1. Background
Obesity is a serious public health problem that has increased to the point of representing a worldwide epidemic such that in 2015, approximately 700 million people were considered obese (1). The use of weight loss dieting has been overemphasized as the first modality to treat obesity (2). A deficit of 500 to 1000 calories/day has been prescribed as an integral part of a weight-loss program aiming at achieving a safe rate of weight loss (3).
Self-efficacy is an integrative framework that has been proven useful in a variety of treatment contexts (4). In terms of weight loss, self-efficacy refers to a person’s belief in his/her ability to adhere to dietary recommendations (5). It has been reported that self-efficacy plays an important role in successful weight loss behaviors, weight loss, and maintenance (6-8). The persons with high efficacy expectations will engage in important behaviors related to losing weight and persist in the face of weight loss barriers (9). On the other hand, changes in eating self-efficacy have appeared to be an even stronger predictor during treatment than at baseline (4, 10, 11).
Nutrition education intervention is an instructional method of healthy eating promotion aiming at facilitating the voluntary adoption of nutrition-related behaviors beneficial to health (12). It has been reported that nutrition education is significantly associated with changes in the measures of self-efficacy (13, 14).
2. Objectives
The aim of the current study was to compare the effects of a balanced low-calorie diet with or without nutrition education in an individual format on eating self-efficacy and its subscales changes and weight loss in short (3 months) and medium term (6 months).
3. Methods
The target sample size of 60 subjects (30 in each group) was calculated for the study by considering type І error (α = 0.05), type ІІ error (β = 0.1), mean and standard deviation in a previous study (15) and using the formula of

Finally, given an anticipated dropout rate of 30%, enrollment target was set for 90 subjects. In this randomized clinical trial, ninety volunteer obese women were recruited from the nutrition clinic in Ardabil city. The participants were apparently healthy, non-pregnant, non-lactating, and non-menopausal obese women, aged 18 - 50 years, and body mass index ranged from 30 to 40 kg/m2. They had no participation in weight loss programs in the previous 6 months.
Written information, including the purpose of the study and confidentiality of personal information, was given to each participant. The written informed consent form was obtained from the subjects. The protocol of the study was approved by the ethics committee of Tabriz University of Medical Sciences and registered in the registration center for clinical trials in Iran with the registration code IRCT201110181197N12.
Participants’ weight, height, and waist circumference were measured using a balanced scale. The body mass index was calculated as weight (kg) divided by squared height (m2) of each participant. The anthropometric measurement was done at baseline, 3, and 6 months after the intervention.
Weight efficacy lifestyle questionnaire (WEL) (4) was employed to measure individuals’ perceptions of their ability to control their weight by resisting eating in various situations such as availability of food, negative emotions, physical discomfort, positive activities related to eating, and social pressure to eat. The participants were asked to rate their confidence to resist the desire to eat using a 10-point scale ranging from 0 (not confident) to 9 (very confident). Participants’ scores on each subscale were calculated by averaging scores within each subscale. The score of WEL was also computed as an overall index of self-efficacy. In this study, the validated Persian version of the questionnaire by Babai et al. was used (16). The WEL questionnaire was completed at baseline, 3, and 6 months after the intervention.
