1. Background
Lumbar disc herniated is the most common complication that has a poor prognosis after a primary open-ended discectomy. The most common cause of patients who refer to nerve surgery clinics is the back pain that some of them need surgery due to the rupture of the disc. Eighty to 90% of surgical procedures can produce good results for lumbar disc during the first year after surgery (1). Lumbar herniated disc recurrence is the most common complication after initial open-ended discectomy that has a poor prognosis (2). Lumbar herniated disc is defined as a recurrence of leg or foot pain after a definite painless period for at least 6 months after primary surgery (2-5). Lumbar disk recurrence is a major problem in the treatment of herniated disk (6). The actual recurrence rate of the lumbar disc is usually reported between 5% - 15% (7-11). The overall incidence of adverse outcomes is reported to be 5 to 20% after primary lumbar discectomy and herniated recurrence is the main cause of pain, disability and re-surgery (1). The main reason for the recurrence of the lumbar disc is the annular rent that has not been completely settled after the discectomy. Therefore, it allows a weak defect to be exposed to intradiscal mechanical pressure changes. The risk factors for recurrence of lumbar disks have already been reported in various studies and include weakness in circular texture, continuous lifting or vibration, heavy lifting, age, smoking, pre-disk size, disc level and height, and herniated shape during surgery (1, 2, 9, 12-14). Considering the complications of spinal surgery and the patient’s and physician’s concerns about their outcomes, finding a way is mandatory to reduce the need for re-surgical procedures.
2. Objectives
The aim of this study was to determine the risk factors for recurrence and the need for re-surgical repair in patients with lumbar disks referring to Golestan Hospital, Ahvaz as an indicator of further investigation to prevent this complication. This study is based on ecological-environmental, ethnic, tribal, and occupational differences.
3. Methods
This epidemiological and retrospective study was performed on patients who underwent lumbar disc discectomy from Golestan Hospital, Ahvaz between 2011 and 2015. All patients who underwent reoperation following discopathy were studied on the basis of access to the file and the patient himself. Therefore, it was not necessary to determine the sample size and twice the number of people who needed re-surgical treatment were considered normal group. Group 1 included people who re-operated on each side and each level (35 patients) and underwent surgery 6 months ago. The second group consisted of patients (70 patients) who were randomly selected from those that six months have passed since surgery and did not recurrence (normal group).
Patients were selected from those who underwent surgery with the same neurology surgeons. The technique of surgery was not described in this study. MRI imaging was advised for all post-operative patients who experienced persistent pain or back pain relief. Clinically, the herniated disk recurrence is a ruptured disc that causes foot pain and has symptoms in radiography (MRI) and is defined by the disk material at the same side and level of the surgical index that causes impingement, compression, or deviation of the nerve tissue. Patients with herniated recurrence on the other side and the surface were excluded by failure to capture an MRI image, recent cerebrovascular arrest or psychological and cognitive impairment, a history of amputation, severe back arthritis, and neuropathy other than diabetes.
The medical history of all patients was investigated regarding demographic characteristics, including age, sex, height, weight, body mass index (BMI, weight division by height to ability 2), diabetes mellitus, education, marital status, and ethnicity background. In addition, all patients were evaluated for the incidence of associated illness (possibly prone to recurrence), for example, smoking, drinking alcohol, or diabetes. Smoking and working status was obtained from patients’ records before surgery (1). The job variables are classified into three categories: light (office staff and light shopkeeper), medium (housewives and bodybuilders who do not need to carry shipping), and heavy (building workers, factories, squares and taxi drivers).
To describe the data, the mean and standard deviation were used for quantitative variables and frequency and percentage were used in qualitative variables. To analyze the data as mono-variable, independent t-test (Mann-Whitney U test in the absence of assumption of normal data), chi-square test and Fisher’s exact test were used. In order to analyze the data in a multivariate way, variables that had a lack of communication or recurrence of the waist disk were strongly identified in the single-variable analysis section and excluded from the study. To analyze the multivariate data, variables that had a lack of communication or recurrence of the lumbar spine were strongly recognized in the single-variable analysis section and they were excluded from the study. Then, the remaining variables were investigated together using logistic regression. All analyses were performed using SPSS software version 18. The significance level was considered as P < 0.05.
