be disrupted by treatment regimens, and financial strain may arise due to medical expenses. Moreover, the adolescent’s emotional distress can affect family interactions and overall family functioning. Parent-child conflict tends to peak during adolescence, with relationship issues representing a prominent developmental concern (22).
Various studies have demonstrated that skin diseases significantly impact the health-related quality of life of affected individuals (23, 24). Given these findings, identifying factors influencing the quality of life of adolescents with skin diseases is crucial for developing effective preventive and therapeutic interventions to optimize outcomes for these adolescents and their families. Based on the presented literature, there is a clear need for interventions to address the challenges faced by these adolescents.
2. Objectives
Therefore, the present study aimed to investigate the correlation between perceived stress, parent-child relationships, and quality of life in adolescents with skin diseases.
3. Methods
This descriptive correlational study investigated adolescents with skin diseases (acne, alopecia, vitiligo, psoriasis) who presented at the Dermatology Department of Babol Hospital in 2023. A power analysis, conducted using G*Power, determined the appropriate sample size. With an alpha level of 0.05 and a power of 0.80, the analysis indicated a required sample of 199 participants. To account for the number of study variables and anticipated attrition due to incomplete data, 220 individuals were initially recruited via convenience sampling. Following the removal of incomplete questionnaires, 206 were deemed suitable for analysis.
Inclusion criteria for the study included adolescents aged 14 - 18 years, a diagnosis of skin disease (acne, alopecia, vitiligo, psoriasis) confirmed by a dermatologist, and living with both parents. Exclusion criteria included failure to complete all questionnaire items. After obtaining consent and explaining the purpose of the study to the adolescents, the research questionnaires were distributed. Ethical approval was granted by the University Ethics Committee. All participants were assured of the confidentiality and anonymity of their data and were informed that results would be presented in aggregate form to protect individual privacy. Written informed consent was obtained from all parents/guardians on behalf of participants under 18 years old, and written assent was obtained from all adolescent participants.
3.1. Instruments
3.1.1. Teenagers’ Quality of Life Questionnaire
The Teenagers’ Quality of Life (T-QoL) Questionnaire, developed by Alonso-Naranjo et al. (25), was used to assess quality of life. This 18-item questionnaire includes three subscales: Self-image, physical health and future aspirations, and psychological impact and relationships. Each item is rated on a 5-point Likert Scale (1: Never; 5: Always). A total score for the T-QoL is calculated by summing the scores of all 18 items. Higher scores indicate a higher quality of life. In this study, Cronbach’s alpha for the total scale, the physical health and future aspirations factor, the self-image factor, and the psychological impact and relationships factor were 0.95, 0.87, 0.95, and 0.92, respectively, indicating strong internal consistency reliability for the current sample.
3.1.2. Perceived Stress Questionnaire
The Perceived Stress Questionnaire (PSQ) is a 14-item self-report measure designed to assess participants’ perceived stress in various life domains. Participants respond on a 5-point Likert Scale (0: Never; 4: Very often), with higher scores indicating greater perceived stress. Items 4, 5, 6, 7, 8, 9, 10, and 13 are reverse-scored to account for positive phrasing (26). The PSQ exhibits acceptable internal consistency, with a reported Cronbach’s alpha coefficient of 0.72 (27).
3.1.3. Parent-Child Relationship Questionnaire
This instrument is used to assess the perception and open communication within family relationships between parents and children. It was developed by Fine et al. (28). This 24-item scale is based on a 7-point Likert Scale. The minimum possible score is 24 and the maximum is 168, with higher scores indicating a stronger parent-child relationship. In Alikhani et al.’s (29) study, Cronbach’s alpha for the questionnaire was reported as 0.92. In the present study, Cronbach’s alpha for the Parent-Child Relationship Questionnaire was 0.86.
3.2. Data Analysis
SPSS-27 software was used to analyze the data collected from this study. At the descriptive level, mean and standard deviation were used, and at the inferential level, Pearson correlation coefficient and stepwise regression were employed to examine the prediction of adolescents’ quality of life based on perceived stress and the parent-child relationship.
