1. Background
New unknown pneumonia was reported from Wuhan, China, at the end of 2019 (1, 2). The etiology was known to be a coronavirus family member, named Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). It spread around the world very soon. On March 11, 2020, the World Health Organisation (WHO) declared this global health emergency a pandemic (3, 4).
The severity of COVID-19 symptoms can range from very mild to severe, and some people may show no symptoms. Healthcare Workers (HCWs) are one of the high-risk groups who are exposed to COVID-19 (5). Many reports from different countries show the outbreak of COVID-19 among HCWs (6-8). Infection in hospital staff is a big challenge, as it reduces the capacity of the health system and increases secondary transmission (9). Thus, it seems that the early detection of infected hospital staff is crucial to prevent the transmission of the virus to other employees and patients and maintain their stable workforce at optimum performance.
Typically, seroconversion occurs 11 to 14 days after the first symptoms (10). According to various studies, the overall seroprevalence of COVID-19 in HCWs is low. Based on data from Santa Clara state of USA (11), Germany (8), and Dutch hospitals (12), the rates of SARS-CoV-2 IgG antibody were 1.5, 4.5, and 6%, respectively. However, another study from the United Kingdom revealed that the rate was higher (18%) (13). The Real-Time Reverse Transcription Polymerase Chain Reaction (RT-PCR) in respiratory samples was introduced as the gold standard COVID-19 diagnostic test (14) and is a sensitive and accurate way to confirm the diagnosis of SARS-CoV-2 infection in practice (15). However, this test takes a long time (an average of two to three hours) to get the result and requires certified laboratories, expensive equipment, and trained technicians.
Most importantly, several false-negative results have been reported for RT-PCR of COVID-19 (14) that can lead to a major problem in the diagnosis and controlling of virus transmission (16). To identify a large number of symptomatic and asymptomatic infected patients quickly, an accurate and rapid testing method is needed (15). Serological tests can be helpful (17). These tests allow experts to know what proportion of the population has been involved, and assess their types of involvement (symptomatic or asymptomatic) and the probability of spreading the virus without being aware of it (18). Also, it helps estimate how many people are at risk. On the other hand, in workplaces, serology detection can help get a decision on who can return to work safely, especially for healthcare workers, provided that high-quality tests are used.
2. Objectives
At Mofid children's hospital, based on unpublished data, 36 of 800 employees became infected within two months of the COVID-19 epidemic. No data is available for asymptomatic cases because we did not conduct periodic surveillance by PCR in our hospital. As children can be silent carriers or mild non-specific symptom presenters, the HCWs in children's hospitals may be at higher risk of infection in contact with apparently asymptomatic cases, causing a neglected risk. This study aimed at determining the antibodies (IgM and IgG) against SARS-COV-2 in Mofid children's hospital staff to define the rate of seropositivity.
3. Methods
3.1. Specimens Collection, Preparation, and Testing
This cross-sectional study was performed in April 2020 in a referral pediatric subspecialty tertiary center in Tehran (the capital of Iran). From Mofid children's hospital, 475 staff participated in the study. The inclusion criteria included all Mofid children's hospital staff who were presented in the period of this study. The COVID-19 IgG/IgM antibodies were detected by Rapid Test Dipstick (Hangzhou AllTest Biotech Co. INCP-401, China). Rapid serological tests provide a means to quickly diagnose COVID-19-suspected cases by detecting IgG and IgM antibodies in blood samples. The participant's finger was punctured by a lancet, and the blood was applied to the test card by using a capillary tube. Then, 20 μl of blood and one drop of buffer were added to the test card, and we waited for the colored line(s) to appear. The result was interpreted by the company instructions based on three lines of color (Control, IgG, and IgM). All the tests were performed under strict biosafety conditions. Informed consent was obtained from all participants in this study. The sensitivity, specificity, and accuracy of COVID-19 IgG/IgM antibodies according to the manufacturer's instructions are shown in Table 1.
Sensitivity, Specificity, and Accuracy of COVID-19 IgG/IgM Rapid Test Kits
3.2. Statistical Analyses
Statistical analyses were performed using SPSS software, version 25. Simple and multiple logistic regressions were used to analyze the relationship between risk factors and the disease. P values of less than 0.05 were considered statistically significant.
