1. Introduction
The global spread of the coronavirus disease 2019 (COVID-19), as a highly infectious disease, have been affected thousands people in all of the world (1, 2). This infection has led to the death of more people than severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS), although it has a lower fatality rate. In Iran, the ongoing COVID-19 epidemic was first reported in Qom. It is important to note that due to the COVID-19 epidemic in Iran, the number of patients, referred to our gastroenterology clinics in Shahid Beheshti Hospital, had increased by 20% (3). After the first report of this infection in Iran, all clinical evaluations, as well as treatment and clinical outcomes of patients with laboratory-confirmed COVID-19, were recorded.
Considering the increasing number of patients referred to gastroenterology clinics and reports of some therapy-resistant pure gastrointestinal (GI) symptoms, we suspected a case of COVID-19 in one of our patients. It should be mentioned that we encounter a large number of patients with only GI symptoms, whereas in this case report, we only documented one case, referred to our gastroenterology clinic. Some important questions need to be addressed promptly to determine whether pure GI symptoms appear without the incidence of respiratory disorder in confirmed COVID-19 patients. The answer to these questions may lead to the effective management of the disease before affecting and transferring of SARS-CoV-2 to heath people who were in close contact with infected patients with pure GI symptoms. With this background in mind, we aimed to collect and analyze the detailed clinical features and chest computed tomography (CT) scans of an old male patient with an only GI disorder without respiratory involvement.
2. Case Presentation
A 74-year-old man was referred to our gastroenterology clinic with complaints of abdominal pain, diarrhea, vomiting, and chest pain for two weeks. He did not report any coughing, dyspnea, or respiratory disorders. His medical history indicated diabetic hypertension. He also avoided smoking and drinking.
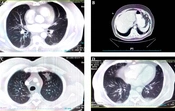
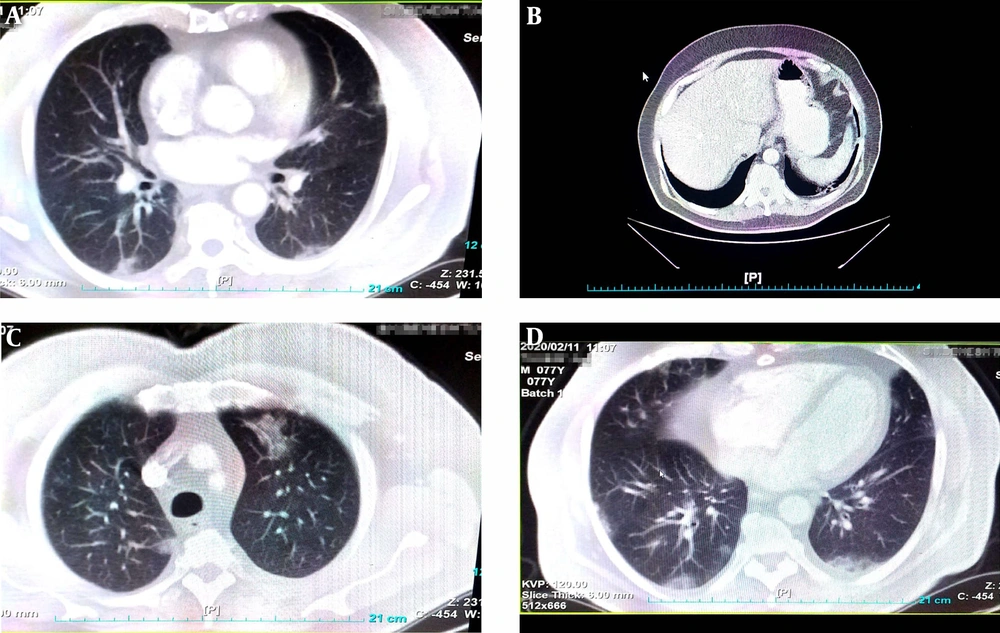
Upon admission to the hospital, he looked ill, and his vital signs were as follows: blood pressure: 110/60 mmHg; pulse rate: 79 bpm; respiratory rate: 16 bpm; and oral temperature: 38°C. The patient had a medical history of diabetes and hypertension. After one week of hospitalization, he presented with fever and sweating. For a better examination, laboratory tests were performed; the results are summarized in Table 1. The CBC test revealed the increased level of WBC and the decreased level of RBC. The serum levels of alkaline phosphatase and amylase were in the normal range. Also, endoscopy and colonoscopy did not indicate any abnormalities. With regard to the increasing prevalence of laboratory-confirmed COVID pneumonia (based on conventional PCR assay and sequencing of PCR amplicons using a throat swab) and dyspnea, in addition to the results of physical examinations and laboratory tests, we performed a chest CT scan due to its high diagnostic value, high accuracy (low false-negative rate), and time efficiency (4). The chest CT scan revealed small bilateral peripheral consolidations with ground-glass opacity and a crazy paving pattern (Figure 1).
