1. Background
Continuous professional education is crucial for healthcare professionals to maintain competency (1) and keep up-to-date with advancements in technology, diseases, treatments, and evidence-based practices, including patient safety (2). The main emphasis is on improving clinical skills through healthcare education, equipping practitioners to devise effective treatments, and providing high-quality patient care with medical sciences, physiology, and pharmacology knowledge. Additionally, promoting patient safety is a vital concern (3). Patient safety and healthcare quality present challenges across all medical fields, including transfusion medicine. Enhancing the knowledge of healthcare experts and technicians can significantly improve patient safety (4). Today's health workforce must maintain professional competency by completing a minimum number of continuing education hours annually (5). Healthcare professionals in rural and remote clinical settings also need similar opportunities for continuing professional development (6). Recent technological advancements have turned traditional learning into essential virtual and electronic formats (7), particularly benefiting this group. Virtual education improves learning through adaptability, interactivity, reduced training costs, and round-the-clock access (8). E-learning includes several formats: Face-to-face (physical presence without electronic communication), self-paced (independent learning without communication), asynchronous (electronic communication without presence), synchronous (virtual presence with communication), hybrid/mixed asynchronous (case presence), and hybrid/mixed synchronous (presence with communication). These taxonomies enable researchers to evaluate the effectiveness of each format and its impact on the student learning experience (9). Although most research on e-learning for healthcare professionals has focused on participant satisfaction and knowledge acquisition (8). On the other hand, blood transfusions are essential for patients suffering from hemorrhage and impact numerous individuals globally. Healthcare professionals have a fundamental responsibility to care for these patients (2). While transfusions are essential, they carry risks due to potential side effects and human error. Training healthcare workers can significantly mitigate these risks (3). Improving staff knowledge is crucial for ensuring patient safety and providing high-quality care. Therefore, proper training is essential for safeguarding patient health in this field (10). Additionally, patient blood management (PBM) is recognized worldwide as a standard practice to ensure the safety and quality of blood transfusions (11).
2. Objectives
For PBM implementation in the third referral hospital, training programs were conducted for physicians, laboratory personnel, and nurses to: (1) Investigate the effect of this training on their knowledge, and (2) sustain learning. Thus, we conducted a study to evaluate training retention in blood transfusion practices after six months and one year.
3. Methods
This cross-sectional study was conducted at Shahid Lavasani Hospital, a 160-bed tertiary facility in Tehran, Iran, from November 2016 to November 2017. The study aimed to train staff on PBM principles and evaluate long-term knowledge retention. Participants were randomly selected from departments involved in blood transfusion and included nurses, laboratory personnel, and physicians. The sample size was determined based on feasibility and the availability of personnel in the hospital. A sample of 243 participants was selected to ensure adequate statistical power for detecting differences after the intervention. This sample size was chosen based on the number of hospital staff available for training within the study period and was considered sufficient to detect meaningful changes in knowledge retention over time.
3.1. Inclusion and Exclusion Criteria
3.1.1. Inclusion Criteria
Staff with over one year of experience in blood product transfusion who volunteered and provided informed consent.
3.1.2. Exclusion Criteria
Staff unwilling to participate.
3.2. Conducting the Study
Before training, participants completed a knowledge assessment test. Subsequently, all enrolled staff attended a six-hour virtual seminar on PBM principles, blood product alternatives, and restrictive transfusion practices. The seminar was led by an anesthesiologist with 20 years of experience in transfusion medicine. The training course employed active learning techniques, including question and answer sessions, one-minute essays, and think-pair-share discussions, and was conducted synchronously online (virtual presence with communication).
The Think-Pair-Share method involves all participants by having the instructor pose an open-ended question, allowing a minute for reflection and responses. A one-minute essay is used in class as a formative assessment. At the end of class or just before recess, participants are asked, “What were the two most important points from today’s session?” or “What was the muddiest (least clear) point from today’s session?” Participants are given 1 - 2 minutes to write brief responses to answer anonymously as they leave the class. Their responses are reviewed in the next session.
After the training course, participants took an exam on the material, and knowledge retention was evaluated using the same exam six months and one year later. The final exam, designed and reviewed by experienced scientists, included five sections of 25 multiple-choice questions on PBM, awarding one point for each correct answer and imposing no penalties for incorrect ones.
