1. Background
Addiction as a chronic, progressive, and destroying disease (1) is concerned as a serious public health problem in the world, which may lead the addict to cause serious harm to their family, addicted person, and community (2). The strategic situation of Iran as well as the geographic limits, with countries as production centers of opioid substances in the world, leads to the high prevalence of addiction and substance abuse in Iran (3). Currently, the prevalence of 12-month drug addiction, any illicit drugs, according to the DSM-5 criteria, is 2.44% of the Iranian population (4). Although the social and cultural characteristics and related common attitudes to addiction in community can involve various levels of people in substance abuse (5), one of the major challenges in this field is a high rate of slip and relapse among addicts (6, 7). The relapse generally indicates the treatment program, personal failure, or both (8). It is a complex phenomenon where both neurobiological processes and socio-psychological factors play roles in this phenomenon. Relapse as a failure experience usually had various consequences for patient, caregivers, and health professionals (9).
Relapse and a slip reflect the duration and the severity comeback to the past addictive behaviors. Otherwise, relapse suggested as a complete comeback to the past addictive behaviors that it may last for 1 or 2 days, 1 month, or even more than 1 month, however, a slip refers to the 1 time during 1 day and it is concerned as a temporary period, not severe comeback and addictive behavior (10). Drug addiction theories have special emphasis on the biological changes and their interactions with socio-psychological factors in the relation with relapse continuation. According to the most penetrating socio-psycho-behavioral models by Marlatt, the relapse is defined as a manifest, which abuse of substance occurs as a last event of long strict of non-adjustment responses to the internal or external stressful factors (11). According to the differential theory, the behavior derivates from learning values, motivations, and techniques related to the promise of not desirable behavior to intimate friends (8). Jiloha (2011) believes that more traditional situations include internal thoughts and external events act as predictable triggers for relapse (10).
Based on the conducted studies, lower age and unemployment, education, history of addiction treatment, addict friends, marital status, poor perceived social support, degree of distress induced by substance abuse, distress of comorbid psychiatric disorders, treatment duration, lack of family and friends support, negative emotional traits and skill deficits, family history of addiction, times of past relapses, not effective and non-adjustment coping strategies, more risk full situations, as well as more stressful life events are related to a greater probability of a relapse (9, 11-13).
In general, the different researchers indicate that only 26% to 72% of addicts can continue discontinuation of substance for more than 1 year and adhere to treatment (14, 15). This rate has been reported for the Iranian patients about 30% - 50% (6, 12) and it suggests the necessity to relapse and slip among under treatment addict patients. In another hand, although the assessment of effective factors has been emphasized in 3 levels of before, during, and after treatment (13), the treatment and medication related factors are less of a concern than the other factors.
2. Objectives
Therefore, due to the concern of this issue where most of the addicts have a relapse in the first year of treatment, especially the first 3 to 6 months (6, 9), the present study aimed to assess the predictors of slip and relapse among addicts during the first 6 months of treatment with an emphasis on treatment related factors.
3. Methods
3.1. Design and Context
In this cross-sectional study, addict patients who were referred to the Methadone/ Buprenorphine Maintenance Therapy (MMT/BMT) clinics in Kermanshah city-Iran during April-September 2015 were asked to participate in this research. Kermanshah city is the center of Kermanshah province in the western part of Iran that is 326 miles to Tehran (Capital of Iran). Based on census 2011, the population of this city was estimated as 851405. The MMT/BMT clinics of this city are the professional outpatient clinics for substance abuse treatment (6).
3.2. Inclusion and Exclusion Criteria
The inclusion criteria consisted of positive urinary opium test, addiction approval by a physician, primary registration in a MMT/BMT clinic, tendency to treatment, age in range of 18 - 65 year, education level higher than primary school, ability to appropriate communication in Persian language, and tendency to participate. The exclusion criteria consisted of taking medical or psychiatric medication for substance abuse treatment in another center, lack of concordance in self-reported information and medical record, and lack of response to calls in follow-up periods.