| Test, Unit | Result | Reference Range |
|---|---|---|
| Blood Biochemistry | ||
| FBS, mg/dL | 109 | 70 - 99; diabetic: > 126 |
| Creatinine, mg/dL | 1.54a | 0.7 - 1.4 |
| Cholesterol, mg/dL | 105 | < 200 |
| Triglycerides, mg/dL | 100 | < 150 |
| HDL, mg/dL | 36 | Low risk: > 60 |
| Total bilirobin, mg/dL | 1.37a | 0.1 - 1.2 |
| Direct bilirobin, mg/dL | 0.36a | 0 - 0.3 |
| Indirect bilirobine, mg/dL | 1.01 | 0 - 1.1 |
| SGOT (AST), U/L | 30 | 11 - 37 |
| SGPT (ALT), U/L | 28 | 13 - 40 |
| Alkaline phosphatase, U/L | 139 | 100 - 460 |
| Amylase serum, U/L | 82 | 0 - 100 |
| Iron (Fe), µg/dL | 89 | 40 - 120 |
| TIBC, µg/dL | 419 | 230 - 440 |
| Hb A1c, % | 6.2 | Non diabetic: 4 - 6; diabetic: > 6.5 |
| Estimated average glucose, mg/dL | 131 | This test is a calculated glucose over the past 2 - 3 months period based on Hb A1c results |
| Serology, Endocrinology and Tumor Marker | ||
| CRP, mg/L | 4.4 | Up to 6 |
| Ferritin, ng/mL | 95.8 | 20 - 250 |
| Total PSA, ng/mL | 0.3 | 0 - 4 |
| AFP (Clia), IU/m | 3.22 | 0 - 4 |
| CEA (Clia), IU/mL | 2.02 | Up to 4.7 |
| Keton | Negative | - |
| Hematology | ||
| WBC, ×103 | 10.70a | 4.1 - 10.5 |
| Neutrophil, % | 53.30 | 43 - 78 |
| Lymphocyte, % | 33.70 | 15 - 45 |
| Monocyte, % | 9.70 | 4 - 9 |
| Eosinophil, % | 3.00 | 1 - 7 |
| Basophil, % | 0.30 | 0.3 - 1.3 |
| Immature granulocyte, % | 0.20 | 0.16 - 0.62 |
| Neutrophil, ×103 | 5.70 | 2 - 7.7 |
| Lymphocyte, ×103 | 3.61 | 1 - 2.7 |
| Monocyte, ×103 | 1.04 | 0.3 - 0.7 |
| Eosinophil, ×103 | 0.32 | 0.2 - 0.6 |
| Basophil, ×103 | 0.03 | 0.01 - 0.3 |
| RBC, 106/µL | 4.31 | 4.5 - 5.9 |
| Hb, g/dL | 13.80 | 13.5 - 17.5 |
| HTC, % | 39.90 | 37 - 53 |
| MCV, fL | 92.6 | 80 - 100 |
| MCH, pg | 32.00 | 26 - 34 |
| MCHC, g/dL | 34.60 | 32 - 36 |
| RDW-CV, % | 13.80 | 11.5 - 16 |
| RDW-SD, fL | 47.10 | 38 - 50 |
| Platelet, 103/µL | 209.00 | 150 - 450 |
| PDW, fL | 13.00 | 9.5 - 15.2 |
| MPV, fL | 10.90 | 9.4 - 12.3 |
| P-LCR, % | 32.70 | 19.4 - 43.7 |
| PCT, % | 0.23 | 0.19 - 0.39 |
| ESR 1 h, mm/h | 21a | 0 - 20 |
| Urine Analysis | ||
| Color | Light yellow | - |
| Appearance | Clear | - |
| Specific gravity | 1.012 | - |
| Osmolarity | 520 | - |
| pH | 5.0 | - |
| Protein | Negative | - |
| Glucose | Negative | - |
| Bilirobine | Negative | - |
| Urobilinogen | Normal | - |
| Keton | Negative | - |
| Nitrite | Negative | - |
| Blood | Negative | - |
| RBC/hpf | 0 - 1 | - |
| WBC/hpf | 1 - 2 | - |
| Squamous epithelial | 1 - 2 | - |
| Bacteria | Negative | - |
| Mucus | Negative | - |
| Casts | Negative | - |
| Crystals | Negative | - |
Abbreviations: AFP, alpha-fetoprotein; ALT, alanine transferase; AST, aspartate amino transferase; CEA, embryonic carcinoma antigen; CRP, C-reactive protein; FBS, fasting blood sugar; Hb A1c, glycosylated hemoglobin; Hb, hemoglobin; LDH, lactate dehydrogenase; TIBC: Total Iron-Binding Capacity; RBC, red blood cell; Total PSA, total prostate specific antigen; WBC, white blood cell.