4. Results
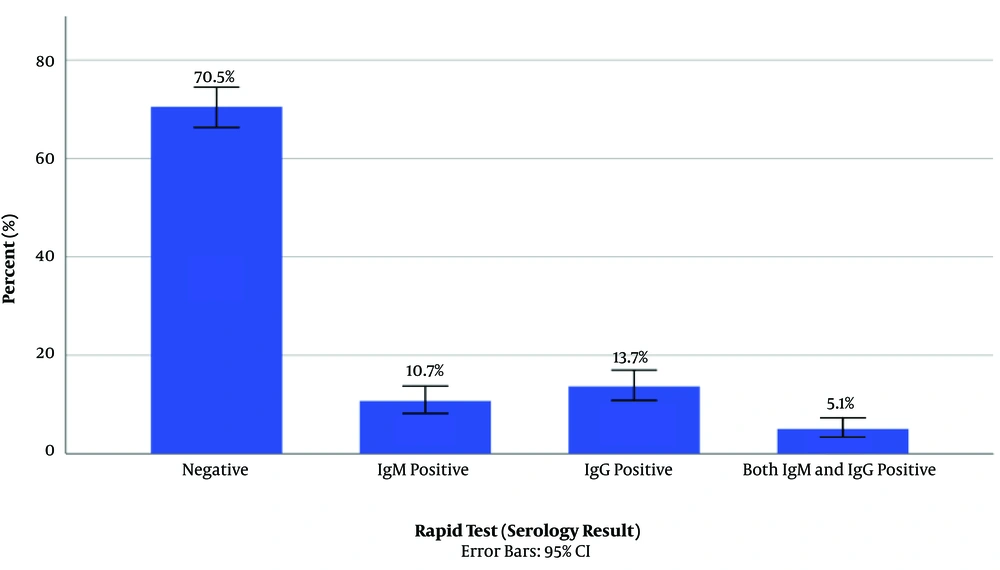
Of 475 staff participating in the study, 387 were female, and 97 were male. The demographic data of the participants by serological results and the relationship between individual independent variables and COVID-19 serology results are presented in Table 2. A total of 140 (29.4%) staff were infected with COVID-19 based on serologic tests, including 115/140 health care workers, 13 office workers, and 12 hospital service workers. Among 140 seropositive cases, 52 were asymptomatic, 83 were symptomatic, and five had severe symptoms who were hospitalized. Besides, 51 (10.7%) and 65 (13.7%) cases had positive IgM and IgG antibodies, respectively. Also, 24 (5%) cases had both IgG and IgM positive results (Figure 1). To investigate the effect of family crowding, we divided the sample based on the number of family members into two groups of < 4 and > 4 persons. The results showed that 66 (47.14%) cases with positive serology belonged to the group of < 4 persons, and 74 (52.86%) cases belonged to the group of > 4 persons (P value = 0.06). Besides, 25 (5.26%) staff had a history of confirmed COVID-19 by CT scan (16 cases) or PCR (nine cases), of whom 21 (84%) were positive (3 IgM+, 10 IgG+, 8 both of them) and four (16%) were seronegative.
| Variable | Positive Serology | OR | 95%CI | P Value | |
|---|---|---|---|---|---|
| Negative (n=335) | Positive IgM, IgG, or both (n=140) | ||||
| Education level | |||||
| Diploma | 62 (71.26%) | 25 (28.74%) | Ref. | ||
| BSc | 178 (71.77%) | 70 (28.23%) | 0.98 | 0.57 - 1.67 | 0.93 |
| MSc | 31 (62.00%) | 19 (38.00%) | 1.52 | 0.73 - 3.17 | 0.26 |
| Doctorate | 64 (71.11%) | 26 (28.89%) | 1.01 | 0.53 - 1.93 | 0.98 |
| Age group | |||||
| < 40 | 238 (74.84%) | 80 (25.16%) | Ref. | ||
| 40-62 | 97 (61.78%) | 60 (38.22%) | 1.84 | 1.22 - 2.77 | 0.004 |
| Type of service | |||||
| Service | 27 (69.23%) | 12 (30.77%) | Ref. | ||
| Official | 16 (55.17%) | 13 (44.83%) | 1.83 | 0.67 - 4.96 | 0.24 |
| Health/Medical | 292 (71.74%) | 115 (28.26%) | 0.89 | 0.43 - 1.81 | 0.74 |
| Family size | |||||
| 1-3 | 190 (74.22%) | 66 (25.78%) | Ref. | ||
| ≥ 4 | 145 (66.21%) | 74 (33.79%) | 1.47 | 0.99 - 2.18 | 0.06 |
| Used masks | |||||
| N95 | 46 (73.02%) | 17 (26.98%) | Ref. | ||
| Surgery | 218 (68.99%) | 98 (31.01%) | 1.22 | 0.66 - 2.23 | 0.53 |
| Other types | 67 (76.14%) | 21 (23.86%) | 0.85 | 0.40 - 1.78 | 0.66 |
| None | 4 (50.00%) | 4 (50.00%) | 2.71 | 0.61 - 12.05 | 0.19 |
| Body mass index | |||||
| < 24 | 169 (76.47%) | 52 (23.53%) | Ref. | ||
| ≥ 24 | 166 (65.35%) | 88 (34.65%) | 1.72 | 1.15 - 2.58 | 0.008 |
| Contact to persons with COVID-19 | |||||
| No | 135 (70.31%) | 57 (29.69%) | Ref. | ||
| Yes | 200 (70.67%) | 83 (29.33%) | 0.98 | 0.66 - 1.47 | 0.93 |
Demographic Data of Participants by Serological Results and Relationship Between Individual Independent Variables and COVID-19 Serology Results in Hospital Staff
The results of multiple analyses showed that the two variables of BMI and family members had relationships with positive serology. The odds ratio was 1.72 times higher for health workers with a BMI ≥ 24 compared to BMI below 24 (95% confidence interval: 1.17 to 2.57; P value = 0.006) and 1.49 times higher for those with a family of four members or more in comparison with families with three or fewer members (95% confidence interval: 1.01 to 2.20; P value = 0.04). By the elimination of the number of family members, variables that were independently related to positive serology of COVID-19 were BMI and age. It means that the odds ratio is 1.62 times higher in health care workers with BMI ≥ 24 in comparison with ones who had BMI below 24 (95% confidence level: 1.09 to 2.43; P value = 0.02) and 1.52 times higher in health workers ≥ 40-years-old in comparison with ones who were < 40 years (95% confidence interval: 1.01 to 2.30; P value = 0.04). Other variables were not significant in this study.