3.3. Participants
The sample size consists of 148 addict patients who were admitted and treated in 6 a month period (April to September 2015) in 5 MMT/BMT clinics of Kermanshah city. These cases were selected through cluster multi-phases method from 5 urban areas. One clinic randomly selected from 1 area and about 40 patients (200 individuals as a total) selected from 1 clinic. 52 patients were excluded caused to lack of inclusion criteria and 148 individuals entered to analysis. Due to the fact that our model includes 12 predictor variables (without gender variable because of very few female cases in this research) and the formula (N > 50 + 8 m), which was used progressively in the regression analysis, the minimum sample size of this research is 146 cases (16). All 148 cases entered the analysis; therefore our sample size seems appropriate for the regression analysis.
3.4. MMT/BMT Clinics and Treatment Protocol
The MMT/BMT clinics are the professional outpatient clinics for substance abuse treatment. In these centers, the agonists of opioids, which act on μ receptor as same as natural opioids, are prescribed for substance abuse treatment. These medications include Methadone (2, 17) as pure agonist of μ receptor, Buprenorphine (2, 17) as partial agonist of μ receptor and k receptor and tincture of opium. Although the main medication is methadone, approximately 20% of patients are treated by buprenorphine and tincture of opium due to the fact that tincture of opium has a short history in Iran and sublingual 2 and 8 milligram tablets of buprenorphine are not available in pharmaceutical market of Iran (18).
The MMT/BMT clinics are classified in 3 grades in Iran: The 3rd grade clinic has this item: maximum of admittance as 50 patients and at least 1 physician, 1 clinical psychologist, 2 nurses, and 1 social worker. The 2nd grade clinic has the capacity of 100 admittances, at least 2 physicians, 1 clinical psychologist, 4 nurses, and 1 social worker. The 1st grade clinic has the maximum capacity of 200 admittances, at least 4 physicians, 1 clinical psychologist, 8 nurses, and 1 social worker (18).
The initial dosage of methadone is 10 to 30 milligrams and depends on the amount and type of substance after the primary interview with the physician, patient’s identity, and formation of medical record. This initial dosage can be increased after the 3rd day. This dosage may exceptionally and progressively be increased to 120 milligrams if the patient needs a higher dosage. After these levels are named as induction and stabilization phases and they usually last 6 weeks, the maintenance phase begins. In this phase the stabilization of patient’s condition is more concerned. In the maintenance treatment phase with methadone, the dosage increased to the level that withdrawal symptoms are not seen and the crave for illegal abuse is at minimum level. The maintenance treatment phase lasts at least several months and usually more than 1 year, even it continues for a lifetime. In this protocol, the patient refers daily at indicated hours for receiving medication in the first 2 months. In the 3rd and 4th months, if the patient is stable, he/she refers every 2 days and receives the home dose. Finally, in the end of 6th month, patients refer weekly for medication and other health services and they receive the weekly dose of methadone (18).
3.5. Care Subsidy
The license of MMT/BMT clinics is given under supervision of the welfare organization and Medical Sciences University in Iran and inceptors of these organizations assess the commitment to the legal introductions monthly. Regarding the poor patients’ economic condition and lack of coverage of health insurances for addiction treatment, welfare organization provides care subsidy packs monthly, every 3 or 6 months, so patients receive 30% to 50% discounts for treatment of MMT/BMT clinics in the first 3 - 6 months of treatment.
3.6. Data Collection
After verbal approval of the ethical committee of Kermanshah University of Medical Sciences and satisfaction of heads of MMT/BMT clinics, the patients identified and referred voluntarily to the research team. After providing assurance to the patients about the confidentiality of their identity, demographic, treatment, and history checklists were gathered. The physician of the team recorded the demographic, treatment and history checklists after adjustment with data, which gathered by MMT/BMT teams for accuracy approval. The amount of subsidy and monthly payment recorded accurately. The comorbidity index was recorded by the physician during the interview. The data related to the urinary opium test during the 6-month follow-up derivate from the medical record. In case of discontinuation of treatment, a call follow-up was done and the patient is registered as a relapse case after reference to clinic and interview.
3.7. Instruments
3.7.1. Demographic, History and Treatment Checklists
The self reported items included gender, age, education level, marital status, addict relative or friend, type of medication (methadone, buprenorphine, tincture of opium), dosage (mg), satisfaction about dosage, monthly treatment cost (IR. Rial), history, and type of past treatment (physicians prescribed medication, medication without physician prescription through illegal methadone or buprenorphine, residency in a treatment center without medication, self-treatment without medication, and use of 2 mentioned items) were recorded in baseline after adjustment with medical record and physicians approval.