4. Results
There were no lost data in this study and no sample was extracted based on the criteria. Table 1 shows the demographic characteristics of the samples. Age, BMI, smoking, alcohol consumption, marital status, ethnicity, familial history and diabetes were not significantly different between the two groups of recurrence and normal. However, gender, height, weight, occupational status and education variables were significantly different in the normal group.
| Variables | Without Recurrence Group | Recurrence Group | P Value |
|---|---|---|---|
| Quantitative Variables | |||
| Age, y | 42.69 ± 7.06 | 43.29 ± 5.98 | 0.667 |
| Height, cm | 166.01 ± 5.52 | 173.43 ± 6.20 | < 0.001 |
| Weight, kg | 70.76 ± 6.64 | 7.72 (78.06) | < 0.001 |
| BMI, kg/m2 | 25.73 ± 2.60 | 2.15 (25.98) | 0.631 |
| Qualitative Variables | |||
| Gender | 0.038 | ||
| Women | 37 (52.9) | 11 (31.4) | |
| Men | 33 (47.1) | 24 (68.6) | |
| Job status | < 0.001 | ||
| Light | 15 (21.4) | 3 (8.6) | |
| Average | 40 (57.2) | 11 (31.4) | |
| Heavy | 15 (21.4) | 21 (60) | |
| Diabetes | 0.295 | ||
| No | 63 (90) | 29(82.9) | |
| Yes | 7 (10) | 6 (17.1) | |
| Education | 0.035 | ||
| Diploma and under diploma, | 37 (52.9) | 26 (74.3) | |
| Higher than diploma | 33 (47.1) | 9 (25.7) | |
| Smoking | 0.294 | ||
| No | 51 (72.9) | 22 (62.9) | |
| Yes | 19 (27.1) | 13 (37.1) | |
| Alcohol | 0.746 | ||
| No | 67 (95.7) | 33 (94.3) | |
| Yes | 13 (37.1) | 2 (5.7) | |
| Marital Status | 0.605 | ||
| Single | 15 (21.4) | 6 (17.1) | |
| Married | 55 (78.6) | 29 (82.9) | |
| Ethnicity | 0.960 | ||
| Fars | 15 (21.4) | 7 (20) | |
| Arab | 27 (38.6) | 13 (27.1) | |
| Lor | 28 (40) | 15 (42.9) | |
| Family history | 0.746 | ||
| No | 67 (65.7) | 33 (94.2) | |
| Yes | 3 (4.3) | 2 (5.7) | |
The Demographic Characteristics of Single-Variable Analysis in with/Without Recurrence Groupsa
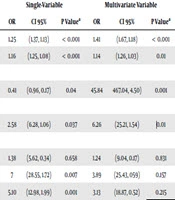
Logistic regression showed that in the absence of other variables, height, weight, sex, education, and occupational status predict lumbar herniated disc recurrence. But in the presence of other variables, height, weight, sex and education predict the recurrence of lumbar disc herniated. The chance of recurrence of the disk in women is 0.41 times than men. In other words, the incidence of lumbar disc recurrence in men is 45.2 times than women. But the chance of recurrence of the lumbar disk in women is 84.44 times than men in the presence of other variables. Consequently, in the presence of other variables, there was a statistically significant relationship between gender variable and recurrence of the lower back disks, but there was an inverse relationship completely rather than the previous state. In the previous state, the chance of recurrence was lower in women than men, but the incidence of recurrence in women was more than men in the presence of other variables (Table 2).
