1. Background
Although breast cancers are thought to be highly related to viruses, different researchers have presented controversial results (1). Breast cancer is a multi-stage disease and infection with DNA viruses may be contributing for some stages (1, 2). The DNA viruses may be oncogenic in many cancers such as Hepatitis B virus in hepatocellular carcinoma, Epstein-Barr virus (EBV) in lymphoma, nasopharyngeal cancer, and langerhans cell histiocytosis, as well as Human papilloma virus (HPV) in cervical cancer (1-3). Oncogenic viruses are contributing to 20% of human cancers. EBV, Human herpes virus type 8 (HHV-8), cytomegalovirus (CMV), HPV, and Herpes simplex virus-1 (HSV) were detected in breast malignant tissues by PCR (2).
Epstein-Barr virus from the Herpesviridae family has shown significant association with sporadic breast cancer cases and it has been suggested to be associated with the total survival rate (1) due to the presence of genes of this virus in breast tumoral tissues, however, not in normal tissues. Epstein-Barr virus may be not involved directly in breast carcinogenesis and may be the cause of cellular behavioral alteration to invasive patterns leading to the hypothesis that EBV is more common in breast cancers with negative receptors and higher grades (4). If convincing evidence for a carcinogenic role of these viruses in breast can be built up, there is a chance of primary prevention (4). Regarding controversies regarding the etiological role of EBV in development of breast cancer (5-11), this study was performed to detect the presence of EBV-DNA in breast tumors and show if there is any association of EBV virus and breast cancer in Iranian patients.
2. Objectives
The previous studies on this subject are limited in Iran. Early diagnosis and treatment of EBV, could be taken into consideration in the management of breast carcinoma. Therefore, we looked for EBV- DNA in the tumors of Iranian women diagnosed with breast cancer.
3. Methods
3.1. Ethics Statement
Our patients were anonymous and the information extracted from the pathology reports is unchanged. The study protocol was approved by the Shahid Beheshti University of Medical Sciences ethic committee (SBMU.REC.1393.192).
3.2. Patients and Controls
The samples of 75 breast carcinomas used in this study were formalin fixed as well as paraffin-embedded and were diagnosed by the pathologist in 1 of the referral centers (pathobiology laboratory center) in Tehran, Iran, between 2005 and 2014. The criteria of diagnosis were taken from the related pathology textbooks. The slides were reexamined under the light microscope and adequate tumor samples were selected for the study. The criterion of exclusion was a small sized tumor. All cases were Iranian with a mean age of 48.2 years. For the control group, 75 non-tumoral tissue samples (reduction mastectomy, fibrocystic change (FCC), FCC and sclerosing adenosis, as well as FCC and focal adenomatoid change, ductal ectasia, and fat necrosis) were selected (2005 - 2014) from the files of the same department. Absence of malignancy was the criterion of inclusion.
3.3. Tissue Preparation and DNA Extraction
The embedding material should completely be removed from the 5 µm-thick-tissue samples prepared from paraffin-embedded blocks before DNA extraction. Xylene and alcohol were employed to deparaffinize the tissues and rehydrate, followed by tissue lysis using tissue lysis buffer and proteinase K. To extract DNA from lysed tissue, instructions of the company was followed (RTP® DNA/ RNA Virus Mini Kit procedure; Stratec Molecular GmbH, Berlin, Germany) and the nucleic acids were frozen at -20°C.