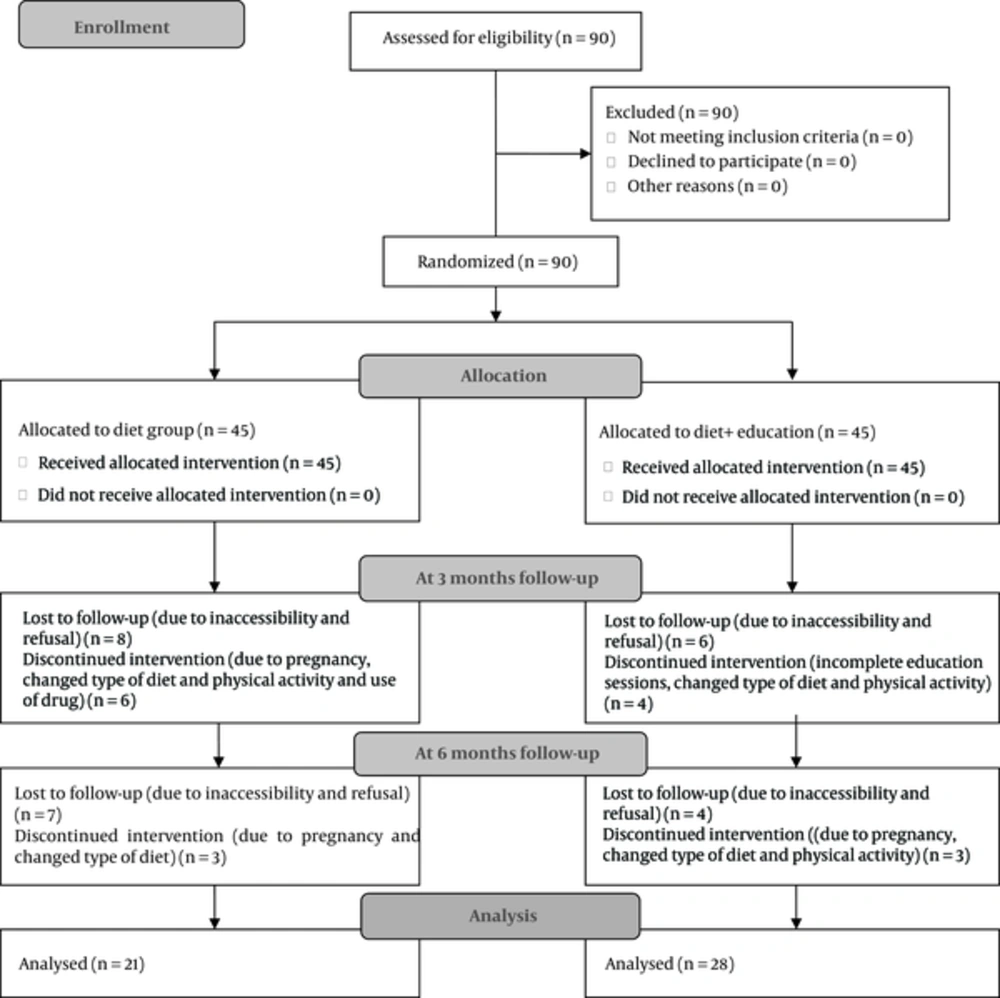
The participants were randomly assigned to receive a balanced low-calorie diet with or without education. Balanced low-calorie diet was an individualized diet with an energy deficit of 500 calories of daily average energy intake that was calculated from 3-day food records (2 weekdays and 1 weekend day) for every person. The macronutrient content of both groups was based on the percent of ingested calories comprising approximately 55% carbohydrate, 15% protein, and 30% fat. Diet was established by a registered dietitian based on food exchange systems in both the groups. In the group with nutrition education, six one-hour sessions were conducted over the initial 3 months. These led to an individual format about the food guide pyramid, goal setting for weight loss, self-monitoring, and stimulus control. Study flowchart is presented in Figure 1.
All statistical analyses were performed using SPSS version 13.0 (SPSS Inc., Chicago, IL, 2005). Data were checked for normality with Kolmogorov-Smirnov test. All variables had a normal distribution. Independent T-Test was used to compare between-group differences. General linear model repeated measures analysis of variance was employed to assess the trend of changes over 6 months for the time effect and the interaction between time and group effect. Paired t-test was used to compare the variable changes before and after the intervention in both groups. The significance level was set at P < 0.05.
4. Results
Descriptive characteristics of the study participants are presented in Table 1. Drop out was 26.5% at the 3-month period (31.1% in the diet group vs. 22.2% in the diet + education group) and 45.5% at the 6-month period (53.3% in the diet group vs. 37.7% in the diet + education group).
| Variable | Diet Group | Diet+ Education Group | P Value |
|---|---|---|---|
| Age, y | 28.40 ± 7.98 | 27.02 ± 6.37 | 0.37 |
| Weight, kg | 85.37 ± 11.44 | 84.72 ± 12.11 | 0.79 |
| BMI, kg/m2 | 32.28 ± 2.90 | 33.22 ± 3.16 | 0.92 |
| Waist circumference, cm | 103.91 ± 9.56 | 107.40 ± 11.45 | 0.12 |
| Energy intake at baseline, kcal | 2715.13 ± 1097.88 | 2806.98 ± 763.89 | 0.68 |
| Recommended energy, kcal | 2247.8 ± 219.02 | 2262.22 ± 235.28 | 0.67 |
A significant decrease in weight and an increase in the total score of WEL and all the subscales were observed in the entire study population at the end of the intervention (Table 2: the time effect). Significant differences were found in the trend of changes in weight, the total WEL score, availability of food, negative emotions, physical discomfort, and positive activities subscales between the groups (Table 2: the time × group effect), which suggests that the effect of intervention on the self-efficacy scores and weight was not the same for the two groups.