3.3. Data Analyses
We employed random sampling to mitigate selection bias. Descriptive statistics, including mean, standard deviation, frequency, and percentages, were used to summarize the data. We examined the relationships between final exam scores, participants' education levels, their departments, and years of work experience. The number and percentage of correct answers for each question were also reported, with scores expressed as mean ± standard deviation. We utilized one-way ANOVA, chi-square tests, and paired t-tests for comparisons, analyzing the data using SPSS version 23. A P-value of less than 0.05 was considered statistically significant.
4. Results
In 2016, a total of 243 staff members were randomly selected to participate in the study during the first educational seminar. The participants included 12 lab technicians (4.9%), 229 nurses (94.3%), and 2 physicians (0.8%). Among the participants, 64.2% were women and 35.8% were men. The results of the staff exams were analyzed based on their total years of education, which ranged from a minimum of 12 years to a maximum of 19 years, with a mean of 15.38 ± 1.4 years. Additionally, participants had job experiences ranging from 1 year to a maximum of 25 years, with a median experience of 8.9 ± 5.6 years. The statistical analysis showed a significant result (P = 0.03, 95% CI: 0.5051 to 12.2949). Moreover, the mean and standard deviation of the first exam scores are detailed in Table 1. The difference in mean scores was found to be significant (P < 0.0001, 95% CI: 12.4414 to 21.3986). Participants were categorized into three groups based on their years of work experience: Group A (1 to 5 years), group B (6 to 15 years), and group C (more than 16 years). The final scores for each group, according to their work experience, are displayed in Table 2. However, no significant relationship was found between job experience and exam scores (P = 0.07, 95% CI: -0.46 to 9.46).
| Education (y) | Values | Score in the First Test After Training |
|---|---|---|
| 12 | 28 (11.5) | 87.43 ± 10.25 |
| 14 | 30 (12.4) | 97.47 ± 7.38 |
| 16 | 176 (72.4) | 90.69 ± 10.77 |
| 18 | 7 (2.9) | 88.57 ± 10.93 |
| 19 | 2 (0.8) | 98.00 ± 2.82 |
| Total | 243 (100) | 91.15 ± 10.60 |
Total Scores of Participants Based on Education Years a
| Job Experience (y) | Values | Score in the First Test After Training |
|---|---|---|
| Group A (1 - 5) | 18 (7.4) | 88.86 ± 11.43 |
| Group B (6 - 15) | 74 (30.4) | 92.09 ± 10.24 |
| Group C (> 16) | 151 (62.2) | 93.33 ± 9.89 |
| Total | 243 | 91.15 ± 10.60 |
The Relationship Between Job Experience and Scoring of Participants at the First Training a
4.1. After Six Months
Six months later, we invited the participants to take the same test in a virtual environment, but only 35 took the test. Table 3 shows the occupation section and their scores. All participants were nurses with work experience ranging from 1 to 20 years (average 9.8 ± 5.7 years). After six months, the mean score was 81.09 ± 10.31 (minimum 52 and maximum 100), showing no significant differences between groups (P = 0.09, 95% CI: 1.19 to 13.51) as shown in Table 3. Participants' scores based on job experience showed no significant difference (P = 0.1, 95% CI: -2.72 to 18.92) after six months, as presented in Table 4.
