1. Background
Addiction is a global dilemma that requires serious attention because it affects not only people's physical and mental health, but also social and economic aspects (1). Addicts have no control over the use of drugs and continuous drug use causes health, family, job, and legal problems (2). Obviously, solutions must be provided to deal with this problem. Some of these problems can be addressed with scientific therapies that are suitably stable and prolonged. One of these measures is methadone maintenance therapy (MMT) that keeps the patient in a slow and gentle way of reducing mental fluctuations and improving health. In this therapy, the patient receives a set of medical, pharmaceutical, and psychotherapy treatments (3). MMT does not result in a complete disruption in drug use, but can avoid leaving the treatment and reduce depression, social and familial disorders, death, suicide, serious delinquencies, and unsuccessful marriages (4, 5). On the other hand, the replacement of various drugs with methadone reduces the prevalence of life-threatening diseases such as AIDS and hepatitis C, which are transmitted through injecting drug use. A study by Dastjerdi et al. (6) about the effect of methadone on the reduction of high-risk behaviors showed that 86% of opioid addicts on methadone treatment began to avoid joint infusion and self-harm after six months of therapy, and only 14% continued unprotected sex. A study by Raisi Dehkordi et al. (7) in Tehran showed decreased depression and anxiety and improved quality of life in methadone-treated addicts so that after one month, 48% were not depressed. Moreover, since methadone is an oral drug, it often reduces the effects of addiction, such as liver problems, gastrointestinal tract infections, skin ulcers, and mortality due to drug injecting (8-10).
2. Objectives
Considering the fact that the issue of addiction withdrawal has become widespread in Iran in recent years and it has attracted the attention of many people, especially the youth, this study aimed to determine the efficacy of MMT in addicts referring to Samen Al-Aemmeh center in Kermanshah. We surveyed demographic characteristics, drug relapse, drug use method, depression, anxiety, and quality of life in addicts.
3. Methods
In this descriptive cross-sectional study on addicts referring to the methadone therapy center of Samen Al-Aemmeh in Kermanshah in 2017, a random sample of 275 addicts with an accuracy of 5%, and a confidence level 95% was selected. The data collection tools consisted of four questionnaires. The first questionnaire was composed of three parts: demographic information (age, sex, education level, occupation, marital status, and history of imprisonment), type of addiction (cigarettes, alcohol, opium, heroin, opium juice, etc.), and the method of consumption (ingestion, inhalation, smoking, intravenous and non-venous injections). The other three questionnaires included the Beck depression inventory (Cronbach's alpha coefficient: 0.9) (11), the World Health Organization Quality of Life Questionnaire (WHOQOL-26) in four domains of physical health, psychological health, social relationship, and environment (Cronbach's alpha coefficient: > 0.7) (12), and Spielberger Anxiety Inventory (Cronbach's alpha coefficient: 0.86 - 0.95) (13). According to the Beck Depression Inventory, people with a score of less than 16 have no depression, 17 - 25 have mild depression, 26 - 34 have moderate depression, and more than 34 have severe depression. The Spielberger questionnaire was designed based on a Likert-type scale that non- anxiety and high anxiety have 1 and 4 scores, respectively. Data were collected in two steps: before the start of the MMT and six months after the start of the MMT. Data analysis was done by SPSS version 20 software at a confidence level of 95%. Data normality was assessed by the Kolmogorov-Smirnov test. The McNemar test and t-test were used to determine the effects of therapy on qualitative and quantitative variables, respectively. Pearson correlation and ANOVA tests were applied to identify differences between the domains of the quality of life.