3.7.2. Slip and Relapse
Regarding the lack of acceptable and comprehensive definition for a relapse and slip, in this research these items assessed through positive morphine urinary test 7: approval of slip in positive test for 1 or 2 times in a 6-month follow-up, and approval of relapse in positive test for more than 2 times in a 6-month follow-up. Also, the social worker call excluded patients and they were admitted to refer to the center. After insurance regarding their desire to discontinue treatment, lack of registration to another center and approve of substance abuse, these patients were entered to the relapse group. It should be mentioned that morphine urinary test were done 2 - 3 times a month by a physician diagnosis and recorded in the patients’ medical record. Finally, data were recorded in demographic, history, and treatment forms.
3.7.3. Comorbidity Index
This scale was made by Ifudu et al. in 1998 and it is a grading scale for assessment of related physical diseases in patients that consists of 14 components for evaluation of main physical systems, which included: 1) ischemic heart disease, 2) other cardiovascular problems, 3) chronic respiratory disease such as asthma, 4) autonomic neuropathy, 5) other neurological problems, 6) neuromuscular disorders, 7) infections such as HIV, 8) pancreas and biliary diseases, 9) blood disorders, 10) back pain, spine and joints disorders, 11) visual disorders (decreased visual to complete blindness), 12) limb disorders, 13) genitourinary diseases, and 14) psychiatric disorders. Each item receives a score from 0 (lack of physical relative disease) to 3 (severe relative disease) (19).
3.7.4. Satisfaction About Dosage
As mentioned, the dosage was provided and indicated by the physician in several phases. Regarding the emphasis for reduction of probable induced overdose medication harms, the necessary dose was indicated accurately. Despite this issue, some of the patients are not satisfied about their dose because of different reasons. We recorded this item through a single item, which includes: “Do you satisfy about your dose of medication?”, The responses recorded as: no, I don’t satisfy (= 1), yes I satisfy about it (= 2).
3.8. Statistical Analysis
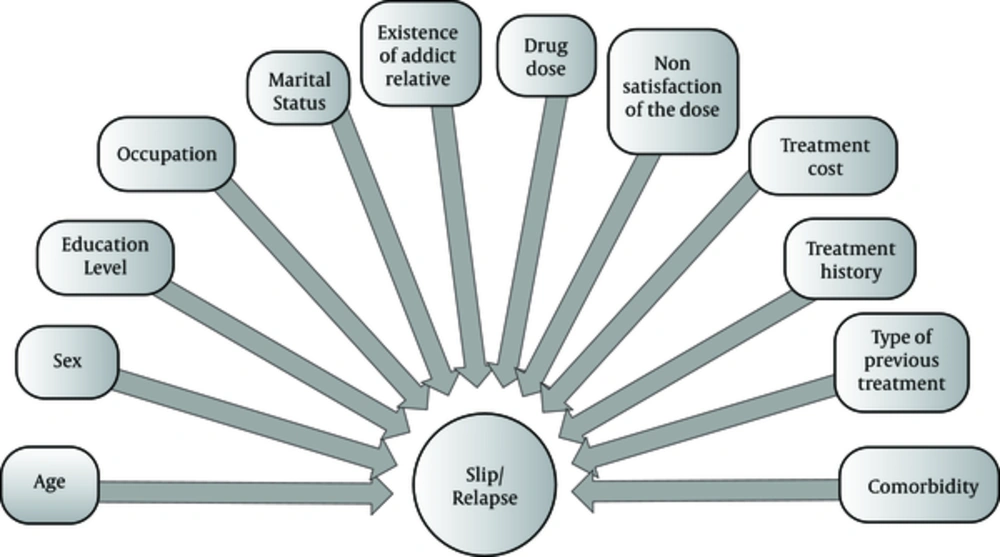
The patients’ characteristics with and without relapse and slip were compared through chi-square for nominal and classified variables and independent t-test for continuous variables. At the baseline, the percentages of not continuous variables, mean, and standard deviation of continuous variables were reported. Binary logistic regression analysis was used for demographic correlatives, present treatment, history of disease, and diseases related to slip and relapse. Gender, age, education level, marital status, job, addict relative or friend, type of medication, dosage, satisfaction about dosage, monthly treatment cost, history, and type of past treatment were entered to analysis. In this analysis, all demographic variables included gender, age, education, job, and marital status were adjusted. Finally, SPSS version 20 was applied for an analysis and P < 0.05 concerned as significant level. Before analysis, needed presumptions for Binary logistic regression analysis (normality, collinearity, and multicollinearity) were assessed. The main analysis was done after approval of overruns of presumptions (16). The predictive model of slip and relapse is seen in Figure 1.
