1. Background
The Herpesviridae family of DNA viruses is widely recognized for causing infections in individuals with both normal and compromised immune systems. Among the Herpesviridae family, eight virus types primarily infect humans, collectively referred to as human herpesviruses (HHV1–8) (1). Herpesvirus infections are prevalent worldwide, with varying rates of primary infection influenced by factors such as race, ethnicity, and geographic location. These viruses primarily affect children and are commonly transmitted through close contact. While primary infections may or may not present symptoms, all individuals become lifelong carriers following the initial infection (2, 3).
Five out of the eight virus types are commonly found in humans, including Herpes simplex viruses (HSV-1&2), Varicella zoster virus (VZV), Epstein–Barr virus (EBV), and cytomegalovirus (CMV) (4). The HSV-1&2 are responsible for oral and genital herpes, respectively, characterized by the appearance of typical lesions. The EBV causes infectious mononucleosis, while VZV is associated with chickenpox and shingles. Congenital CMV infection poses a significant risk to the developing fetus (5, 6). Several HHVs have been implicated in the development of cancer, notably EBV, which significantly increases the risk of lymphoma and carcinoma in the nasopharyngeal region (7).
In addition to the well-documented symptoms of primary infections and reactivations, several HHVs have been linked to chronic neurological disorders. Herpes simplex virus types 1, in particular, has been associated with Alzheimer’s disease, while EBV has been linked to multiple sclerosis (8, 9). Epidemiological factors, including geography, socioeconomic status, and age, impact the rate of HHV infection acquisition. Furthermore, host factors such as comorbidities, coinfections, and immunosuppression influence the acquisition, reactivation, and severity of symptoms (10).
Given that the majority of herpesvirus infections are not documented in medical records, the detection of anti-HHV immunoglobulin G (IgG) antibodies is currently the gold standard for screening a history of HHV infection. An individual may test positive for anti-HHV IgG (indicating carrier status) or negative (indicating non-carrier status). The proportion of positive individuals in a population is expressed as seroprevalence (6). Accurate estimates of seroprevalence are essential for driving vaccine development and guiding decisions regarding screening programs and treatment recommendations for a population.
This research aimed to determine the prevalence of serum IgG and M antibodies against HSV-1&2, EBV, VZV, and CMV in the population of Ahvaz. A thorough understanding of the seroepidemiology of HSV-1&2, EBV, VZV, and CMV in Ahvaz is crucial for developing effective strategies for infection prevention and control.
2. Objectives
Considering the importance of understanding the epidemiology of these infections during childhood and the significant impact of maternal seroprevalence on the epidemiology of these infections in children, we decided to investigate the seroprevalence of CMV, EBV, HSV, and VZV viruses among children and adults in the city of Ahvaz over an 11-year period.
3. Methods
3.1. Inclusion and Exclusion Criteria
All individuals who requested testing and did not have any specific disease were included in the study, while individuals whose age was unknown and pregnant women were excluded from the study.
The current study employed a cross-sectional descriptive-analytical approach, analyzing the laboratory records of 14,126 patients referred to the Matourian private laboratory in Ahvaz City between 2011 and 2023. A sampling method was used, relying on readily accessible and user-friendly files. The data collection process utilized test software developed by the company "Linking Medicine and Software." Data were collected through a census using a self-constructed checklist, which included variables such as the seroprevalence of CMV, EBV, HSV, and VZV viruses, age (categorized into groups), and the gender of the patients. The study included individuals from various cities in Khuzestan, with the majority residing in Ahvaz. The exclusion criteria encompassed individuals with incomplete information and pregnant women.
Data analysis was conducted using STATA version 12 for Windows. Mean and standard deviation were applied to analyze quantitative variables, while frequency percentages were calculated for qualitative variables, such as age and gender. The relationship between the primary variable (serum prevalence) and dependent variables was assessed using the chi-square test, with a significance level set at less than 0.05%.
This cross-sectional study was based on laboratory data from archived patient files and was conducted under the research project code OG-0214. The study was approved by the ethics committee and adhered to the ethics code (IR.AJUMS.REC.1402.336).
4. Results
The current study analyzed 14,126 serum samples from individuals aged 1 to 88 years, with a mean age of 30.61 ± 17.01 years. The samples were tested for the presence of CMV, HSV-1&2, EBV, and VZV using ELISA. Participants were categorized into diverse age groups: 2,421 individuals (17.1% of the total sample) were aged 1 - 10 years, 1,342 (9.5%) were aged 11 - 20 years, and 3,130 (22.2%) were aged 21 - 30 years. Additional age groups included 3,551 individuals (25.1%) aged 31 - 40 years, 1,777 (12.6%) aged 41 - 50 years, and 1,905 (13.5%) aged over 50 years.
