1. Introduction
Rat bite fever (RBF) is a disease caused by either Streptobacillus moniliformis or the spirochete Spirillum minus (1). Streptobacillus moniliformis is prevalent in North America and very rare in Asia (2). Streptobacillus moniliformis colonizes the mouth cavity and nasopharynx of 50 - 100% of rodents (1). It is also found in gerbils, guinea pigs, and squirrels. Rat bite fever results from direct bites from rodents or via consumption of contaminated milk or food (1). The majority of patients with the disease have a history of bite or interaction with rodents. Here, we describe a relatively rare case of S. moniliformis-associated bacteremia without a rodent bite. For cases without a bite or contact history, diagnosis is based on microbiological testing. In the present case, the patient presented with high fever and multiple joint swelling and pain that decreased the patient’s range of motion after influenza vaccination in the upper left arm. Although reactive arthritis was initially suspected, the patient was correctly diagnosed with rat bite fever after blood culture analysis.
2. Case Presentation
A 77-year-old Chinese woman was admitted to the rheumatology and immunology department of Jinhua Hospital of Zhejiang University on 21 October 2021. The patient complained of having multiple joint swelling, pain, decreased range of motion, and fever for more than 10 days, which were more pronounced at night. A discussion of recent events leading to the patient’s current condition revealed that she had an acute onset of swelling and pain of the left shoulder joint and fever after receiving an influenza vaccination in the upper left arm. She first visited Yongkang City First People’s Hospital but her symptoms did not improve after infusion treatment. Unfortunately, the treatment she received was not clear before she coming to our hospital. At Yongkang Hospital, Laboratory tests confirmed increased C-reactive protein (CRP) (44.05 mg/L) and a white blood cell count (WBC) of 10.32 × 109/L per liter. Urinalysis revealed hematuria (126/μL). For further examination and treatment, she visited the outpatient department of our hospital where chest CT examination found no abnormality. On admission, she presented with fever of 38.5°C, a respiratory rate of 18 breaths/min, blood pressure of 145/81 mmHg, and heart rate of 74 beats/min.
Laboratory tests confirmed increased C-reactive protein (CRP) (17.83 mg/L), platelet (PLT) count (299 × 109/L), neutrophils levels accounting for 86.1% of the white blood cell (WBC) count of 13.1 × 109/L. Other laboratory results were: serum albumin (Alb, 31.3 g/L), hemoglobin (128 g/L), a serum creatine (CR, 60.3 μmol/L), serum total bilirubin (TB, 9.3 μmol/L), alanine aminotransferase (ALT, 109.0 U/L), aspartate aminotransferase (AST, 78.0 U/L), and sedimentation rate of 30 mm/h.). Urine analysis revealed mild erythrocyturia (25/μL). However, anti-CCP antibody, rheumatoid factor, anti-streptococcal hemolysin O, PR3-ANCA and MPO-ANCA were negative, while antinuclear antibody was positive.
The patient was a professional farmer in Yongkang. At physical examination, she was conscious and had normal cardiac, pulmonary, and abdominal findings. No rash, morning stiffness, frequent and urgent urination, cough and sputum, chest tightness, abdominal pain and diarrhea, difficulty in turning over, or fearless chills were observed. The patient had no history of smoking, regular alcohol consumption, or animal rearing. In addition, she reported no history of allergy to inhaled substances, foods or drugs. At her first day in the hospital, the patient was initially diagnosed with reactive arthritis with liver dysfunction and osteoporosis.