4. Results
The mean age of total cases was 42.4 ± 11.3 years and 98% of participants were male. 27% and 35.1% of 148 participants had a slip and relapse, respectively. The demographic characteristics, histories of treatment and disease, and comorbidities in generally and separated were indicated in Table 1. As seen, there are significant differences between the 2 groups with and without slip in age (P = 0.016), education (P = 0.023), job (P = 0.026), satisfaction about medication (P = 0.036), and type of past treatment (P = 0.018) at baseline. Also, there are significant differences between 2 groups with and without relapse in treatment costs (P = 0.041), history of treatment (P = 0.006), and type of past treatment (P = 0.010).
| Characteristic | Overall Population, n = 148 | Non-Slip, N = 108 (73.0%) | Slip, N = 40 (27.0%) | P Valueb,c | Non-Relapse, N= 96 (64.9%) | Relapse, N = 52 (35.1%) | P Valueb,c |
|---|---|---|---|---|---|---|---|
| Age, y | 42.4 ± 11.3 | 43.8 ± 12.0 | 38.8 ± 8.1 | 0.016d | 43.6 ± 12.0 | 40.3 ± 9.5 | 0.097 |
| Sex | 0.287 | 0.198 | |||||
| Female | 2.0 | 2.8 | 0.0 | 3.1 | 0.0 | ||
| Male | 98.0 | 97.2 | 100 | 96.9 | 100 | ||
| Education level | 0.023d | 0.071 | |||||
| Less than diploma | 56.1 | 59.3 | 47.5 | 57.3 | 53.8 | ||
| Diploma | 29.0 | 23.1 | 45.0 | 24.0 | 38.5 | ||
| Academic | 14.9 | 17.6 | 7.5 | 18.7 | 7.7 | ||
| Occupation | 0.026d | 0.063 | |||||
| Clerk | 18.9 | 22.2 | 10.0 | 19.8 | 17.3 | ||
| Market | 63.5 | 59.3 | 75.0 | 59.4 | 71.2 | ||
| Housewife | 2.0 | 2.8 | 0.0 | 3.1 | 0.0 | ||
| Retired | 9.5 | 12.0 | 2.5 | 13.5 | 1.9 | ||
| Unemployed | 6.1 | 3.7 | 12.5 | 4.2 | 9.6 | ||
| Marital status | 0.230 | 0.781 | |||||
| Single | 14.2 | 13.9 | 15.0 | 15.6 | 11.5 | ||
| Married | 82.4 | 84.3 | 77.5 | 81.3 | 84.7 | ||
| Divorced or widowed | 3.4 | 1.8 | 7.5 | 3.1 | 3.8 | ||
| Existence of addict relative | 85.8 | 86.1 | 85.0 | 0.863 | 83.3 | 90.4 | 0.241 |
| Drug type | 0.293 | 0.701 | |||||
| Methadone | 91.9 | 89.8 | 97.5 | 90.6 | 94.2 | ||
| Buprenorphine | 6.1 | 7.4 | 2.5 | 7.3 | 3.9 | ||
| Opium tincture | 2.0 | 2.8 | 0.0 | 2.1 | 1.9 | ||
| Drug dose | 81.7 ± 30.1 | 81.5 ± 32.3 | 82.3 ± 23.8 | 0.891 | 80.6 ± 30.6 | 83.6 ± 29.5 | 0.561 |
| Non satisfaction of the dose | 16.9 | 13.0 | 27.5 | 0.036d | 15.6 | 19.2 | 0.576 |
| Treatment cost, Iranian Rial | 1150.9 ± 281.6 | 1130.3 ± 183.0 | 1220.9 ± 447.3 | 0.064 | 1120.4 ± 168.7 | 1220.3 ± 411.3 | 0.041d |
| Treatment history | 77.7 | 75.0 | 85.0 | 0.194 | 70.8 | 90.4 | 0.006d |
| Type of previous treatment | 0.018d | 0.010d | |||||
| Never | 22.3 | 25.0 | 15.0 | 29.2 | 9.6 | ||
| Medication prescribed by a doctor (MMT/BMT) | 22.3 | 23.1 | 20.0 | 18.8 | 28.8 | ||
| Medication non prescribed by a doctor | 23.6 | 22.3 | 22.5 | 22.9 | 25.1 | ||
| Stay on treatment centers without medication | 4.1 | 4.6 | 2.5 | 5.2 | 1.9 | ||
| Self-treatment without medication | 6.1 | 8.3 | 0.0 | 8.3 | 1.9 | ||
| Using two methods | 21.6 | 14.8 | 40.0 | 15.6 | 32.7 | ||
| Comorbidity | 2.44 ± 1.7 | 2.40 ± 1.7 | 2.57 ± 1.9 | 0.583 | 2.47 ± 1.6 | 2.40 ± 1.9 | 0.828 |
Baseline Characteristics in the Overall Population and by Slip and Relapsea
4.1. Slip