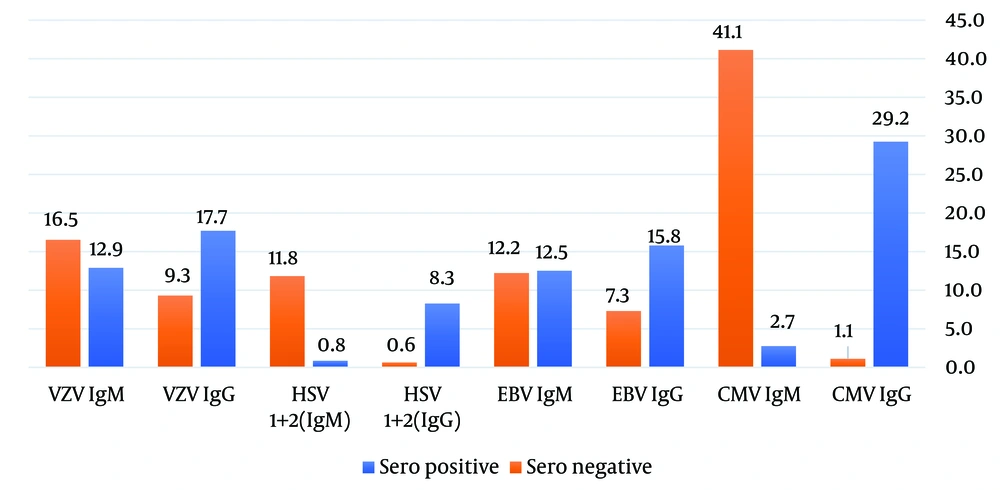
Among the participants, 7,844 (55.5%) were female, and 6,282 (44.5%) were male. Positive laboratory results were observed in 8,490 individuals (60.1%), while 5,636 (39.9%) tested negative. As shown in Figure 1, the highest seroprevalence among positive cases was for CMV (IgG) (29.2%), while the lowest was for HSV-1&2 (IgM) (0.8%).
The study findings indicated that the age group with the highest seroprevalence among participants with positive results was 31 - 40 years, while the group with the lowest seroprevalence was 11 - 20 years. Data in Table 1 show that the 31 - 40 age group had the highest seroprevalence for EBV (IgM) and the lowest for HSV-1&2 (IgM). Conversely, the 11 - 20 age group displayed the highest seroprevalence for EBV (IgG) and the lowest for HSV-1&2 (IgM).
| Age Group (y) | F (%) | CMV IgG | CMV IgM | EBV (IgG) | EBV (IgM) | HSV-1&2 (IgG) | HSV-1&2 (IgM) | VZV IgG | VZV IgM | P-Value b |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 - 10 | 1335 (15.7) | 333 (3.9) | 59 (0.7) | 329 (3.9) | 385 (4.5) | 73 (0.9) | 8 (0.1) | 53 (0.6) | 95 (1.1) | 0.001 |
| 11 - 20 | 795 (9.4) | 179 (2.1) | 25 (0.3) | 184 (2.2) | 137 (1.6) | 67 (0.8) | 8 (0.1) | 100 (1.2) | 95 (1.1) | 0.0001 |
| 21 - 30 | 1898 (22.4) | 659 (7.8) | 51 (0.6) | 223 (2.6) | 193 (2.3) | 165 (1.9) | 20 (0.2) | 320 (3.8) | 267 (3.1) | 0.001 |
| 31 - 40 | 2214 (26.1) | 827 (9.7) | 60 (0.7) | 222 (2.6) | 144 (1.7) | 159 (1.9) | 20 (0.2) | 463 (5.5) | 319 (3.8) | 0.01 |
| 41 - 50 | 1080 (12.7) | 268 (3.2) | 15 (0.2) | 159 (1.9) | 90 (1.1) | 103 (1.2) | 8 (0.1) | 286 (3.4) | 151 (1.8) | 0.001 |
| > 51 | 1168 (13.8) | 217 (2.6) | 23 (0.3) | 223 (2.6) | 113 (1.3) | 136 (1.6) | 8 (0.1) | 280 (3.3) | 168 (2.0) | 0.001 |
| Total | 8490 (100) | 2483 (29.2) | 233 (2.7) | 1340 (15.8) | 1062 (12.5) | 703 (8.3) | 72 (0.8) | 1502 (17.7) | 1095 (12.9) | - |
The Frequency of Seroprevalence Based on Positive Laboratory Results for Each Age Group is Presented (N = 8490) a
For the 21 - 30 age group, CMV IgG had the highest seroprevalence, while HSV-1&2 (IgM) exhibited the lowest. Among individuals aged 41 - 50 years, CMV IgG demonstrated the highest seroprevalence, and HSV-1&2 (IgM) the lowest. In the + 51 age group, VZV IgG had the highest seroprevalence, with HSV-1&2 (IgM) again showing the lowest.