3.4. Polymerase Chain Reaction (PCR)
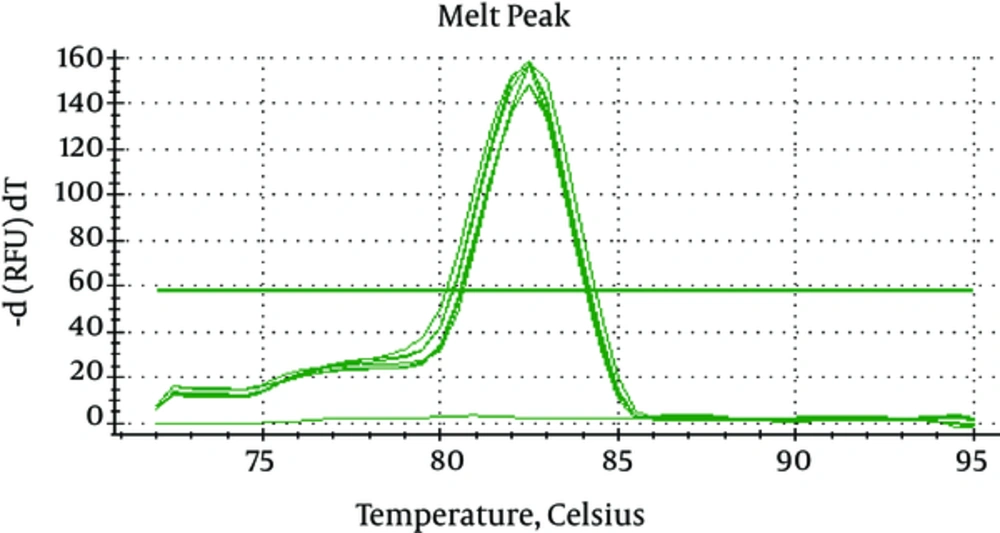
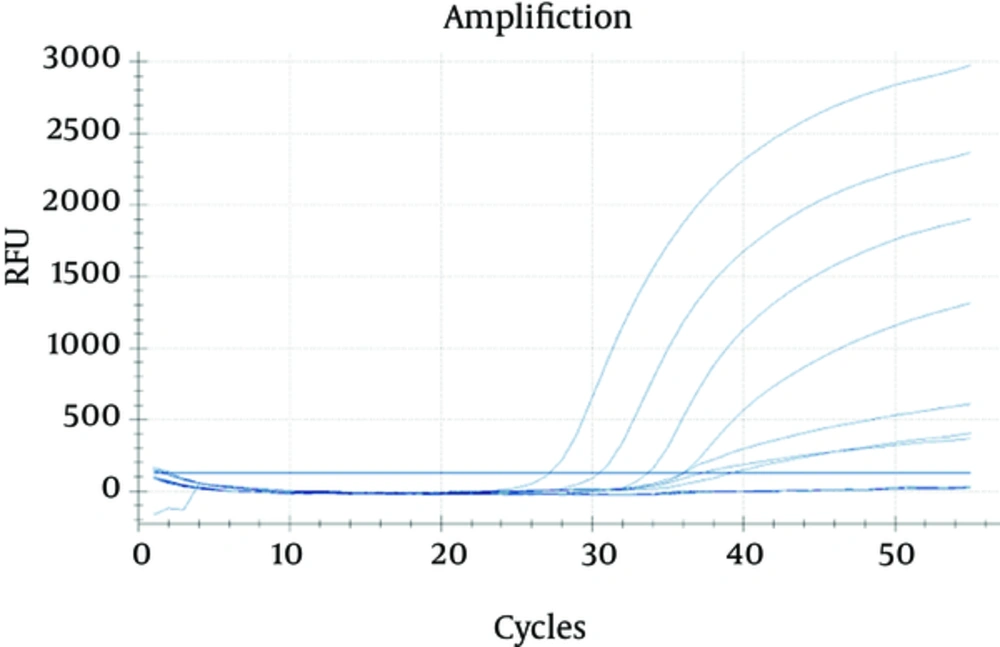
The quality control of the extracted DNA was done by using the Sybr green real-time PCR-Melting curve for beta globin gene using GH20 primer; GAAGAGCCAAGGACAGGTAC and PCO4 primer; CAACTTCATCCACGTTCACC (Figure 1). The Thermo ScientificTM MaximaTM SYBRTM Green 2X qPCR master mix and 10 pmol per reaction of the GH20/PCO4 primers were used to conduct the quality control (Figure 1). To preform RT- PCR, BamH1W EBV sequence primer sets was used. It amplifies 84 bp gene region of the EBV genome (ebv-f; 5’-GCAGCCGCCCAGTCTCT-3’), ebv-r; 5’- ACAGACAGTGCACAGGAGCCT-3’). The internal probe was ebv-p; 5’-FAM- AAAAGCTGGCGCCCTTGCCTG-BHQ1-3’ (12). Reaction volumes of 20 μL underwent amplification as follows: 1) sample denaturation at 94°C for 10 minutes, 2) 10 second denaturation at 94°C, 3) annealing and extension at 60°C (1 minute, 50 cycles) (Figure 2). CFX-96 RT-PCR System (BIO-Rad, USA) was employed and the reagent was HS prime taq premix taqman (GENETBIO, Korea). Serial dilutions of AmpliRun® EBV DNA CONTROL (Vircell, Spain) was used to detect the limit of 15 copies of EBV genome per reaction.The respective r2 values generated by the standard curves were 0.996. The quality of the assays, in terms of efficiency, was 93.1%.