After adjustment for all demographics including gender, age, marital status, education, and occupation, Table 2 displays the adjusted odds ratio, 95% confidence interval, and p value for each covariate included in the binary logistic regression model. In relation with the regression model, the Hosmer-Lemeshow test indicated that the fitness of model is appropriate (P = 0.897) and our model predicts 79.7% of membership of group correctly. The model was statistically significant overall (Chi-square = 62.215; P < 0.0005). Of the 13 variables included as covariates in the regression, 5 were found to be independently significantly associated with a slip. Indicators of effect size showed suitable explanatory power with respect to slip (Cox and Snell R2 = 0.343; Nagelkerke R2 = 0.498). Therefore, it suggests that our model can explain 34.3% to 49.8% of a variance of slip.
| Characteristic | Slip, % | Adjusted OR | P Value | Relapse, % | Adjusted OR | P Value |
|---|---|---|---|---|---|---|
| Age, y | - | 0.97 (0.92 - 1.02) | 0.244 | - | 0.98 (0.94 - 1.03) | 0.381 |
| Sex | ||||||
| Female | 0.0 | Referent | 0.0 | Referent | ||
| Male | 27.6 | 7.24 (0.00 - ….) | 0.998 | 35.9 | 4.89 (0.00 - ….) | 0.999 |
| Education level | ||||||
| Less than diploma | 22.9 | Referent | 33.7 | Referent | ||
| Diploma | 41.9 | 5.14 (0.61 - 43.33) | 0.133 | 46.5 | 0.85 (0.16 - 4.52) | 0.846 |
| Academic | 13.6 | 2.55 (0.17 - 38.37) | 0.497 | 18.2 | 0.30 (0.04 - 2.28) | 0.244 |
| Occupation | ||||||
| Clerk | 14.3 | Referent | 32.1 | Referent | ||
| Market | 31.9 | 13.35 (1.17 - 152.53) | 0.037c | 39.4 | 1.00 (0.19 - 5.21) | 0.997 |
| Housewife | 0.0 | 0.00 (0.00 - ….) | 0.999 | 0.0 | 0.00 (0.00 - ….) | 0.999 |
| Retired | 7.1 | 13.94 (0.45 - 431.12) | 0.132 | 7.1 | 0.00 (0.00 - 5.37) | 0.407 |
| Unemployed | 55.6 | 24.75 (0.80 - 767.69) | 0.067 | 55.6 | 2.84 (0.20 - 40.01) | 0.438 |
| Marital status | ||||||
| Single | 28.6 | Referent | 28.6 | Referent | ||
| Married | 25.4 | 5.18 (0.62 - 42.90) | 0.127 | 36.1 | 3.26 (0.59 - 17.94) | 0.175 |
| Divorced or widowed | 60.0 | 8.48 (0.00 - ….) | 0.998 | 40.0 | 0.94 (0.04 - 19.69) | 0.966 |
| Existence of addict relative | 26.8 | 1.40 (0.30 - 6.56) | 0.672 | 23.8 | 2.28 (0.57 - 9.04) | 0.242 |
| Drug type | ||||||
| Methadone | 28.7 | Referent | 36.0 | Referent | ||
| Buprenorphine | 11.1 | 0.08 (0.00 - 2.60) | 0.153 | 22.2 | 0.67 (0.06 - 7.46) | 0.748 |
| Opium tincture | 0.0 | 0.00 (0.00 - ….) | 0.999 | 33.3 | 0.40 (0.01 - 11.02) | 0.589 |
| Drug dose | - | 0.99 (0.97 - 1.01) | 0.466 | - | 1.00 (0.98 - 1.02) | 0.964 |
| Non satisfaction of the dose | 44.0 | 0.22 (0.07 - 0.72) | 0.012c | 40.0 | 0.90 (0.30 - 2.68) | 0.855 |
| Treatment cost | - | 1.04 (0.75 - 1.34) | 0.049c | - | 1.01 (0.46 - 1.89) | 0.106 |
| Treatment history | 29.6 | 4.97 (1.20 - 20.54) | 0.027c | 40.9 | 6.37 (1.66 - 24.44) | 0.007c |
| Type of previous treatment | ||||||
| Never | 18.2 | Referent | 15.1 | Referent | ||
| Medication prescribed by a doctor (MMT/BMT) | 24.2 | 0.25 (0.06 - 0.97) | 0.046c | 45.4 | 0.74 (0.24 - 2.30) | 0.605 |
| Medication non prescribed by a doctor | 25.7 | 0.47 (0.12 - 1.81) | 0.273 | 37.1 | 0.73 (0.21 - 2.45) | 0.607 |