4. Results
The demographic characteristics of the sample are presented in Table 1. Most participants were in the age range of 20 - 30 years, unemployed (63.63%), single (50.9%), with a history of imprisonment (due to addiction-related crimes) (60.72%), and intermediate education level (57.81%). The independent t-test showed no significant relationship of addiction with marital status (P > 0.05), but there were significant relationships with other variables.
| Parameters | No. (%) |
|---|---|
| Gender | |
| Male | 223 (81.09) |
| Female | 52 (18.9) |
| Age | |
| 20 - 30 | 106 (38.54) |
| 31 - 40 | 85 (30.9) |
| 41 - 50 | 62 (22.54) |
| 51 - 60 | 22 (8) |
| Education level | |
| Intermediate | 159 (57.81) |
| Diploma | 112 (40.72) |
| Academic | 4 (1.47) |
| Job status | |
| Employed | 100 (36.36) |
| Unemployed | 175 (63.63) |
| Marital status | |
| Single | 140 (50.9) |
| Married | 135 (49.1) |
| History of imprisonment | |
| Yes | 167 (60.72) |
| No | 108 (39.27) |
Characteristics of the Participants in This Study
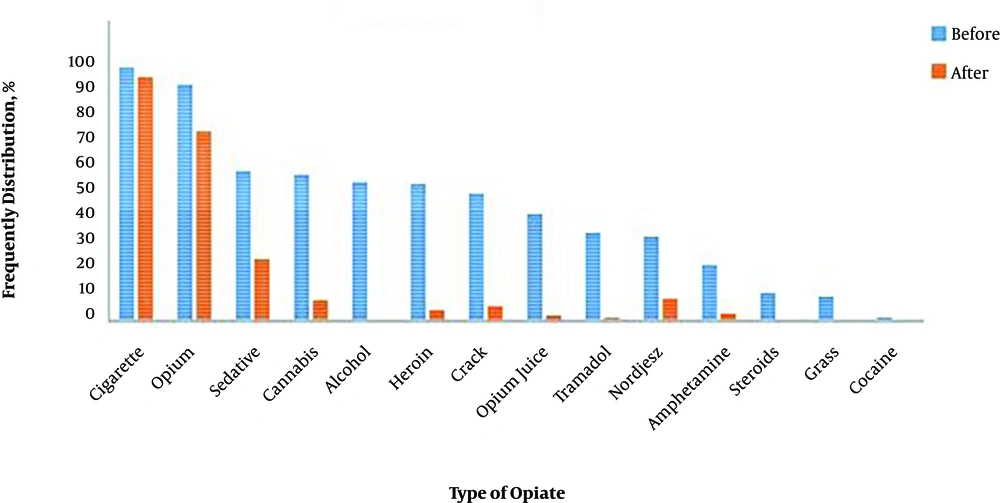
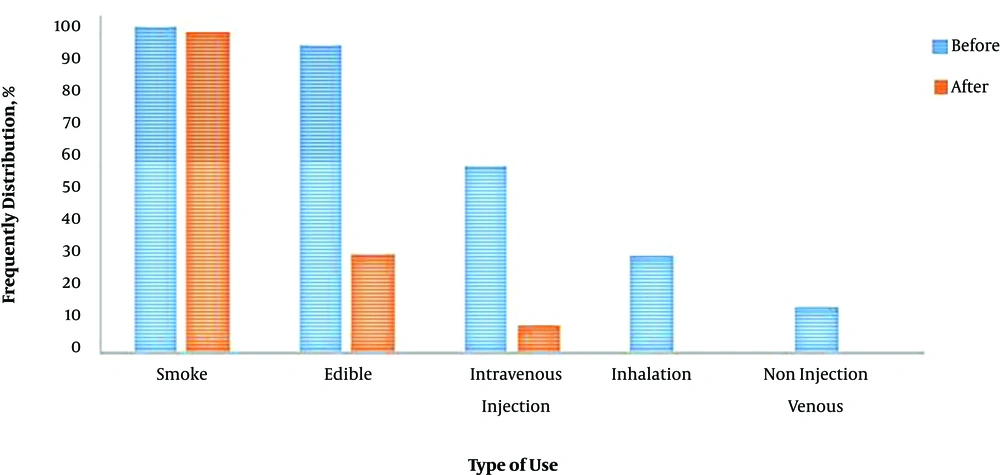
The data about the type of addiction before MMT indicated that 96 (34.9%) participants consumed 15 cigarettes a day. Other drug use consumptions per day were reported as follows: 133 (48.4%) participants consumed 1 g Hashish, 130 (47.3%) participants consumed 1 g opium, 82 (29.8%) participants consumed 1 g heroin, 64 (23.3%) participants consumed opium juice, 33% (12%) participants consumed 1 g amphetamines, 96 (34.9%) participants consumed one sedative tablet, 91 (33.1%) participants consumed 1 of crack, 25 (1.9%) participants consumed three vial, and 82 (29.8%) participants consumed one tramadol tablet. It should be noted that some people were addicted to more than one type of drugs. In general, the distribution of users based on the type of used drugs and the methods of drug use before and after MMT is presented in Figures 1 and 2, respectively. People were treated with methadone for six months. Follow-up results showed that the overall efficacy of MMT was 50.5% so that after six months, 139 patients remained on persistent therapy and did not consume drugs. After MMT, there were no cases of cocaine, grasses, and steroids consumption. Moreover, there was a significant decrease in other drug use (except for smoking) (P < 0.05). No case of non-injection and inhalation use were reported after MMT. Intravenous injection significantly decreased (84.86%) but smoking was still high (98.2%). Oral consumption dropped to 67.5%. Drug reduction rates after MMT were as follows: alcohol consumption, 98.9%; cannabis, 78%, opium, 92%; heroin, 91%; opium juice, 94%; amphetamine, 85%; sedatives, 59%; crack, 87%; Norgesic, 73%; and tramadol, 95%.