| Ward of Participants | Participants | Score in the Second Test Six Months After Training |
|---|---|---|
| Emergency room | 3 (8.6) | 78.0 ± 23.5 |
| Intensive care units | 11 (31.4) | 77.4 ± 10.4 |
| Operating room | 3 (8.6) | 82.6 ± 2.3 |
| General ward | 18 (51.4) | 83.56 ± 8.07 |
| Total | 35 (100) | 78.0 ± 23.5 |
The Mean Score of the Participants After Six Months Based on the Department Where They Work a
| Job Experience (y) | Values | Score in the Second Test (Six Months Later) |
|---|---|---|
| Group A (1 - 5) | 9 (25.7) | 85.3 ± 11.7 |
| Group B (6 - 15) | 20 (57.2) | 77.9 ± 9.8 |
| Group C (> 16) | 6 (17.1) | 86.0 ± 7.6 |
| Total | 35 (100) | 81.09 ± 10.3 |
The Average Score of Participants Based on Work Experience in Years in Second Test a
4.2. After One Year
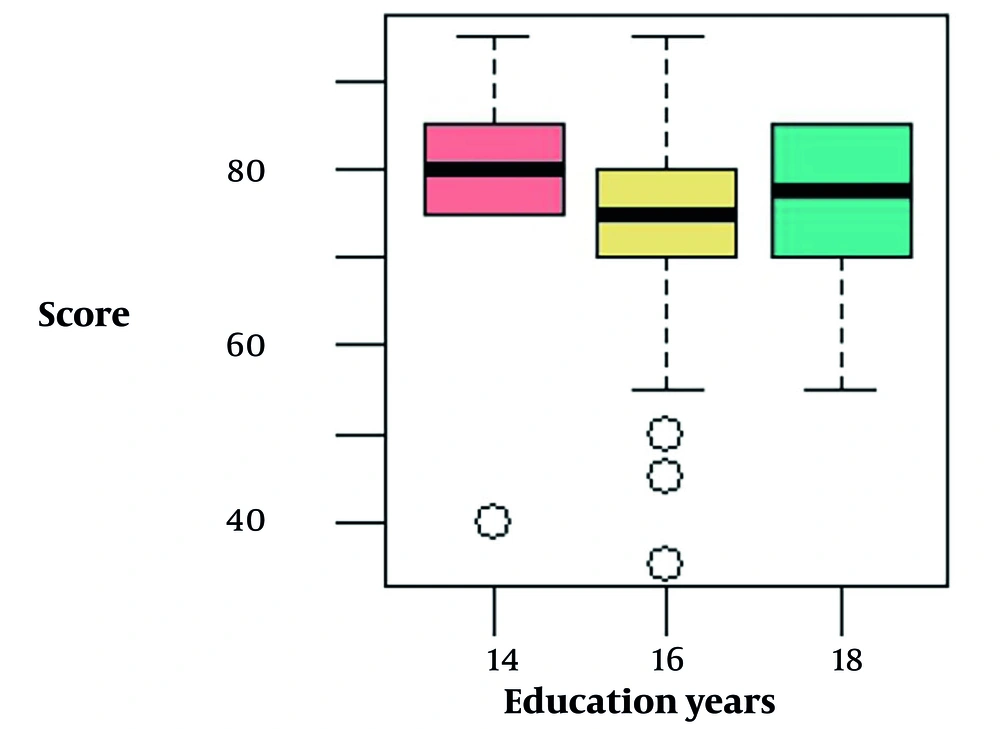
One year after the initial training, participants underwent the same tests to evaluate long-term memory. A total of 116 individuals agreed to participate in this test, with the following distribution among departments: 6 (5.2%) from the emergency department, 22 (19%) from the ICU, 20 (17.2%) from the lab, 1 (0.9%) from the operating room, and 67 (57.7%) from the general ward. The scores for employees in each department are presented in Table 5. The overall average score was 75.60 ± 10.28, with a minimum score of 35 and a maximum score of 95. The average years of education among the participants was 15.9 ± 0.7, ranging from 14 to 18 years. The distribution of exam scores among healthcare workers (HCWs) after one year showed a minimum score of 35 and a maximum score of 95. The median score was 75, with an interquartile range (IQR) of 70 to 80, indicating that 50% of the participants scored within this range. The mean score was 75.6 ± 10.28 (Table 5).