| Stay on treatment centers without medication | 16.7 | 0.10 (0.00 - 2.15) | 0.142 | 16.7 | 0.17 (0.01 - 2.29) | 0.183 |
| Self-treatment without medication | 0.0 | 0.00 (0.00 - ….) | 0.999 | 11.1 | 0.07 (0.01 - 0.85) | 0.037c |
| Using two methods | 0.0 | 0.00 (0.00 - ….) | 0.998 | 53.1 | 0.00 (0.00 - ….) | 0.997 |
| Comorbidity | - | 1.21 (0.91 - 1.61) | 0.192 | - | 1.08 (0.83 - 1.40) | 0.558 |
The results of this table show that patients with a market job compared to clerks (AOR = 13.35; 95% CI = 1.17 to 152.53; P = 0.037), those who pay higher costs for treatment (AOR = 1.04; 95% CI = 0.75 to 1.34; P = 0.049), and people with treatment history (AOR = 4.97; 95% CI = 1.20 to 20.54; P = 0.027) have a more likely change for a slip. The patients with a higher satisfaction of the medication dose (AOR = 0.22; 95% CI = 0.07 to 0.72; P = 0.012) and people with medication history prescribed by a physician (AOR = 0.25; 95% CI = 0.06 to 0.97; P = 0.046) have a less likely chance for a slip.
4.2. Relapse
After adjustment for all demographics, Table 2 also displays the adjusted odds ratio, 95% confidence interval, and p value for each covariate included in the binary logistic regression model for relapse. In relation with the regression model, Hosmer-Lemeshow test indicated that the fitness of model is appropriate (P = 0.264) and our model predicts 75.7% of membership of group correctly. The model was statistically significant overall (Chi-square = 45.744; P = 0.014). Of the 13 variables included as covariates in the regression, 2 were found to be independently significantly associated with relapse. Indicators of effect size showed suitable explanatory power with respect to relapse (Cox and Snell R2 = 0.266; Nagelkerke R2 = 0.366). Thus, it suggests that our model can explain 26.6% to 36.6% of a variance of relapse.
The results of this table show that patients with treatment history compared to patients without it (AOR = 6.37; 95% CI = 1.66 to 24.44; P = 0.007) are 6.37 times more likely to have a relapse. The patients with self-treatment without medication were compared to individuals without a treatment history (AOR = 0.07; 95% CI = 0.01 to 0.85; P = 0.037) have a less likely chance for a relapse.
5. Discussion
The present study aimed to assess the predictors of substance abuse slip and relapse among addicts in the first 6 months of treatment with an emphasis on treatment related factors. Kassani et al. (6) findings (17% relapse in the first 6 months) are concordant with our findings (27% and 35.1% of 148 participants had slip and relapse respectively). The results suggested that self-employment, more treatment costs, previous treatment history, not satisfied dose of medication, and lack of medical therapy under physician’s supervision can increase the possibility of a slip significantly. In addition, the previous treatment history increases the relapse possibility to 6.37 times otherwise the self-treatment history without medication decreases the possibility of a relapse to 0.07 times. Our results about the role of job, (11, 12, 20, 21) received dose (22-24), high costs due to lack of support of insurance organizations or subsidy, (20) and history of treatment (11, 23) ,are concordant to the past studies.