4. Results
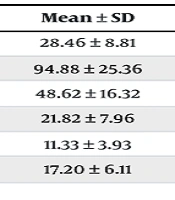
Findings related to demographic variables revealed that the mean age of adolescents was 16.25 ± 4.2 years, with a range of 14 to 18 years. Of the adolescents, 106 (51.46%) were female and 100 (48.54%) were male. The means, standard deviations, skewness, and kurtosis of the study variables are presented in Table 1. The skewness and kurtosis values for all variables were within acceptable ranges (± 1.5), indicating that the data were approximately normally distributed.
| Variables | Mean ± SD | Skewness | Kurtosis |
|---|---|---|---|
| Perceived stress | 28.46 ± 8.81 | 0.20 | 0.40 |
| Parent-child relationship | 94.88 ± 25.36 | 0.04 | -0.63 |
| Quality of life (total) | 48.62 ± 16.32 | 0.24 | 0.60 |
| Self-image | 21.82 ± 7.96 | -0.04 | 0.35 |
| Physical health and future aspirations | 11.33 ± 3.93 | -0.26 | 1.15 |
| Psychological impact and relationships | 17.20 ± 6.11 | -0.32 | 1.27 |
Descriptive Statistics of Study Variables
Table 2 presents the correlation coefficients among the study variables. Perceived stress exhibited a significant negative correlation with quality of life (r = -0.38), indicating a moderate inverse relationship wherein higher levels of perceived stress are associated with lower quality of life. Conversely, a significant positive correlation was observed between the parent-child relationship and quality of life (r = 0.60), suggesting a strong positive relationship wherein more positive parent-child relationships are associated with higher quality of life. To examine which variable had a more significant role in predicting quality of life, a stepwise regression analysis was conducted, with perceived stress and parent-child relationship as predictor variables and quality of life as the criterion variable. The results are presented in Table 3.
| Variables | Quality of life | |
|---|---|---|
| r | P | |
| Perceived stress | -0.38 | 0.001 |
| Parent-child relationship | 0.60 | 0.001 |
Pearson Correlation Coefficients Among the Research Variables
| Models | Predictor Variables | F | R | R2 | B | SE | β | t | P |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Parent-child relationship | 236.10 | 0.61 | 0.36 | 0.35 | 0.03 | 0.55 | 12.24 | 0.001 |
| 2 | Parent-child relationship and perceived stress | 124.32 | 0.62 | 0.38 | -0.24 | 0.08 | -0.13 | -2.88 | 0.001 |
Results of Simultaneous Regression Analysis
Table 3 presents the results of the regression analysis. In Model 1, the parent-child relationship significantly predicted quality of life (β = 0.55, P < 0.001). For every one-unit increase in the parent-child relationship score, quality of life is predicted to increase by 0.35 units, holding perceived stress constant. The parent-child relationship explained 36% of the variance in quality of life scores (R2 = 0.36). In Model 2, after controlling for the parent-child relationship, perceived stress significantly predicted quality of life (β = -0.13, P < 0.001). For every one-unit increase in perceived stress, quality of life is predicted to decrease by 0.24 units, holding the parent-child relationship constant. The addition of perceived stress to the model explained an additional 2% of the variance in quality of life (R2 change = 0.02, P < 0.001), with the overall model explaining 38% of the variance (R2 = 0.38).
5. Discussion
This study sought to elucidate the influence of perceived stress and parent-child relationships on the quality of life of adolescents afflicted with skin diseases. The primary finding of this study indicated a significant negative correlation between perceived stress and quality of life among adolescents with skin diseases. This finding is consistent with the results of previous studies by Homayuni (30) and Salari et al. (31). Perceived stress, a psychological factor, can significantly impact an individual’s quality of life, especially in adolescents struggling with skin diseases. Skin diseases, due to their direct impact on appearance, can lead to decreased self-esteem, increased anxiety, and social concerns in adolescents. Moreover, the perceived stress arising from these diseases can increase psychological pressure and reduce the ability to cope with daily challenges (16).