| Variable | Baseline | 3 Months | 6 Months | Time Effect, F (df), P Valueb | Time × Intervention Effect, F (df), P Valuec |
|---|---|---|---|---|---|
| Weight, kg | |||||
| Diet group | 85.37 ± 11.44 | 79.57 ± 11.17 | 75.50 ± 7.77 | 12.64 (2) | 5.69 (2) |
| Diet+ education group | 84.72 ± 12.11 | 78.34 ± 11.62 | 72.90 ± 13.16 | < 0.001 | 0.011 |
| Positive activities | |||||
| Diet group | 5.53 ± 2.15 | 6.09 ± 2.25 | 6.75 ± 1.99 | 15.68 (2) | 9.41 (2) |
| Diet + education group | 5.17 ± 2.39 | 6.53 ± 2.12 | 7.31 ± 1.70 | < 0.001 | < 0.001 |
| Physical discomfort | |||||
| Diet group | 5.74 ± 2.12 | 6.23 ± 2.23 | 6.78 ± 2.08 | 10.09 (2) | 8.28 (2) |
| Diet + education group | 5.23 ± 2.14 | 6.53 ± 2.24 | 7.08 ± 1.89 | < 0.001 | < 0.001 |
| Social pressure | |||||
| Diet group | 5.50 ± 2.09 | 6.31 ± 1.89 | 6.93 ± 1.67 | 12.27 (2) | 2.80 (2) |
| Diet + education group | 5.19 ± 2.47 | 6.19 ± 2.56 | 6.77 ± 2.53 | < 0.001 | NS |
| Availability of food | |||||
| Diet group | 4.85 ± 1.30 | 5.62 ± 2.23 | 6.40 ± 2.04 | 18.39 (2) | 6.52 (2) |
| Diet + education group | 4.13 ± 2.37 | 5.67 ± 2.66 | 6.31 ± 2.49 | < 0.001 | 0.002 |
| Negative emotions | |||||
| Diet group | 5.27 ± 2.53 | 5.91 ± 2.48 | 6.67 ± 2.25 | 12.24 (2) | 7.23 (2) |
| Diet + education group | 4.69 ± 2.62 | 6.05 ± 2.48 | 6.90 ± 2.19 | < 0.001 | 0.001 |
| Total WEL score | |||||
| Diet group | 5.38 ± 1.20 | 6.03 ± 2.01 | 6.73 ± 1.75 | 22.57 (2) | 11.30 (2) |
| Diet + education group | 4.89 ± 2.02 | 6.23 ± 2.28 | 6.95 ± 2.05 | < 0.001 | < 0.001 |
Changes in Weight, Total WEL Score and Its Subscales Over 6 Monthsa
The mean difference in weight loss and total self-efficacy score as well as in positive activities, physical discomfort, availability of food, and negative emotions subscales was higher in the diet + education group than in the diet group over 6 months (Table 3). The improvement in the total score of WEL and its subscales was greater in the first 3 months in comparison with the second 3 months after the intervention in the diet + education group (Table 4).
| Variable | Between Baseline and 3 Months | Between 3 and 6 Months | Between Baseline and 6 Months | |||
|---|---|---|---|---|---|---|
| Mean | P Valuea | Mean | P Valuea | Mean | P Valuea | |
| Weight loss, kg | 0.58 | 0.21 | 1.37 | 0.04 | 1.95 | 0.03 |
| Positive activities | 1.28 | 0.008 | 0.44 | 0.03 | 2.13 | 0.001 |
| Physical discomfort | 0.58 | 0.006 | 0.22 | 0.38 | 1.89 | 0.003 |
| Social pressure | 1.24 | 0.23 | 0.17 | 0.38 | 1.13 | 0.07 |
| Availability of food | 1.02 | 0.02 | 0.21 | 0.39 | 1.69 | 0.006 |
| Negative emotions | 1.72 | 0.008 | 0.36 | 0.20 | 2.02 | 0.002 |
| Total WEL score | 1.01 | 0.006 | 0.29 | 0.10 | 1.84 | 0.001 |
Mean Difference in Weight Loss, Total WEL Score and Its Subscales Between the Two Groups Over 6 Months
| Variables | Interval | P Valueb | |
|---|---|---|---|
| Baseline to 3 Months | 3 to 6 Months | ||
| Positive activities | |||
| Diet group | 0.34 | -0.09 | 0.180 |
| Diet + education group | 2.03 | 0.35 | 0.005 |
| Physical discomfort | |||
| Diet group | 0.11 | -0.02 | 0.721 |
| Diet + education group | 1.78 | 0.20 | 0.005 |
| Social pressure | |||
| Diet group | 0.57 | 0.01 | 0.137 |
| Diet + education group | 1.53 | 0.18 | 0.018 |
| Availability of food | |||
| Diet group | 0.56 | -0.02 | 0.046 |
| Diet + education group | 2.05 | 0.19 | 0.001 |
| Negative emotions | |||
| Diet group | 0.21 | 0.11 | 0.776 |
| Diet + education group | 1.87 | 0.47 | 0.023 |
| Total WEL score | |||
| Diet group | 0.36 | -0.005 | 0.157 |
| Diet + education group | 1.91 | 0.29 | <0.001 |
Comparison of Mean Scores of Self-Efficacy and Its Subscales After the Interventiona
5. Discussion
This study provided important information about self-efficacy and its changes during weight loss intervention. Based on the results, nutrition education was associated with a greater weight loss and higher total self-efficacy and its subscales scores. This information can be useful to help with person’s inner desire to want to lose weight.