Our results show that job status is effective in slip and treatment failure, therefore, those with a market job are more at risk of a slip compared to employees. According to the results of a meta-analysis (25), job status and unemployment of patients is a serious risk factor for the emergence of substance abuse and risk-taking. Also, job status may predict a relapse and treatment failure (25). On the other hand, employee patients compared with those with a market job usually have a lower level of education, which may be a serious factor of a slip (20, 24). It suggested that illiteracy and lower education can increase the probability of slip and relapse about 5 times (11). In addition, instability of economic conditions in Iran caused that people with personal jobs contact to significant challenges in prediction of marketing fluctuations. They have lower economic insurance compared to employees and experience more stress. Also, patients with market jobs communicate with various clients and generally they experience a higher risk full of situations and stressful events, which may lead to a slip in lack of efficient coping skills (9, 13, 26). Finally, patients with a market job who work in the mornings and evenings leads to fatigue and slip, however employees have fewer work hours (21).
According to another finding, more costs and lack of satisfaction regarding dose can increase the probability of slip. Higher costs, especially in unemployed cases (25), lead to avoidance to reference and they are at risk of a slip due to physical and psychological stresses. Previous reports show that subsidy on pharmacotherapy and using cost-effective strategies are effective in increasing adherence to treatment (27). Mutter et al. (20) suggested that personal insurance is a main factor in completing the treatment. However, Iranian insurance organizations do not support addict patients in MMT/BMT clinics and these patients use from subsidies of welfare organization in short time. On the other hand, there are legal limitations for delivery of high doses (18), where in most cases (44% in the present study) lead to lack of satisfaction. Therefore, a disabled patient who has to pay the cost of a treatment does not receive an adequate dose and might lead to a slip. In addition, the results of a study indicated that patient’s perception about the dose can increase the severity of pain (28) and slip.
Another result indicates that the history of past treatment increases the probability of a slip and relapse. In this regard, Taymoori and Pashaei found that history of unsuccessful treatment has reduced addicts’ self-confidence in drug abstinence (29). It seems that patients with failed history have more physical and psychological dependency to opioids where their increasing behavioral problems may lead to increase of relapse (11). These patients probably have lower self-efficacy and not desirable treatment outcomes that lead to failure of treatment (23). Another problem are irrational beliefs such as avoidance from problem and lack of emotional responsibility among these patients (30) as well as their ineffective coping skills (26). In patients with failed history of treatment, avoidance from problems related to withdrawal symptoms such as pain and lack of emotional responsibility about treatment are the reasons of failure that may be generalized to the present treatment and explain the failure of the present treatment.
Finally it was indicated that patients with history of treatment in MMT/BMT centers are at a lower risk of a slip and patients with self-treatment without medication are at a lower risk of a relapse. Based on the results of a study, the probability of relapse in MMT patients are fewer 23% than others and this treatment can delayed this probability significantly (31). The past experience of MMT/BMT treatment can increase the patient’s adjustment with the present treatment and modify his/her expectations from treatment. These patients have better knowledge regarding treatment and future challenges (32) that it insured them about self-management of medication (33). The result of this adjustment and insurance is the lower probability of a slip. In addition, patients with self-treatment without medication usually experience more physical pain that they do not experience in this treatment. Lower pain and higher quality of life (28) during the present treatment is a concern as a positive enhancer that decreases the probability of relapse.
5.1. Strengths and Limitations
Unlike previous studies that focused on personal and environmental factors related to slip and relapse, the major points of the present study are the emphasis on variables and treatment related factors. Given that after a relapse and discontinuation of treatment program access to the patients was difficult, we can followed the patients only for 6 months. In addition, due to lack of access to standard and short instruments, we did not assess the external and internal (such as family function and irrational beliefs of patients) related factors to slip and relapse. Finally, we used the single item form in evaluation of patients’ satisfaction about dosage of medication that the standard questionnaire for quantity assessment in the future studies.
5.2. Conclusion
Despite that prevention of re-abuse and relapse of disease includes multi-factorial approach, it seems that the treatment-related factors are as the most major factors in relapse and a slip during the first 6 months of treatment. Health practitioners’ special attention to the treatment related factors in addiction, especially previous treatment, as the most important predictor of relapse, is probably effective in control and decrease of slip and relapse.