3.5. Statistical Analysis
To perform the analysis, Chi-Square or Fisher’s exact test was used. Statistical significance was a P value of less than 0.05.
4. Results
The mean age in malignant cases was 48.2 ± 10.8 years. The malignant tumors were medullary carcinoma, tubular carcinoma, invasive lobular carcinoma (ILC), and invasive duct carcinoma (IDC) in 1.33%, 1.33%, 9.33%, and 88%, respectively. The malignant lesions were right-sided in 49.3% and left-sided in 50.7%. The mean age in the control group was 38.9 years and 76% of lesions were right-sided. The control group included fibrocystic changes in 57.3%, fatty breast tissue in 25.3%, ductal ectasia in 1.3%, and other types in 16% of cases. As shown in Table 1, the EBV was found in 7 cases (9.3%) of malignant lesions and 0% of benign lesions showing statistically significant difference according to Fisher test (P = 0.014), the odds ratio was 0.907 (CI95%: 0.843 - 0.975). Table 2 demonstrates EBV presence rate based on the type of lesions. Age, tumor laterality, and pathological type of the tumors were not related to the presence of EBV in malignant cases (P > 0.05).
| Type | Positive | Negative | Total |
|---|---|---|---|
| Malignant | 7 (9.3%) | 68 (90.7%) | 75 (100%) |
| Benign | 0 (0%) | 75 (100%) | 75 (100%) |
| Total | 7 (4.7%) | 143 (95.3%) | 150 (100%) |
EBV Presence Rate in Malignant and Benign Lesions in Our Study
| Pathological Type | EBV | Total | |||
|---|---|---|---|---|---|
| Pos | Neg | ||||
| Malignant | Type | IDC | 7 (10.6) | 59 (89.4) | 66 (100.0) |
| ILC | 0 (0) | 7 (100.0) | 7 (100.0) | ||
| Tubular | 0 (0) | 1 (100.0) | 1 (100.0) | ||
| Medullary carcinoma | 0 (0) | 1 (100.0) | 1 (100.0) | ||
| Total | 7 (9.3) | 68 (90.7) | 75 (100.0) | ||
| Benign | Type | Others | 12 (100.0) | 12 (100.0) | |
| FCC | 43 (100.0) | 43 (100.0) | |||
| Fatty breast tissue | 19 (100.0) | 19 (100.0) | |||
| Ductal ectasia | 1 (100.0) | 1 (100.0) | |||
| Total | 75 (100.0) | 75 (100.0) | |||
EBV Presence Rate Based on the Type of Lesions
5. Discussion
Many researchers have been fascinated for decades by the hypothesis that a virus may cause human breast cancer. The link of hormone-responsive viruses with breast cancers cannot be excluded (HPV, mouse mammary tumor virus (MMTV) and EBV are the major candidates) and EBV is expressed in up to 50% of breast tumors by several researches (1, 4). In our study, EBV was detected in 9% of malignant lesions with no positivity in benign lesions or normal breast, showing statistically significant difference according to Fisher test.
Different studies have shown viruses in cells lines, in addition to their contribution to some breast tumors. The review article by Hsu et al. (1) reported that HPV, EBV, CMV, HSV-1, and HHV-8 may be contributing to breast cancer. The study by Lawson and colleagues (4) suggested the association between EBV and breast cancer. Tsai et al. (2) assessed 127 subjects in 2 groups of case and control and it was seen that HHV-8 and EBV were related to malignant status of lesions. Mazouni et al. (8) reported that 65 out of 196 breast cancer cases had EBV-DNA by RT-PCR, which was related to worse pathology subtype. Preciado and colleagues (11) showed presence of EBV in breast carcinoma with 35% positivity (using immunohistochemistry (IHC) in 69 breast carcinomas) as well as 31% positive results (using PCR in 39 breast carcinomas) and zero rate for 48 control groups, however, there was no significant association between EBV expression and worse clinical or pathologic characteristics. They used the IHC method for EBV-encoded nuclear antigen 1 (EBNA-1) and the positive results were approved with PCR.