Based on the data of the quality of life assessment in addicted people, significant differences were seen before and after MMT in the mean scores of physical health, psychological health, social relationship, and environment domains (P < 0.05) (Table 2). The differences in the scores of physical health, psychological health, social relationship, and environment domains before and after MMT were 14.55, 8.21, 7.15, and 5.6, respectively.
| Domain | Before | After | Difference | P Value |
|---|---|---|---|---|
| Physical health | 49.56 | 64.11 | 14.55 | 0.001 |
| Psychological health | 52.04 | 63.25 | 8.21 | 0.000 |
| Social relationship | 53.71 | 60.89 | 7.15 | 0.003 |
| Environment | 51.12 | 56.72 | 5.6 | 0.001 |
Scores of the Quality of Life at Baseline and Six Months After MMT
The largest mean difference belonged to the physical domain with a mean score improvement of 14.55 while the environment domain had the least improvement (mean difference = 5.6). It should be noted that the highest prevalence of depression was observed in cannabis and opium users. After six months of MMT, the number of people with depression decreased from 236 (85.81%) to 174 (63.27%) (P < 0.05). The mean anxiety score was 39.4 before MMT and 20.41 after MMT, which showed a significant mean difference based on the independent t-test (P < 0.05) (Table 3).
| Severity of Depression | Before | After |
|---|---|---|
| Severe | 22 (8) | 18 (6.54) |
| Moderate | 98 (35.63) | 69 (25.09) |
| Mild | 116 (42.18) | 87 (31.36) |
| None | 39 (14.18) | 101 (36.72) |
Frequency Distribution of Severity of Depression in Patients Referring to the Clinica
5. Discussion
Various studies indicate the effectiveness of MMT centers in reducing the risks of addiction, e.g., to injecting drug use, and its adverse effects related to diseases such as AIDS and hepatitis (14). Considering the lack of a comprehensive study in this regard in Kermanshah province, this study attempted to evaluate the therapeutic effectiveness of MMT in reducing depression, anxiety, and quality of life among addicts.