These findings are summarized in Table 1. The Pearson test results revealed a statistically significant difference between age groups and the prevalence of serum test results among individuals with positive outcomes (P < 0.05). For further details, refer to Table 1.
The results showed that among participants with positive results, the highest seroprevalence was 56.3% in females, while the lowest was 43.7% in males. As detailed in Table 2, CMV IgG had the highest seroprevalence, and HSV-1&2 (IgM) had the lowest seroprevalence in both males and females with positive test results. Additionally, a statistically significant difference was observed in the seroprevalence of the examined virus types based on gender (P < 0.05).
| Variable | F (%) | CMV IgG | CMV IgM | EBV IgG | EBV IgM | HSV-1&2 (IgG) | HSV-1&2 (IgM) | VZV IgG | VZV IgM | P-Value b |
|---|---|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||||
| Male | 3709 (43.7) | 1043 (12.3) | 78 (0.9) | 538 (6.3) | 432 (5.1) | 352 (4.1) | 27 (0.3) | 744 (8.8) | 495 (5.8) | 0.0001 |
| Female | 4781 (56.3) | 1440 (17.0) | 155 (1.8) | 802 (9.4) | 630 (7.4) | 351 (4.1) | 45 (0.5) | 758 (8.9) | 600 (7.1) | 0.001 |
| Total | 8490 (100) | 2483 (29.2) | 233 (2.7) | 1340 (15.8) | 1062 (12.5) | 703 (8.3) | 72 (0.8) | 1502 (17.7) | 1095 (12.9) | - |
The Frequency of Seroprevalence Based on Positive Laboratory Results and Gender is Presented Here (N = 8490) a
5. Discussion
The discussion provides an overview of the two primary methods used for diagnosing VZV, HSV, EBV, and CMV infections: Molecular and serological techniques. Numerous seroepidemiological studies have been conducted across various populations and regions worldwide, including our country, revealing a high prevalence of these infections.
5.1. Herpes Simplex Virus 1&2
In ten developed countries, including the United States of America, Canada, Japan, Germany, England, Belgium, France, Italy, Spain, and Australia, more than 107 million individuals have tested positive for HSV-2 IgM. In Iran, the spread of this virus is relatively low, possibly due to family health practices and cultural factors. Arabzadeh et al. examined 966 patients referred to the blood transfusion organization, finding that 49% were HSV-1 IgG positive, while 2.7% were HSV-2 IgG positive. The prevalence of HSV-2 IgG positivity significantly increased with age (11). Parvaie et al. conducted a study on 100 students in Birjand, reporting that 41% tested positive for HSV-1 IgG (12). Similarly, Kasraian and Movasseghi investigated 835 women in Shiraz, revealing a 93.78% prevalence of HSV IgG-positive individuals (13). Table 1 presents the frequency of seropositive individuals across different age groups in this study.
5.2. Epstein-Barr Virus
In a report by Taherkhani et al. conducted in Bushehr on patients with multiple sclerosis, 95.2% tested positive for IgG VCA EBV (14). A study by Soleimani et al. on 245 children in Zahedan tested for VCA-IgG EBV revealed that 81.2% had a positive titer, while 11% had a negative titer. No significant difference in antibody titers was observed between males and females. The research demonstrated that the anti-EBV antibody titer increases with age (15). The findings indicated an overall prevalence of EBV infection in children of 81.2%, with higher rates in older age groups and those from larger families, likely due to increased exposure to the virus through social contacts. Compared to similar studies, the higher prevalence of infection in Zahedan may be attributed to larger household sizes and a lower level of healthcare in the area (15).
In a study by Rostamzadeh et al. on 68 kidney transplant recipients, 58 patients (85.3%) tested positive for IgG EBV, while 10 patients (14.7%) tested positive for IgM EBV (16). Table 1 presents the frequency of seropositive individuals across different age groups in this study.