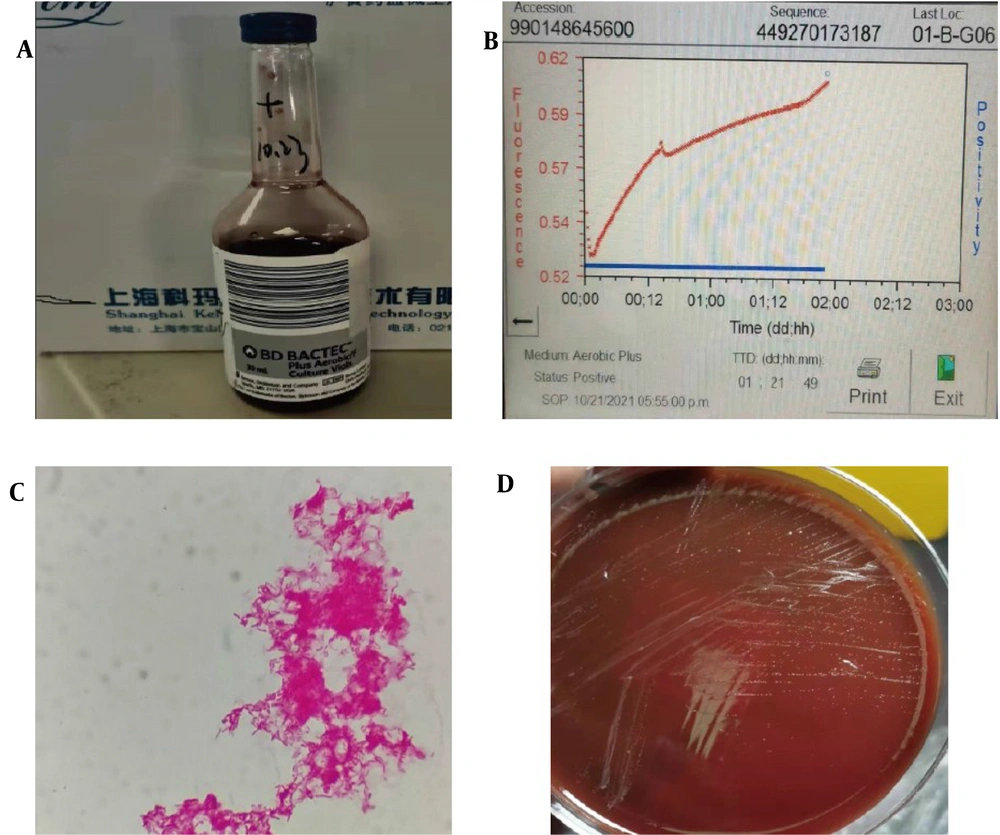
At present, it was considered as reactive arthritis first, and it was necessary to be vigilant in differentiating infection-related arthritis, rheumatoid arthritis and tumor-related arthritis. Since the patient’s condition was severe, she was admitted to the rheumatology and immunology department where two sets of blood cultures were obtained and bacterial culture done using the BACTEC FX blood culture system (Becton Dickinson Microbiology Systems, Sparks, BD, USA) (Figure 1A). In the meantime, empirical anti-inflammatory and analgesic treatment was started using oral loxolprofen sodium at 60 mg every 8 h. Adjuvant treatments were initiated using compound glycyrrhizin tablets and omeprazole enteric-soluble capsules for liver and stomach protection, respectively. Symptomatic supportive treatments combined with treatment for osteoporosis were also given.
On the third day, Gram-negative bacilli were isolated from a single aerobic blood culture bottle after 46h of incubation (Figure 1B). Gram staining revealed gram-negative rods (Figure 1C). The sample was then sub-cultured at 35°C on Columbia blood plate, chocolate plate, and MacConkey agar plate in a capnophilic atmosphere containing 5% CO2. Ceftriaxone sodium was given empirically using an intravenous drip injection at 2 g once daily were given to prevent infection.
Loxolophen (60.0 mg every 8 h) was given for inflammation and pain relief but it was not effective. Thus, we switched to Betamethasone sodium phosphate injection (1.0 mL every 3d) on the 3rd day of hospital stay. On the 4th day, we observed growth on Columbia blood plate and obtained a colony of about 1 mm in diameter three days later (Figure 1D). Using the MALDI-TOF MS system (Biotyper system (Bruker Daltonik, Germany), we identified the bacteria as S. moniliformis at a score of 2.25 on the same day. we did not perform antimicrobial susceptibility testing of this strain. After multidisciplinary consultation with infectious diseases specialists and medical microbiologists, the diagnosis of RBF caused by S. moniliformis was made. Empirical ceftriaxone treatment was subsequently changed to intravenous penicillin G 4800,000 IU three times daily.
In order to discover the etiology of infection, we re-interviewed the patient. On interviewing the patient, she was not aware of any bites or scratches but she owned one dog and handled contaminated dog feces and urine. She may have had contact with contaminated food or water at her house in Yongkang, Zhejiang province, China. She responded very well to Penicillin G treatment. However, although fever was controlled, joint swelling and pain did not improve. Thus, we switched the Betamethasone sodium phosphate injection (1.0 mL every 3d) to an intravenous infusion of methylprednisolone (20.0 mg every 24h) on the 7th day in hospital. Within a few days, the patient was afebrile and her arthritis symptoms improved gradually.
On the 12th day, she underwent echocardiography which found no symptoms of endocarditis. Moreover, blood cultures were repeated which did not detect any microorganism. On the 14th day, the patient could be discharged home with oral doxycycline (100 mg every 12 h) in good clinical condition. At the time of discharge, the patient’s joint pain and swelling had improved markedly and her WBC count (5.95 × 109/L), CRP level (< 0.5 mg/L), ALT level (28.6 U/L), AST level (32.0 U/L) and sedimentation rate (16.0 mm/h) had returned to normal. At one and four weeks after discharge, the patient should be seen for follow-up, but she never came to our hospital again. She was found to have made a full recovery in a telephone interview at three months after discharge.
