1. Background
Human brucellosis, or Malta fever, was first recognized in Malta in the 1850s. It is caused by bacteria belonging to the genus Brucella, of which the most relevant species to livestock animal health and public health are Brucella abortus, B. melitensis, B. ovis, and B. suis (1, 2). Brucellosis, as a zoonotic disease, is transmitted from animals to humans. Humans contract brucellosis when their skin (especially skin with cuts) or nasopharyngeal mucous tissues/membrane come in contact with infected animals' materials such as abortion materials, fetuses, placental materials, vaginal discharges, urine, and manure (1, 3). Humans are also infected after consuming unpasteurized milk and milk products and improperly cooked meat from infected animals (4, 5).
According to WHO, about 500 000 new human brucellosis cases are reported yearly (6). In humans, the bacteria infect reproductive tissues, lymph nodes, and the spleen and cause inflammation, edema, and necrosis. In pregnant animals, it causes placental lesions and increases the risks of abortion (1, 3). Patients usually present with nonspecific symptoms, including undulant fever, chills, profuse sweating, headache, bone pain, weight loss, and myalgia. Although human brucellosis is not lethal in most cases, in lack of proper treatment and chronicity of the disease, it can lead to severe complications such as arthritis, osteomyelitis, spondylitis, endocarditis, and neurological involvement (7, 8).
Proper diagnosis is one of the key obstacles to completely eradicating brucellosis. Although several serological tests, such as the Rose Bengal tube test, Serum Agglutination test, and enzyme-linked immunosorbent assay (ELISA), are used for disease diagnosis; however, these are often found to be misleading (7). Blood culture is a gold standard for Brucella investigation, but this method is time-consuming and elevates the risk of disease transmission. Also, it orders a high level of skill and safety parameters. Serological screening methods detection, such as the Rose Bengal, are commonly conducted in diagnostic laboratories (8-10). Recently, polymerase chain reaction (PCR)-based and serological tests have been widely used to ensure proper diagnoses. In addition to public health risks, late diagnosis and treatment of brucellosis raise financial concerns for livestock stakeholders or latent product consumption and health care cost. Real-time PCR can detect a very low level of bacteria in a sample and is widely used to diagnose infectious diseases (11-14).
2. Objectives
Our study aimed to evaluate the PCR method in patients with suspected brucellosis and compare it with serological tests.
3. Methods
This descriptive cross-sectional study was performed on 90 febrile patients with clinical features of brucellosis who were examined by an infectious disease specialist.
3.1. Blood Sample and Data Collection
A blood sample (10 mL) was taken from each patient and sent to the laboratory. The Rose Bengal test screened all specimens. Of the 90 samples, 45 turned out to be positive, and the other 45 were negative. Serum separation and serological tests were performed using standard techniques and commercially available antigens. DNA extraction and bacterial target gene fragment amplification were performed by PCR. We evaluated all 90 samples for Rose Bengal and PCR, and each method's results were recorded and compared. Serum separated by centrifugation at a speed of 3000 rpm for 5 minutes. Then, sera were transferred to 1.5 mL vials for serological tests and stored at –70°C until the serological test (Rose Bengal test) was performed.
3.2. DNA Extraction and PCR Protocol
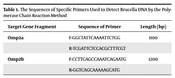
A DNA extraction kit (Thermo Fisher Scientific Co, Waltham, Massachusetts, United States) was used to isolate the DNA. The extracted DNA was stored at –20°C until storage, and 4 μL of the extracted DNA was used for PCR. In this study, omp2a and omp2b fragments were extracted from DNA and examined by molecular PCR (Table 1). The BLAST software was used due to the Specificity of primers for the target sequence in the genome of Brucella bacteria and check the homology of the sequence of the primers with the genetically registered sequences (https://blast.ncbi.nlm.nih.gov/Blast.cgi).The amplification of omp2aF fragments was performed using the 3-GGCTATTCAAAATTCTGG-5 sequence, and 3-ATCGATTCTCCACGCTTTCGT-5 was used for omp2aR with a length of 1100 base pairs (bp). The amplification of omp2aF fragments was performed using the 5-CCTTCAGCCAAATCAGAATG3-3 sequence, and 5-GGTCAGCAAAAAGCATG-3 was used for omp2aR with a length of 1200 bp (15).
| Target Gene Fragment | Sequence of Primer | Length (bp) |
|---|---|---|
| Omp2a | F-GGCTATTCAAAATTCTGG | 1100 |
| R-TCGATTCTCCACGCTTTCGT | ||
| Omp2b | F-CCTTCAGCCAAATCAGAATG | 1200 |
| R-GGTCAGCAAAAAGCATG |
Abbreviation: bp, base pair.
To amplify selected fragments in a 50 μL portion, we used PCR 10x buffer that contained 0.2mM dNTP mix, 1μM of each primer of omp2aF, omp2aR, omp2bF, and omp2bR, 1 unit of Taq DNA polymerase, and 75200 ng of DNA (16). We put the samples in a thermocycling device; then, we set the following thermal profile for the device: primary denaturation (95°C for 5 minutes), final denaturation (95°C for 1 minute), annealing (58°C for 2 minutes), primary extension (70°C for 3 minutes), and final extension (70°C for 10 minutes). The PCR products were combined with 1.5% agarose gel and 0.5x TBE solution for electrophoresis. Then, we saw the bundle patterns in the duct gel device after the samples were colored with ethidium bromide. All samples from the serological test with brucellosis symptoms were analyzed by the PCR method with a sensitivity of 90% and an error of 10% (17, 18).