5.3. Cytomegalovirus
In a report by Falahi et al., the percentages of CMV IgG and CMV IgM in women with spontaneous gonorrhea were 14.28% and 28.58%, respectively (17). In a study conducted by Mohammadi et al. on 178 medical students in Babol, the percentage of CMV IgG positivity was 96% (18). A case-control study conducted by Ebadi et al. examined 120 pregnant women with recurrent miscarriages and 120 pregnant women with normal deliveries as a control group. The CMV IgG was positive in 94 patients (78.3%) from the miscarriage group and 75 patients (62.5%) from the control group (19). Omidifar et al. conducted a study on 2,469 individuals and found that CMV IgM was positive in 18 patients (0.73%) and CMV IgG was positive in 1,139 patients (46%) (20).
Tayebi et al. demonstrated that 94.4% of participants tested positive for CMV IgG, a finding that was similar to or different from our study (21). In the study by Motamedifar et al., conducted on 360 blood donors in Shiraz in 2009, 98.9% tested positive for CMV IgG and 4.4% for CMV IgM (22). This research found no significant relationship between gender, age, and the prevalence of serum antibodies against CMV. The findings align with our study regarding prevalence but differ concerning the relationship with age and sex. Khudir and Molan found that among 186 male and female students aged 18 to 23 years, 181 (97.4%) tested positive for CMV IgG, consistent with our results (21-23). Hejazi et al. conducted a study on 180 healthy blood donors and found that 5 (2.8%) had IgM antibodies against CMV (24). Table 1 presents the frequency of seropositive individuals in different age groups in this study.
The high prevalence of IgG anti-CMV antibodies in our study suggests a widespread and significant prevalence of CMV infection in society. Given this high prevalence and the importance of congenital diseases caused by CMV, it is essential to expand prevention programs and provide targeted training, particularly for seronegative healthcare personnel (e.g., doctors, nurses, and midwives) and seronegative women of reproductive age.
5.4. Varicella Zoster Virus
In Iran, immunity levels to VZV range from 71.4% to 78.5% in the general population (25) and from 86.5% to 86.9% among women of reproductive age (26). In one study, 26% of women tested positive for VZV, while 57.8% tested positive for VZV IgG, which accounted for 83.8% of the study population (27). Table 1 illustrates the frequency of seropositive individuals across different age groups. In this study, 99.4% of participants were found to be non-immune or sensitive to the VZV virus (IgG VZV-negative population), placing them at clinical risk for chickenpox and its potentially severe complications. Consequently, it is recommended that these individuals be identified and vaccinated, if possible. This contrasts with the significantly lower percentage of non-immune individuals among Turkish students (2.2%) (28, 29).
Maghbooli et al. reported a VZV IgG prevalence rate of 95.5% among stroke patients (30). Similarly, a study on healthcare workers in Kermanshah found a VZV IgG prevalence rate of 84.5% (31). In India, the VZV IgG rate was found to be 70% (32). Conversely, a study conducted in the Philippines revealed that 50% to 60% of individuals with sufficient antibody levels were in the age group of 16 to 20 years (33). Additionally, a study in Spain demonstrated that 80% of children produce sufficient levels of IgG antibodies by the age of seven years (34). Jafari-Shakib et al. reported that out of 101 students studied, 72.3% tested positive for VZV IgG, while 26.7% tested negative (35).
Our study yielded results consistent with most of the aforementioned studies in terms of prevalence rates and the relationships with age and sex. However, a small number of studies in Iran and other countries occasionally report lower or, in some cases, higher prevalence rates. Variations in results among different studies suggest a relationship between the prevalence of infection and factors such as age, gender, geographic and climatic location, and the quality of healthcare available in different regions.
5.5. Conclusions
The high seroprevalence of CMV and VZV in this population underscores the need for targeted vaccination programs, particularly for at-risk groups such as women of childbearing age and healthcare workers. The prioritization of developing and implementing CMV vaccines, which are currently not widely available, is well-justified given their significant seroprevalence and impact on the health of both mothers and fetuses. Furthermore, longitudinal studies are crucial to monitor the progression of herpesvirus infections over time, especially in light of changing social behaviors, vaccination efforts, and advancements in healthcare infrastructure.
This study provides a robust foundation for ongoing surveillance efforts. Health education campaigns emphasizing hygiene practices, particularly in communities with higher transmission rates, may help reduce the seroprevalence of viruses such as herpes simplex virus type 1 (HSV-1) and EBV. Additionally, public health messaging should include education on the risks associated with herpesvirus reactivation and its implications for chronic diseases.