3. Discussion
To the best of our knowledge, this is the first case of documented RBF without a rodent bite in mainland China. Clinically, RBF is a rare zoonotic disease caused by S. moniliformis or Spirillum minus (1, 3, 4). Patients with condition often experience sudden and intermittently relapsing fever, skin lesions and arthritis (5). RBF has non-specific manifestations, including fever (92%), rash (61%), polyarthralgia (66%), vomiting (40%) and headache (34%) (1). RBF is a low incidence of the disease with non-specific symptoms, as for this clinicist make a direct clinical diagnosis virtually impossible. In our review of case reports on RBF infections, we found in most cases accurate diagnostic delays caused up to seven days of significant delays to the initiating pathogen-specific therapy (6). More than 50% of patients with RBF develop migratory polyarthralgias, involving the small and large joints of the extremities (1) and may also be accompanied by septic arthritis (7). The prognosis of RBF is favorable when pathogen-specific therapy is timely given. However, in cases of severe complication it has a mortality rate of 7 - 13% (8). RBF-associated endocarditis accounts for up to 53% of mortality due to infectious endocarditis (9).
Streptobacillus moniliformis, is a filamentous, non-acid-fast, and highly pleomorphic, nonmotile rod bacterium (10). Streptobacillus moniliformis is an extremely fastidious organism that requires specific culture medium supplemented with 10 - 30% serum or blood and microaerophilic conditions to grow. Furthermore, the bacteria grow slowly, all for these makes microbiological diagnosis difficult (11). Based upon literature review, we found that S. moniliformis infection has been reported in individuals handling pets, living in poor regions, working in research laboratories, and most cases were identified by 16S-rRNA sequencing (2, 12, 13).
In the present case, no antibiotics had been administered before blood culture. Fortunately, S. moniliformis was identified from blood cultures, allowing for precise and successful treatment. Bloodstream infection (BSI) is a major public health burden, with high mortality worldwide. Blood culture is the most important etiological method for diagnosing bloodstream infection and requires blood sampling prior to antibiotic administration. Unfortunately, blood culture tests might not be a sufficiently reliable diagnostic method, microbial culture failure rates of up to 33% (6). As a result, more rapid and definitive diagnosis method are highly anticipated.
There are several options to accelerate identification of clinical pathogens from clinical samples: on the one hand, MALDI-TOF MS can be performed from positive blood culture bottles without subcultures on the agar plate, on the other hand, specific multiplex PCR diagnostic testing directly from clinical samples is being developed (14). Particularly, Meta-next generation sequencing (mNGS) is a last resort pathogen identification tool to address infectious disease problems, performing well in identifying novel, rare, fastidious and coinfected causative organism directly from clinical samples (15).
An in-depth interview with the patient indicated that she had no history of any bites or scratches. The patient owned one dog and handled contaminated dog urine and feces, making this the most likely etiology of infection. Furthermore, reported cases without a bite history were up to 34 %. (6, 13, 16).Thus, we considered the possibility that she was infected through exposure to contaminated food or water. In a previous report, an outbreak of S. moniliformis blood stream infections was reported at a boarding school and led to the conclusion that it was transmitted through water that had been contaminated by rats (17). Here, although the patient reported no history of rat bite, we identified S. moniliformis infection based on blood cultures and patient presentation. Penicillin G (400,000 - 600,000 IU/day, for 7 - 14 days in adults) is the first-choice antibiotic for the treatment of suspected RBF (2). Treatment is generally given in the absence of complications. Doxycycline, ceftriaxone and erythromycin are recommended for patients with penicillin allergy. In line with other physicians, we opted to begin a cephalosporin-based empirical therapy with Intravenous Ceftriaxone (6, 18, 19), and we adhered to the recommended treatment of penicillin G (19), after knowing the causative organism of RBF. However, continuation of a cephalosporin administration might be acceptable given the rare antibiotic resistance in Streptobacillus moniliformis (18).
The MALDI-TOF MS technique can provide accurate detection of bacterial infection. It is faster, convenient, cheaper, and accurate compared to traditional technique of biochemical identification tools. As shown in the present case, this method accurately identified S. moniliformis. In our review of recent case report on RBF infections, we found most cases were identified by 16S-rRNA sequencing (2, 6, 11). The pathogen was not confirmed by sequencing analyses in the present case, which may be a limitation in the present case. We used corticosteroids to suppress immune response due to the severe pain and swelling in the joints. However, lack of standardized use guide (6), the role of corticosteroids in RBF treatment needs further investigation in future cases.
3.1. Conclusions
This is the first case of RBF caused by S. moniliformis without a rat bite to be reported in China. The method of pathogen identification and successful treatment reported here can be used as a reference strategy. This case emphasizes that for more effective blood culture tests, blood culture specimens should be collected before antibiotic administration and highlights MALDI-TOF MS, a new microbial detection method, as an excellent tool for bacterial identification. However, identify the causative organism of RBF by blood culture may sometimes fail to provide physicians with the timely and definitive diagnosis that would allow initiation of rapid pathogen-specific therapy. Hence, we recommend (1) Physicians should consider the possibility of RBF and obtain a complete zoonotic exposure history when considering potential causes of unexplained fever, arthralgia and rashes, (2) antibiotic empirical coverage of gram-negative bacteria with cephalosporins, such as Ceftriaxone, until pathogen-specific therapy becomes available upon microbiological confirmation, and (3) the laboratory medical microbiologists should be consulted by the clinicians, if there is a suspicion of a relatively rare infectious disease with a fastidious bacteria.