1. Background
Undoubtedly, the unexpected calamities and disasters are considered as complex phenomena that expand quickly in a manner that destruct rapidly and threaten the strategic and real benefits of society (1). These disasters are mostly uncontrollable phenomena that occur all around the world, including our country, Iran (2, 3). Disasters may occur suddenly or gradually, accompanying economic damages, human losses, and remarkable psychological disorders. Every year, 200 million humans are involved with these disasters and thousands of individuals lose their lives (4). In the 21st century, earthquakes, flood, volcano, deadly storms, and roaring waves, even in developed countries, still take abundant victims (2). In some parts of the world, these disasters are converted to crisis; but, in some other parts, they remain in the extent of the same incident. The difference in consequences should be searched in the human preparedness for fighting and dealing with disasters. If there is no preparedness, the crisis will appear. Therefore, to have a plan to cope with disasters is a vital issue for any organization (5).
When an incident or crisis occurs, the work conditions are changed completely in the health service centers and enforcement of duties becomes difficult. In fact, the health care centers should be prepared to cope with emergencies which may occur at any time. In such conditions, many deaths and side effects emerge and the demand for sudden therapeutic cares increases (2). The health service centers should be accountable to this increase in demand and they should organize their human and support resources to present the necessary services (6). In a study, the preparedness rate of hospitals of Kermanshah University of Medical Sciences in facing with natural disasters was estimated to be 23.8%, which is a warning for this province, as it is vulnerable to natural disasters (7). The health care centers at the time of calamities should have the ability to protect people, especially patients, in a safe condition (structural and non-structural safety) and also present desirable performance (8). These centers should gain the necessary knowledge of the management of natural disasters and carry out strategic planning so that at the time of such incidences can act wisely and play their roles appropriately (9). With regard to the experiences of past disasters, the role and importance of performance, structural and non-structural safety elements have been specified in the uninterrupted serving of health centers. In the meantime, regarding the high costs of non-structural elements, keeping them in a safe condition seems necessary for serving appropriately (10). Dashti city is accounted as one of the catastrophic cities of the country (ruinous flood in 1987 and earthquake of Shonbeh city in 2014).
2. Objectives
This study was designed to study the performance, structural, and non-structural preparedness of health service centers of Dashti city.
3. Methods
In this study, we used a similar approach to examine all health service centers of Dashti city in Bushehr province, which included 30 health houses, 4 health station, 6 comprehensive health service centers, and one hospital. The data collection tool was the standard observational checklist of the world health organization. This checklist was translated by Ardalan et al. and its reliability and validity were estimated at an acceptable extent. This checklist has been compiled and introduced under the name of safety index. This index has 145 indicators of structural, nonstructural, and safety performance and two preliminary parts including the general information of health care centers and the risks that threaten them (11). Table 1 shows the classification of safety.
| Safety Class | Safety Score | |
|---|---|---|
| Max | Min | |
| 10 | 100 | 91 |
| 9 | 90 | 81 |
| 8 | 80 | 71 |
| 7 | 70 | 61 |
| 6 | 60 | 51 |
| 5 | 50 | 41 |
| 4 | 40 | 31 |
| 3 | 30 | 21 |
| 2 | 20 | 11 |
| 1 | 10 | 0 |
Classification of Safety
The risk cognition dimension is divided into three levels based on its score, as follows:
- Level one: Low-risk level
- Level two: Moderate-risk level
- Level three: High-risk level
The scores of the performance, structural, and non-structural dimensions were also divided into three levels:
- Level one: Low safety level
- Level two: Moderate safety level
- Level three: High safety level
After completing the checklist, the data were inserted into Excel software and descriptive statistics (central and distributive indices) were calculated. Then, the data analysis was done.
4. Results
The performance, structural, and non-structural preparedness scores were measured for the health service centers of Dashti city. In terms of performance preparedness, the investigated centers acquired a total score of 39.40. As Table 2 shows, the preparedness level of the centers was poor. In terms of structural preparedness, the health service centers acquired a total score of 77.57. As Table 3 presents, the preparedness level of the investigated health care was good.
| Unit | Performance Preparedness Score |
|---|---|
| House of health | 39.1 |
| Health station | 39.2 |
| Comprehensive health service centers | 39.4 |
| Hospital | 39.8 |
| mean score of performance preparedness | 39.4 |
The Performance Preparedness Level of Health Service Centers in Dashti City
| Unit | Structural Preparedness Score |
|---|---|
| House of health | 73.6 |
| Health station base | 75 |
| Comprehensive health service centers | 71.6 |
| Hospital | 90 |
| Total score of structural preparedness | 77.5 |
The Structural Preparedness Level of Health Service Centers
In terms of non-structural preparedness, the health care centers gained a total score of 56.59. As Table 4 shows, the non-structural preparedness level of the investigated centers was moderate.