In Mohamed’s research (9), the EBV positive rate was 35.3% and they proposed a possible association between this virus and breast malignancy. Zekri et al. (13) assessed 90 Egyptian and Iraqi women with breast cancer and showed a 45% (Egyptian) and 28% (Iraqi) positive rate of EBV-DNA in malignant cases compared to none of benign cases, showing a significant difference. No statistically significant difference between EBV presence and tumor grade was reported in either population. The methods used included In situ hybridization (ISH) for EBV-specific RNA (EBER) and IHC for CD21 as well as PCR. The meta analysis performed by Huo and colleagues (6) in 2012, on researches using the PCR technique for detecting the EBV, including 24 studies and 1535 cases (1993 - 2008), showed EBV infection in 29.32% of the women with malignant breast tumors. The highest prevalence (35.25%) was in Asian patients and the lowest (18.27%) in Americans. Statistically, the strongest connection of EBV was with lobular carcinoma.
Glenn et al. (14) used the situ PCR method and reported that 68% and 35% of cases with breast cancer and control breastfeeding women had EBV-DNA. They also identified high risk HPV in 50% and MMTV sequences in 78% of 50 invasive breast cancer specimens. More than 1 virus was detected in 72% of samples of the same breast carcinoma and in 13% of the same milk samples. They concluded that these viruses are probably related to a higher tumor grade and young age. The study by Richardson et al. (15), using both quantitative PCR and determination of serum immunoglobulin level for EBV and CMV, also reported significant difference between malignant and benign tissues in 70 subjects. Their review of the literature and the meta-analysis of all the results of PCR studies performed on breast carcinoma regarding CMV and EBV, raised the following possibilities: 1, these analyses have limitations and cannot confirm whether the viruses are associated with breast cancer; however, using ISH in addition to PCR may increase the sensitivity; 2, the virus may be absent after development of the tumor (‘hit and run’ oncogenesis), causing contradictory results; 3, one or more viruses could be responsible for induction of breast carcinoma at a later period; 4, the possibility of breast carcinoma could be increased by infection with multiple viruses; 5, none of the virus has a role in cancer development.
On the contrary to the positive reports, Perrigoue et al. (10) reported no significant association between EBV and breast cancer in 45 cases by RT- PCR and ISH. Joshi et al. (7), in their review of the literature in 2012, concluded that the data in the publications reviewed do not defend a conclusion that MMTV-like sequences, HPV, or EBV have an etiologic role in breast cancer. The 3 previous studies performed in Iran (Table 3) showed no significant positive results; Eghbali and colleagues (5) had a higher but statistically insignificant rate of HBV-DNA in malignant cases using the PCR technique. Kadivar et al. (16) reported that EBNA-1 and LMP-1 were negative in all 100 breast carcinoma cases and control subjects, which were approved by the PCR method. Also, the study by Fadavi et al. (17), using PCR and RT-PCR, showed negative EBV-DNA in 18 breast cancers. The false positive results may be due to contamination, infected circulating lymphocytes, cross-reaction of antibodies or use of ISH, which determines the virus with qualitative but not quantitative method. The negative results may be due to geographical differences and various distribution patterns of virus, low amount of the virus, and low sensitivity of used techniques (16). Also, some techniques may not distinguish between viruses in tumoral cells and those in tissue lymphocytes (16, 17).
Results of Previous Studies in Iran (Breast ca. and EBV)
5.1. Conclusion
According to our results and review of other studies in the literature, it can be concluded that EBV may have an etiologic role in breast cancer. No significant association between pathological subtype and EBV-DNA presence was identified in our study. Although the presence of a virus alone does not establish a causal role in the disease and other techniques are not used to prove the attendance of EBV- DNA in tumor cells, our findings with 9.3% positivity, in addition to the previously reported positive results, supports the possibility of an etiologic relationship. The proof of etiologic role of EBV in the induction of breast carcinoma needs more efforts using more specific and sensitive techniques (1, 2, 16, 17). If the association of one or more of these viruses with breast cancer can be established, there is a possibility of prevention by anti-viral treatments and vaccination strategies (11). Limitations in our study included unavailability of IHC and ISH for EBV and absence of EBV serologic test results.