5. Discussion
Children can be silent carriers or show non-specific mild symptoms. Children are admitted to the hospital for different reasons while they carry viruses. As all hospitalized children stay with their mothers in the wards, people who work in children's hospitals may be at higher risk of being infected by SARS CoV-2. This study aimed to investigate the effect of different variables on the seropositivity of Mofid children's hospital staff in Tehran, Iran. Based on our knowledge, this research was the first large-scale prevalence study on Iranian children's hospital staff during the COVID-19 pandemic. Our results showed that 140 (29.4%) staff were seropositive for IgG, IgM, or both. Other studies from Belgium and the USA showed rates of 6.4% and 1.5%, respectively, which were lower than our result (11, 19). In a study conducted at a pediatric and woman hospital in Germany, 1.8% were serologically positive (20). The high rate of antibodies among our staff may be due to some reasons. First of all, the epidemic of COVID-19 started in Iran sooner than in Europe and the USA. As our study was conducted four months after the epidemic onset, our population had more time to being infected more. Second, it may be related to the lack of compulsory quarantine in our country compared to other countries.
This study was done in a children's hospital where patients were admitted because of different complaints and stayed with their parents who might be carriers of the virus. Also, at the first stages of the epidemic, according to the data from Wuhan, it seemed that the rate of infection in children is low; so HCWs in children hospitals did not follow the protocols carefully. As 51 of our cases were IgM positive, it may show that they were infected recently, and their immune system started responding to the virus. Besides, 65 cases were IgG positive; this antibody indicates that they may have acquired COVID-19 before. Similar to the results of our study, other studies have shown that age has a significant role in the incidence of the disease (21-23).
Our findings showed that the risk of seropositivity was not different between staff who were working in administrative departments of the hospital and those working as health care or service workers. In contrast, a study from Wuhan showed that the number of HCWs with COVID-19 was significantly lower in office buildings than in clinical wards (24). A higher rate of seroconversion in our study than in Lai et al. study from Wuhan may show that our staff in different parts of the hospital did not appropriately follow protocols because the risk of contact and working with children was not clear as an important risk factor for them. Thus, we think awareness and education have important roles in better protection. The number of family members in our study did not correlate with seropositivity. Unlike our results, Song et al. reported that close contact and even casual contact with family members increased the risk of COVID-19 transmission (25).
Although most of the participants announced that they were wearing masks, positive serological tests for 140 (29.4%) cases represented that they had not used proper protection during the epidemic, and still, we need more education. Based on another study, a high BMI was a risk factor for the severity of COVID-19 (26). Although we did not compare the seropositivity rate between high and normal BMI people because of limited cases, our results showed that staff with high BMI were more seropositive than normal BMI people. Based on this data, a high BMI can be a risk factor for getting the disease. Besides, 245 participants announced contact with COVID-19 cases in the hospital, 174 (71%) of whom were seronegative. Thus, in this study, having contact with COVID-19 cases was not statistically effective. Our findings are also in line with Fusco et al.'s study in Naples and Korth et al.'s study in Germany that reported 1.6% seropositivity in HCWs (8, 27). The low rate of seropositivity in these staff may be related to some reasons. First, based on the data, only eight participants did not use masks or appropriate personal preventive equipment during the epidemic. Second, it was not confirmed which participants exactly had contact with suspected and probable COVID-19 cases.
Of 230 people who did not appear to have specific contact with patients, 57 (24.7%) had positive serology. Ningxia et al. and Gandhi et al. confirmed that asymptomatic COVID-19 infection is possible, and our data again confirmed that the sources of infection can be asymptomatic or may have mild symptoms (28, 29). This study had some limitations. Because of the pandemic situation, only 60% of the hospital staff were presented at the time of the survey. We did not conduct PCR testing in this study because of limited resources. Thus, we considered negative serology equal to not dealing with COVID-19. However, we know it may happen in the current infection, and even it may change to negative in cured cases.
5.1. Conclusions
In summary, the serological test of the staff from a tertiary children's hospital in Iran had 29.4% positivity after four months of starting the COVID-19 epidemic, which was higher than the rate in the general population at the time of the study. It could be an alarming sign to insist on continuous education on using PPE and other necessary preventive protocols and being aware of asymptomatic carriers.