4. Results
Of the 90 blood samples, the number of positive cases of Rose Bengal was 45, and the other 45 were negative. We did the PCR technique using omp2a and omp2b primers with lengths of 1100 and 1200 bp on gel electrophoresis in all 90 samples (Table 2). We found that all serology-positive patients had positive PCR results. However, 40 out of 45 patients had a positive PCR test in serology-negative patients (Tables 3 and 4). According to this study, the sensitivity of PCR in diagnosing human brucellosis with the serology-positive test is 100%, and with the negative serology test is 88.9%. Therefore, it is higher than the overall sensitivity of the serology test in all patients, which was 50% in our study.
| Target Gene Fragment | Positive | Negative | Total |
|---|---|---|---|
| Omp2a | 40 | 5 | 45 |
| Omp2b | 40 | 5 | 45 |
| Serological Test Outcome | Frequency | Percent | Valid Percent | Cumulative Percent | |
|---|---|---|---|---|---|
| Valid | Positive | 45 | 50.0 | 50.0 | 50.0 |
| Negative | 45 | 50.0 | 50.0 | 100.0 | |
| Total | 90 | 100.0 | 100.0 |
| Serological Test Result | PCR Test Result | Frequency | Percent | Valid Percent | Cumulative Percent |
|---|---|---|---|---|---|
| Positive | Positive | 45 | 100.0 | 100.0 | 100.0 |
| Negative | 0 | 0.0 | 0.0 | 0.0 | |
| Total | 45 | 100.0 | 100.0 | ||
| Negative | Positive | 40 | 88.9 | 88.9 | 88.9 |
| Negative | 5 | 11.1 | 11.1 | 100.0 | |
| Total | 45 | 100.0 | 100.0 |
Abbreviation: PCR, polymerase chain reaction.
5. Discussion
According to Lai et al. (19), brucellosis is a common infectious disease that has the highest prevalence in Africa and Asia. The National Brucellosis Prevention and Control Plan (NBPCP) reported that since 2020 and during the COVID-19 pandemic, a lack of attention to the prevention and treatment of brucellosis guidelines during the pandemic has increased the incidence of human brucellosis and its severe complications. Symptoms vary but generally include headache, heavy sweating, body pain, fatigue, and weight loss. Due to its nonspecific symptoms, its diagnosis may be delayed, causing the disease to change from acute to chronic. The chronicity of the disease leads to the aggravation of the infection and its complications, including cardiovascular and hepatobiliary problems. Sometimes, severe cases can lead to disability or the patient's death. This issue highlights the importance of using rapid diagnostic methods with high accuracy to detect human brucellosis (19-21).
In our study, we entered 90 patients with highly suspected human brucellosis. First, we did the serological test on their samples. As a result, 45 samples were negative, and 45 were positive. Then, we did the PCR test for all samples. We found that all serology-positive patients had positive PCR results. However, 40 out of 45 patients had a positive PCR test in serology-negative patients. Our findings suggest that PCR's sensitivity in diagnosing human brucellosis with the serology-positive test is 100%, and the negative serology test is 88.9%. Therefore, it is higher than the overall sensitivity of the serology test in all patients, which was 50% in our study. In line with our study, Rahbarnia et al. found that out of 120 patients, 55% had a positive serological test, and 50% had a positive PCR test. Of the 66 patients with positive serological tests for brucellosis, 49 tested positive for PCR (22-25).
According to the management of human brucellosis guidelines, when we suspect a patient of having brucellosis, we must confirm our diagnosis with laboratory tests. However, due to the low sensitivity of the serological tests in the early stage, cross-reaction with other bacterial species, the prozone effect, and low-affinity antibodies, after a few weeks, when antibodies level reached the diagnostic threshold in suspected seronegative patients, serological tests should be repeated (18, 21, 22). With this method, treatment in serology-negative patients is delayed for weeks, and as a consequence, these patients encounter more complications from untreated brucellosis than serology-positive patients do (20, 23). To minimize the diagnostic time and reduce the complications in serology-negative patients, we decided to compare the PCR method as a faster solution to diagnose definite brucellosis.
Most studies have shown that standard PCR appeared to be a more sensitive technique than serological methods, not only for diagnosing the first episode of infection but also for the early detection of relapses (26, 27). Differences in the sensitivity and specificity of PCR samples in studies can be due to differences in PCR kits, the disease stage, and the method of DNA extraction from serum or whole blood samples of patients. False negatives in the PCR sample can be attributed to technical errors, the inefficiency of the chemicals used, low DNA content in the serum sample, and previous use of antibiotics (17, 28-30). The current study showed that the PCR method has high accuracy, specificity, and sensitivity, promoting the importance of using this method as a reliable early diagnostic test in human brucellosis, especially in suspected patients with seronegative tests.
5.1. Conclusions
Brucellosis is an infectious disease with various signs and symptoms. Early detection of brucellosis can prevent complications and its burden. PCR tests can be used as a rapid and sensitive diagnostic method in patients living in endemic areas of brucellosis. It is a suitable method for detecting patients with suspected brucellosis. With this method, treatment is started faster, and the risks of complications will be reduced.