| Unit | Non-Structural Preparedness Score |
|---|---|
| House of health | 58.6 |
| Health station base | 55.7 |
| Comprehensive health service centers | 55.0 |
| Hospital | 56.9 |
| Total score of non-structural preparedness | 56.5 |
The Non-Structural Preparedness Level of Investigated Health Service Centers
The overall preparedness level of the investigated centers in terms of performance, structural and non-structural preparedness is presented in Table 5.
| Unit | Overall Preparedness Score |
|---|---|
| House of health | 57.1 |
| Health station base | 56.6 |
| Comprehensive health service centers | 55.3 |
| Hospital | 62.2 |
The Overall Preparedness Level of Health Service Centers
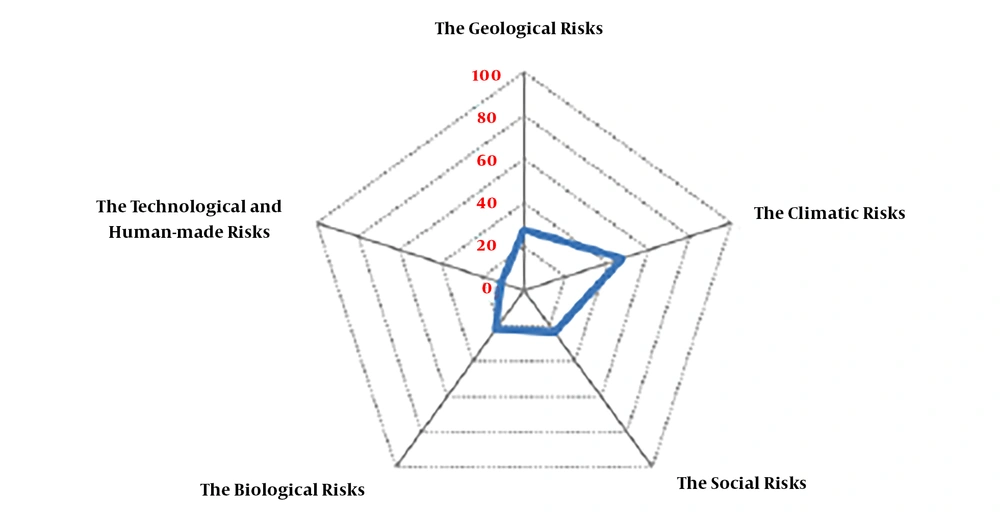
In terms of risks threatening health care centers of Dashti city, the main risk for the centers was related to the climatic factors, as shown in Figure 1. In terms of overall preparedness, the investigated centers gained a total score of 39.40, which showed a weak situation. In terms of structural preparedness, by acquiring a total score of 77.57, they were in a good situation and by acquiring a score of 56.59, they were placed in a moderate level of non-structural preparedness.
5. Discussion
In this study, the preparedness level of health houses with a score of 57.12 rated on safety level 5, which indicated a good preparedness situation. The results are supported by Hojat (8). In the current study, the preparedness rate of health station and centers of comprehensive health services with a score of 50 gained safety level 5, indicating a good preparedness situation. The same results were reported by Hojat (8) and Amiri et al. (12). Also, in the study by Rabeian et al., the most and the least preparedness levels for earthquakes were in the domains of management of unexpected disaster plan and planning for decreasing building dangers, respectively (13). The results of this study showed that the preparedness level of the investigated hospital with a score of 70 gained safety level 8, which showed its good preparedness situation. The results of another study by Amiri et al. showed that two hospitals under study had moderate and low preparedness levels when facing unexpected disasters (12). Barfield et al. reported the vital role of health service personnel’s preparedness in enhancing the quality of health services during the occurrence of natural disasters (14). Hamele et al. stated the need for strategic planning to improve accountability and preparedness of health care services prior to natural disasters (15). Generally, in the domain of structural elements safety, the studied centers had moderate to high preparedness levels that contradicted the results of other studies (4, 16). Although these elements may not have direct effects on the performance of centers, their destruction at the time of natural disasters such as earthquakes can have serious adverse impacts on the efficiency of different parts. The cause of low preparedness in most studies is the lack of sufficient supervision by the related authorities during the construction of health care centers.
5.1. Conclusions
The results of the current study showed that the investigated centers in terms of preparedness were in a poor situation. In terms of structural dimension, due to improvements in two recent years, the investigated centers were in a good preparedness situation; but, in terms of non-structural safety elements, they were placed in a moderate level. Concerning our results, strategic planning and promoting the safety and quality of services are crucial. With regard to the high costs of building repairs, settlement of facilities, equipment, and infrastructural development, it is suggested that, along with developing the appropriate plans for management of disasters, the non-structural and performance of centers be considered as a priority.