| Ward of Participants | Values | Score in the Third Test (One Year After Training) |
|---|---|---|
| Emergency room | 6 (5.2) | 75.8 ± 4.9 |
| Intensive care units | 22 (19) | 75.0 ± 9.5 |
| Lab | 20 (17.2) | 82.2 ± 7.6 |
| Operating room | 1 (0.9) | 75.0 ± 0 |
| General ward | 67 (57.7) | 73.8 ± 10.9 |
| Total | 116 (100) | 75.6 ± 10.2 |
The Average Score of Participants one Year After the First Training Based on Their Workplace a
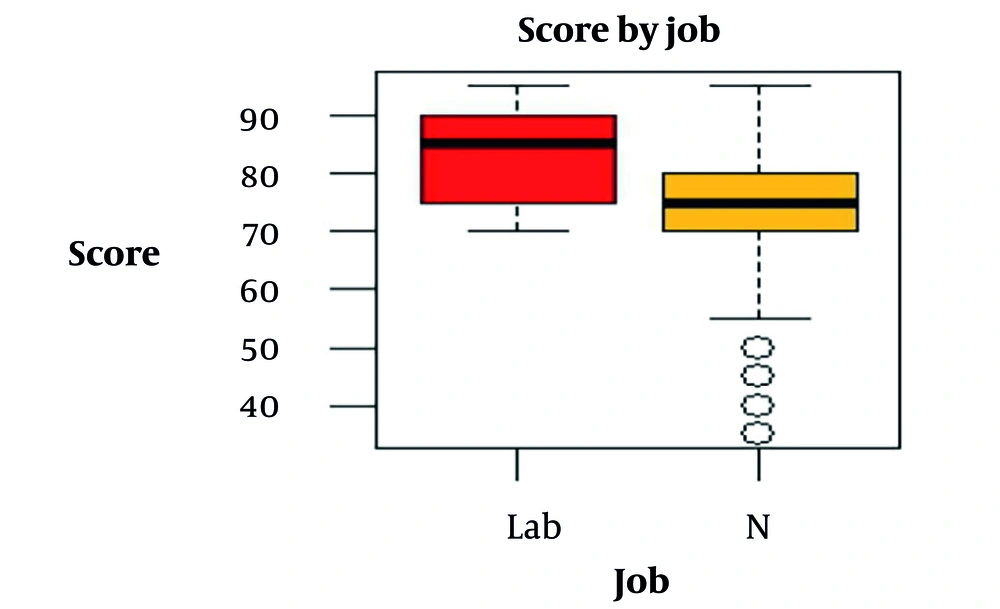
The analysis of exam scores among HCWs based on job type, education level, and hospital ward revealed notable differences in performance:
- Lab technicians consistently achieved higher mean scores across all education levels, with scores ranging from 80 to 83.3. Those with 14 years of education had the highest mean score (83.3 ± 8.16), while those with 18 years of education had a slightly lower mean score (80 ± 7.07).
- Nurses displayed greater variability in scores, particularly across different hospital wards.
- Nurses with 16 years of education working in the CCU had the highest recorded mean score (85 ± 7.7), while those in ward settings had a lower mean score (74.6 ± 10.4).
- Nurses with 18 years of education working in ward settings had the lowest mean score (70 ± 15).
- A nurse in the Angiography ward with 14 years of education had the lowest individual score.
These findings suggest that both job type and hospital ward may influence exam performance, with lab technicians generally outperforming nurses. Additionally, higher education levels did not consistently correspond to higher scores, indicating that other factors, such as clinical experience or ward-specific challenges, may impact performance. The results indicate that job type is a significant predictor of exam performance, with lab technicians achieving higher scores than nurses. However, education level does not appear to significantly impact exam scores. The relatively low R2 value suggests that additional factors, such as clinical experience, workload, or ward assignment, may play a critical role in determining exam performance after one year (Figures 1 and 2).
5. Discussion
To establish the PBM program, we began by training hospital personnel, including physicians, nurses, and laboratory staff. A total of 243 individuals participated in the initial training session. This group comprised 12 laboratory technicians, 229 nurses, and two physicians, with nurses accounting for over 94% of the participants. The average score on the first test was 91.5 ± 10.6. Scores based on job categories were as follows: Laboratory technicians scored 85 ± 10.2, nurses scored 91.4 ± 10.6, and physicians scored 98 ± 2.8. There were no significant correlations observed between job experience and participant scores.
Furthermore, we evaluated the long-term retention of training after one year among the same personnel. The data indicated a consistent decline in scores since the initial training, resulting in an average score of 75.6 ± 10.2. Exam performance differed by job type and ward; lab technicians outperformed nurses. Job type, but not education, was a significant predictor of exam scores. After one year, clinical experience, workload, and ward-specific challenges significantly influenced performance.