aHigher in comparison to the reference value.
3. Discussion
In this case report, we described the clinical findings of an old male patient with a GI disorder, who was suspected of COVID-19. After administering medications for one week, he still showed resistance to therapy. We suspected COVID-19, as the onset of outbreak was reported in Iran at the time. For further evaluations, a biochemical assay was carried out; however, it failed to provide more data for a precise diagnosis. Due to the persistence of abdominal pain, as well as nausea resistant to therapy, pelvic and abdominal CT scans, endoscopy, and colonoscopy were performed; nevertheless, the results were in the normal range. The chest CT scan revealed pleural constipation and sub-pleural constipation on the left side of the diaphragm. The patient was isolated in a negative pressure room for two weeks, and without any medications, all of his symptoms subsided (5).
Based on the present results, we should be aware of the possibility of COVID-19 and the progression of pneumonia in patients following the emergence of pure GI symptoms; such awareness may be important in the prognosis of COVID-19 pneumonia (6). Recently, Zou et al. (7), reported that angiotensin-converting enzyme 2 (ACE2) is the main associate receptor of SARS-CoV-2 and the spike (S) protein of 2019-nCoV had a high affinity to ACE-2, which mediate the virus entrance to the target cell, causing the final infection. It has been demonstrated that ACE2 receptors can be expressed in the oral cavity and are abundantly found in epithelial cells. The overexpression of ACE2 receptors has also been indicated in the colon, intestines, and gallbladder. Therefore, with notice to this point that the viral mutations may occur during transmission, associated clinical features of SARS-CoV-2 during its spread is welcome.
According to the epidemiological findings reported by Lai et al. (8), fever was the most common symptom among adult patients (92.8%; n = 258), followed by cough (69.8%; n = 194), dyspnea (34.5%; n = 96), myalgia (27.7%; n = 77), headache (7.2%; n = 20), and diarrhea (6.1%; n = 17) (3, 8). Nevertheless, our observations were only related to a single case, whereas a larger number of patients suspected of COVID-19 are referred to our gastroenterology clinics. Therefore, we need more time to evaluate new confirmed cases of COVID-19. Precise recording of all GI symptoms and interpretation of the findings should also be addressed in new patients. Recording all clinical symptoms, as well as, GI follow-up studies in patients with the COVID-19, is not without merit and can be a great help in timely diagnosis and treatment of the disease.