The results of the study on the demographic characteristics of 275 addicts showed that most addicts were male. This finding is justified by the fact that addicts are more men than women and that women have more secrecy. In other studies, the proportion of men to women has been often high. In the study by Do et al., 98.7% of addicts were men (15). This rate was reported as 100% in the study by Wang et al. (16). Most patients were in the age group of 20 - 30 years. Other studies in the field of addiction also support this finding (8, 16). This can reflect the high prevalence of addiction among young people. Most addicts were unemployed. This result contradicts the study by Raisi Dehkordi et al. showing that most addicts were employed (7) and is in line with the results obtained by Corsi et al. (17). The level of education in addicts can indicate the role of educational barriers in reducing the risk of addiction. Of course, educated people may have less willingness to attend MMT centers. In the study of Dhawan and Chopra in India (18), the quality of life of addicted people was higher in those with high school education but Baharom et al. (19) in Malaysia had 53.3% of those with university education.
Only 1.5% of the addicts did not mention smoking, which could indicate the strong role of smoking in the onset of drug use. The highest percentage of drug addiction in this study was related to opium. In the study by Behdani et al. Crack drug was the most consumed substance (20). However, other studies in Iran showed that opium was the most commonly used drug (7, 21, 22). The proximity to Afghanistan, the world's largest opium producer, has made it easy to distribute opium in Iran. It seems that the high consumption of opium is also justified due to the cultural characteristics of Kermanshah province for the use of opium in parties.
In this study, after being followed up for six months, 139 out of 275 patients remained on persistent treatment and did not consume drugs. Therefore, the efficacy of MMT in this study was 50.5%. The efficacy of MMT was reported as 84% in the study by Wegman et al. (23) and 20% - 60% in the study by Cousins et al. (24). In the study by Chen and Fujiwara in China, one year after the start of MMT, heroin use decreased from 100% to 17.2% and heroin injection decreased from 89.4% to 14.1% (25). The different success rates in relapse prevention are reported in various studies, which is justified by the socioeconomic status of participants, the type of substance, and the period after which a re-examination of addiction is made.
In this study after six months of MMT, intravenous injection ended and no cases of intravenous injection were reported. The success of MMT was very significant regarding high-risk behaviors such as the use of a common syringe in injection drug users as a way of HIV and hepatitis C virus transmission (26). The results of this study showed that MMT could reduce the risk of transmissible diseases in the community.
Depression has a high prevalence among addicts. In this study, depression was the most commonly observed disorder, which is consistent with the results of Goldberg and Lin (27) and Holmes (28) studies. Over a relatively short period, MMT could have beneficial effects on many aspects of the life of addicts by decreasing anxiety and depression and increasing their quality of life. Substance abuse is associated with a low quality of life. In the present study, the quality of life was low before treatment that increased significantly after MMT. In the study by Haj Hosseini and Hashemi (29), MMT could not reduce depression and increase the quality of life of addicts, which contrasts with the current study. However, Peyravi et al. study (30) confirms the results of our study. In this study, mood swings, changes in social relationships, job problems, financial problems, and chronic symptoms of the disease were among the reasons for stress and low quality of life in individuals. In this study, the anxiety reduced after MMT, which is consistent with Baharom et al. study (19). The results of the study indicated the improvement of quality of life in the aspects of physical health, psychological health, social relationships, and environment after MMT. The findings are similar to the studies by Baharom et al. (19), Nordin et al. (31), and Xiao et al. (32). Our results showed that the most improved domain of the quality of life was physical health, followed by psychological health, and social relationship while the least improvement was in the environment domain. These results contrast with Baharom et al. (19) and Huong et al. (31) studies that indicated the psychological health domain had the most improvement and social relationship had the least improvement.
5.1. Conclusions
According to the results, it can be said that MMT could be effective in controlling drug dependence and reducing high-risk sexual behaviors. Employment, education level, and imprisonment history were the factors affecting the duration of MMT, which can be strengthened by accurate and timely planning of experts. A significant improvement was made in the quality of life. MMT is promising in the therapy of opioid addiction, which is still a big public health predicament in Iran. Considering the prevalence of addiction in society, the harmful consequences of high-risk sexual behaviors such as the transmission of infectious diseases including AIDS and hepatitis C, increased depression, and decreased quality life in addicted, the development of MMT centers and the encouragement of addicts to use this type of therapy are recommended.