Inadequate blood transfusion practices can significantly increase patient morbidity and mortality (12). Piri et al. reported that 26.2% of healthcare workers have a low level of knowledge about blood transfusions, 22.1% have an average understanding, and only 51.6% achieve acceptable competency, underscoring the urgent need for comprehensive training (13). A descriptive study by Gouezec et al. assessed blood transfusion knowledge among staff at 14 public hospitals, revealing a troubling average score of 62%, with responses ranging from 14% to 89% (14). In contrast, our study yielded impressive results, with total mean scores of 91.5 ± 10.6 following the first PBM training, 81.09 ± 10.32 six months later, and 75.60 ± 10.28 after one year. These findings highlight the significant impact of targeted education in enhancing knowledge, which may lead to improved blood transfusion outcomes.
Talati et al. designed 20 questions on blood transfusion, with an average correct response rate of 60.7% (15). Meanwhile, Elhy found that over half of nurses lack adequate knowledge about it (16). Kumarage et al. designed a 45-question self-administered questionnaire in transfusion medicine, which 57 post-internship physicians completed. Participants scored lowest in interpreting laboratory results (19.8%) and highest in blood component administration (56.63%), with an average score of 41.45%. There was no significant statistical difference among various specialties (17). Bicer et al. assessed the nurses’ knowledge level concerning blood components transfusion, including erythrocytes, thrombocyte products, and their storage time, and their level of knowledge increased considerably after the training (18). However, a separate study on inpatient care highlighted that nurses had inadequate knowledge regarding bedside blood compatibility testing, pre-transfusion compatibility checks, red cell antibody screening, and transfusion-related adverse events (19).
In our study, despite the personnel having received previous education on blood products, our objective was to provide advanced training in PBM. Notably, the last five questions in our study were specifically about complications related to blood transfusions. In one study, Akyol found that participants’ mean scores increased during the post-training period, regardless of whether their length of service was less than 4 - 5 years or more. However, this increase was not statistically significant (20). In another study, Dubey et al. reported that staff with more experience working in inner-city blood centers and who received additional training had significantly higher levels of awareness (21). We observed no statistically significant difference in scores between experienced and less experienced employees. Likewise, Hijji et al. found no significant differences in nurses' mean knowledge scores on blood transfusion across hospital wards (22). However, our study demonstrated that job type and hospital ward appeared to influence exam performance, with lab technicians generally outperforming nurses after one year. Admittedly, other factors, like clinical experience, workload, or ward assignment, significantly contributed to exam performance after one year.
Casey et al. indicated that factors like pre-training and context affect learning, with motivation being a key pre-educational state that enhances knowledge retention, attitude change, and learning intent (23). Long-term memory mechanisms involve a dynamic interplay of encoding, consolidation, storage, and retrieval, influenced by neurobiological changes and neuronal plasticity. Effective training strategies can enhance these processes, resulting in improved retention and recall of information (24). Anderson showed that forgetting happens rapidly after initial learning (25). Ebbinghaus's forgetting curve reveals that material learned through traditional methods is typically forgotten within six weeks (26), unless consciously reviewed or applied, which can extend retention by weeks or even months (27). Given that the participants in our study achieved an average score of 75.6 ± 10.2 after one year, we can conclude that they applied scientific principles in their work.
Patient blood management emphasizes timely and appropriate blood transfusions and extends beyond just transfusion practices (28). Creating interdisciplinary systems for PBM is essential for reducing transfusion needs, particularly through early identification and treatment of anemia and its causes (20). Consequently, we trained personnel from various specialties on PBM, highlighting that active learning methods — such as Q&A sessions, one-minute essays, and think-pair-share discussions — can improve long-term memory retention.
5.1. Limitations
This study had several limitations: A small sample size due to participant drop-out at six and twelve months, a lack of diversity, and external factors potentially influencing learning retention. Additionally, we did not account for educational variables such as pre-training, attitude changes, and enthusiasm for learning.
5.2. Conclusions
The average score of the participants decreased over time, from 91.15 ± 10.60 to 75.60 ± 10.28 after one year. We observed that active learning methods and applying learning in practice might contribute to long-term memory and stability after virtual training.