| Variables | Single-Variable | Multivariate Variable | ||||
|---|---|---|---|---|---|---|
| OR | CI 95% | P Valuea | OR | CI 95% | P Valuea | |
| Height | 1.25 | (1.37, 1.13) | < 0.001 | 1.41 | (1.67, 1.18) | < 0.001 |
| Weight | 1.16 | (1.25, 1.08) | < 0.001 | 1.14 | (1.26, 1.03) | 0.01 |
| Gender | ||||||
| Women/men | 0.41 | (0.96, 0.17) | 0.04 | 45.84 | 467.04, 4.50) | 0.001 |
| Education | ||||||
| Under diploma and diploma/higher than diploma | 2.58 | (6.28, 1.06) | 0.037 | 6.26 | (25.21, 1.54) | 0.01 |
| Occupation | ||||||
| Average/light | 1.38 | (5.62, 0.34) | 0.658 | 1.24 | (9.04, 0.17) | 0.831 |
| Heavy/light | 7 | (28.55, 1.72) | 0.007 | 3.89 | (25.43, 059) | 0.157 |
| Heavy/average | 5.10 | (12.98, 1.99) | 0.001 | 3.13 | (18.87, 0.52) | 0.215 |
The Comparison of Multivariate and Single-Variable Analytical Results
5. Discussion
The need for spinal cord recurrence is much more difficult due to uncertain anatomical levels and scars around the nerves than early surgery (5). The rate of re-surgery has been reported in the study of El Shazly et al. (5) who have reported poor results for patients who have undergone re-operation. The aim of this study was to investigate the risk factors for re-surgical need in patients with lumbar discs. The results of this study showed that height, gender (male), weight gain, lower education than diploma and heavyweight and jobs could predict lumbar disc herniated recurrence. However, there was no significant difference between the two groups in terms of age, BMI, diabetes, smoking, alcohol consumption, marital status, ethnicity, and familial history. In this regard, Shimia et al. (1) reported that gender (male), height, heavy work and smoking are predictive of lumbar disc herniated.
In the present study, the recurrence rate of lumbar herniated disc was higher in men than women. However, this completely reverse relationship was seen more in women than men in multivariate analysis. There was no significant difference in age between the two groups with recurrence and no recurrence. There are several risk factors for recurrence of a herniated disc. In some studies, age differences (15, 16) and gender (1) have been reported as a risk factor for recurrence of the herniated disc while other studies reported that age and gender did not relate to a higher recurrence rate (17-20). There was no significant difference in age and gender between the groups with and without recurrence which open microdiscectomy was performed in re-operation (21-23). Unlike the current study, Keskimaki et al. (15) reported that there was a significant difference in gender but patients older than 50 had a higher risk of re-surgical treatment than younger people.
Studies have shown that higher BMI and overweight have a significant relationship with lumbar herniated disc recurrence (16, 17). In the present study, weight gain and height were the predictors of lumbar herniated disc, but BMI was not significantly different between the two groups with recurrence and no recurrence. Similar to the current study, Shimia et al. (1) also reported that height and weight gain were associated with recurrence of lumbar herniated disc, but BMI had no significant correlation between diabetes and lumbar disc recurrence (1). In studies of Hakkinen et al. (18) and Kara et al. (20), BMI did not correlate with lumbar disk recurrence. Moliterno et al. (24) study showed that lacking of individuals’ overweight with lower BMIs are riskier for lumbar discs.
In this study, there was no significant correlation between smoking and lumbar discs. According to the current study, smoking had no significant relationship with lumbar disk recurrence in several studies (17, 20, 22). Unlike this study, Kim et al. (2) and Shimia et al. (1) reported that smoking has a significant relationship with lumbar herniated disc.
This study did not show a significant correlation with lumbar disk recurrence in the statistical population. Similar to our study, Kim et al. (2) and Shimia et al. (1) has been reported that there is no significant relationship between diabetes and recurrence of lumbar disc herniated. Contrary to our study, Mobbs et al. (25) have shown that recurrence of lumbar disc herniated is more common in patients with diabetes.
The results of this study showed that heavyweight and jobs could predict the recurrence of lumbar disc herniated. In the study of Shimia et al. (1), manual work, including continuous lifting or vibration is a predictor of recurrence lumbar herniated disc. Kara et al. (20) reported that the lack of continuous physical exercise was a predictor of lumbar disk recurrence while the job does not relate to the recurrence of a lumbar disc. In Meredith et al. (17), study, manual work did not have a significant relationship with lumbar disc recurrence.
Our study showed that there is a significant relationship between education of two groups with and without recurrence, and the rate of recurrence in people with higher education is lower than the diploma. Education can also predict lumbar discoloration. Contrary to the current study, Shimia et al. (1) did not show a significant difference between two groups of recurrence and no recurrence. The number of different samples can be attributed to this difference in the present study and Shimia et al. (1). One of the limitations of this study was the small sample size of the lumbar herniated disc group. Therefore, the risk information of lumbar herniated disc recurrence factors should be considered cautiously.
5.1. Conclusions
The results of this study showed that height, gender (male), weight gain, lower education than diploma, heavyweight and jobs could predict lumbar herniated disc recurrence. However, there was no significant difference between the two groups in terms of age, BMI, diabetes, smoking, alcohol consumption, marital status, ethnicity, and familial history.