The previous study supports the assessment of self-efficacy in obese persons seeking weight loss treatment (17). In this study, self-efficacy among obese women attending the nutrition clinic was less than that reported in other studies (4, 8, 11, 18). Two of these studies (8, 11) included men and eating self-efficacy may vary by gender. In previous research, men reported higher self-efficacy than women (19, 20). Histories of frequent dieting could undermine women’s confidence in the successful management of their eating (19).
The minimum confidence to resist eating was observed in the availability of food subscale at baseline. This result was consistent with the results of previous studies among obese women (8, 10, 18). The individuals’ confidence to resist eating due to external circumstances is an important cognitive dimension of weight loss (9). This subscale has been reported as the strongest and the most consistent predictor of weight loss (21). The strengthening of strategies targeting this subscale must be considered in interventions.
The improvement of self-efficacy may help participants lose more weight during treatment (17). The higher self-efficacy at the end of the treatment has been associated with more weight loss at follow-up (20, 22). In accordance with previous research (4, 9, 12), we found a significant improvement in the total WEL score and all five subscales during both of the interventions.
Participation in a treatment along with nutrition education has been reported with changes in measures of self-efficacy (14) and perceived barriers reduction (23). This study showed that individualized nutrition education could be more effective in increasing self-efficacy and more weight loss over 6 months. A greater difference was observed in self-efficacy and its subscales in the first 3 months rather than in the second 3 months in the diet + education group. Previous research has found that early weight loss consistently is related to longer-term outcomes (24). It seems that interventions should consider approaches that directly strengthen self-efficacy and promote more weight loss.
The greatest difference between the groups was observed in the negative emotions subscale at 3 months after the intervention. The obese experience more negative emotions, lose control of their food intake, and revert to overconsumption (25) and difficulty in coping with negative emotions has been associated with reduced dietary compliance (26). Berman’s study indicated that low confidence in the ability to control eating while experiencing negative emotions was associated with greater bulimic behaviors (27). The emotional eating is associated with poorly maintained weight loss in long-term (28). Hence, greater self-efficacy in this subscale in the diet + education group can be more effective in weight loss success.
6 months after the intervention, the greatest difference between the groups was observed in the positive activities subscale. In Richman’s study, women who completed the behavior modification intervention had higher scores in this subscale (18). Distractions can increase food consumption. Past research indicates that obese persons have a greater tendency to be distracted than non-obese people (29). It is certain that more confidence to resist eating in such circumstances can be important in weight loss and maintenance.
No significant difference was found in the social pressure subscale between the groups. Social pressure to eating has been reported higher in females (30). Social eating (Taarof) can be considered a norm among Iranian people (31) because refusing to join others in eating may be considered a rude behavior. This is not an issue exclusive to the Iranian culture (32). Therefore, using culturally tailored weight loss education will be most useful.
The strengths of the current study were in its prospective design, assessment of energy intake, and moderate reduction in calorie during 6 months. This study had some limitations. In this study, the dropout rate was high. The attrition rate, as a common problem for long-term weight loss interventions (33) may have restricted the ability to find stronger results. It is certainly possible that participants who drop out represent a unique set of individuals with different outcomes. Another limitation is that the information regarding caloric intake was self-reported, and thus subjected to potential biases. Therefore, future investigations should evaluate the relationship between changes in self-efficacy subscales and longer-term outcomes with a larger group of individuals.