For example, Lazarus and Folkman’s transactional model of stress (32) posits that stress arises from an individual’s appraisal of a stressor and their coping resources. In the context of skin disease, adolescents may appraise their condition as highly threatening to their self-image and social standing, leading to increased stress. Additionally, Beck’s cognitive theory of depression (33) suggests that negative automatic thoughts and maladaptive beliefs about oneself and the future can contribute to both perceived stress and decreased quality of life. Therefore, it is hypothesized that the higher the level of perceived stress in adolescents with skin diseases, the lower their quality of life (31).
In general, skin diseases, particularly during adolescence — a sensitive period for identity development and socialization — can have significant psychological and social impacts. Adolescents with skin conditions may experience feelings of shame, embarrassment, or concern about social acceptance due to their appearance. These feelings can lead to considerable stress, which in turn affects their quality of life. Perceived stress refers to the psychological pressure experienced by individuals in various life situations, which they perceive as a threat to their well-being. This stress can negatively impact an adolescent’s ability to cope with daily challenges, such as academics, friendships, and social activities (34). Especially in adolescents struggling with skin diseases, perceived stress can reduce their motivation and energy to engage in everyday activities.
Another finding of the present study was that the parent-child relationship was significantly and positively correlated with the quality of life of adolescents with skin diseases. While a directly congruent study was not found in the available literature, this finding aligns with research highlighting the importance of family dynamics in adolescent well-being (29). This finding may be explained as follows: The parent-child relationship is an important environmental factor influencing the mental health and quality of life of adolescents. For adolescents facing the challenges of skin diseases, a positive and supportive relationship with parents may serve as a significant resource for coping with stress and psychological difficulties. Parental support may be associated with enhanced feelings of security, self-esteem, and acceptance in adolescents, which, in turn, may be related to improved quality of life (19). Positive parent-child interactions may influence adolescents’ perspectives on their disease and their coping strategies.
A positive and supportive parent-child relationship may be associated with reduced feelings of shame and isolation in adolescents, potentially contributing to improved quality of life. Conversely, a strained parent-child relationship may be related to increased feelings of insecurity, anxiety, and low self-esteem, which could negatively impact the well-being of adolescents with skin diseases. Adolescents reporting less positive parent-child relationships may also report receiving less emotional and psychological support for coping with their condition. Effective parent-child communication may help adolescents develop greater self-confidence in social situations, potentially reducing social anxiety related to skin conditions. This positive connection may encourage adolescents to engage in more social opportunities, which, in turn, may be associated with a higher quality of life. These findings suggest that interventions focused on fostering positive parent-child relationships may be a valuable strategy for improving the quality of life of adolescents with skin diseases and warrant further research and development of practical applications.
Among the limitations of this study, it can be stated that cultural and social differences can influence the nature of parent-child relationships and the level of perceived stress, which may limit the generalizability of the research findings. The presence of variables such as pre-existing psychological problems, socioeconomic status, and access to support resources can affect the results, and these variables may not be controllable. It may be difficult to obtain adequate samples of adolescents with skin diseases who have specific characteristics (such as disease severity or type of parental relationship), which can limit the generalizability of the results.
Despite these limitations, this study has several strengths. It contributes to the limited body of research examining the interplay of perceived stress, parent-child relationships, and quality of life in adolescents with skin diseases. The use of validated instruments enhances the reliability of the findings. Further, the focus on a specific age group (adolescents) allows for a more targeted understanding of the challenges faced by this population.
5.1. Conclusions
This study highlights the significant influence of perceived stress and parent-child relationships on the quality of life experienced by adolescents with skin diseases. Higher perceived stress correlated with diminished quality of life, underscoring the detrimental effects of psychological distress. Conversely, stronger parent-child relationships were associated with improved outcomes, emphasizing the protective role of family support. These findings suggest that effective management of skin diseases in adolescents necessitates addressing both psychological and social factors. Future research should investigate the underlying mechanisms of these relationships and develop targeted interventions to mitigate stress and strengthen family bonds, ultimately promoting well-being in this vulnerable population.