1. Introduction
Klebsiella pneumoniae is one of the most common pathogens (1, 2) and is often isolated from various specimens in the inpatient (3), especially in those immunosuppressed patients, such as cancer patients (4). However, the report of K. pneumoniae in the intestine invading into the blood is rare. Here we report a case of multi-site infections caused by K. pneumoniae after hemopoietic stem cell transplantation, which was first isolated from the stool, then the blood, the sanies, the throat swab, and the urine.
2. Case Presentation
A 22-year-old girl with complete remission after chemotherapy for her acute lymphoblastic leukemia was referred to our hospital for hemopoietic stem cell transplantation on March 22, 2016. On the presentation, her temperature was 36.8°C, blood pressure was 125/93 mmHg and her heart rate as well as respiration were 93/min and 19/min, respectively. She received a good check-up, although, she wasn't in good spirit. Her primitive lymphocyte (0.06%) and total lymphocyte (27.05%) in the peripheral blood were in the normal range. Sulfamethoxazole was used to clean her intestine. BuCy and Flu were used to pretreat the bone marrow before receiving hemopoietic stem cell transplantation on April 5, 2016. Ciclosporin and mycophenolate mofetil were used for preventing a reject reaction.
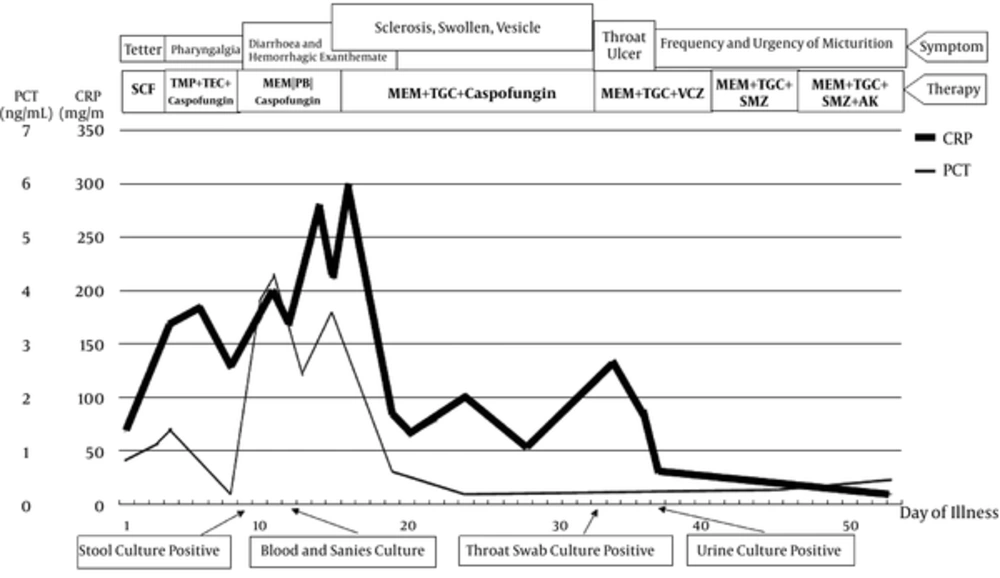
She received a 224 mL stem cell transfusion, including a mononuclear cell (4.87 × 108/kg), CD34+ (0.6%), as well as reached the transplantation threshold of CD34+ cell (3 × 106/kg). Nine days after transplantation, there were no severe side effects except a little bit of vomit. However, diarrhea and hemorrhagic exanthemate of both knees appeared April 15, 2016 and a 3 cm × 2 cm sclerosis appeared on the right greater lip of pudendum. The right greater and lesser lip of pudendum were swollen 1 day later on April 16, 2016. The inspection results, clinical symptoms, and prescriptions were collected (Figure 1). The isolates were collected from the stool culture on April 15, 2016, the blood culture as well as sanies culture on April 18, 2016, the throat swab culture on May 9, 2016, and the urine culture on May 13, 2016 were all the same bacterium (K. pneumoniae).
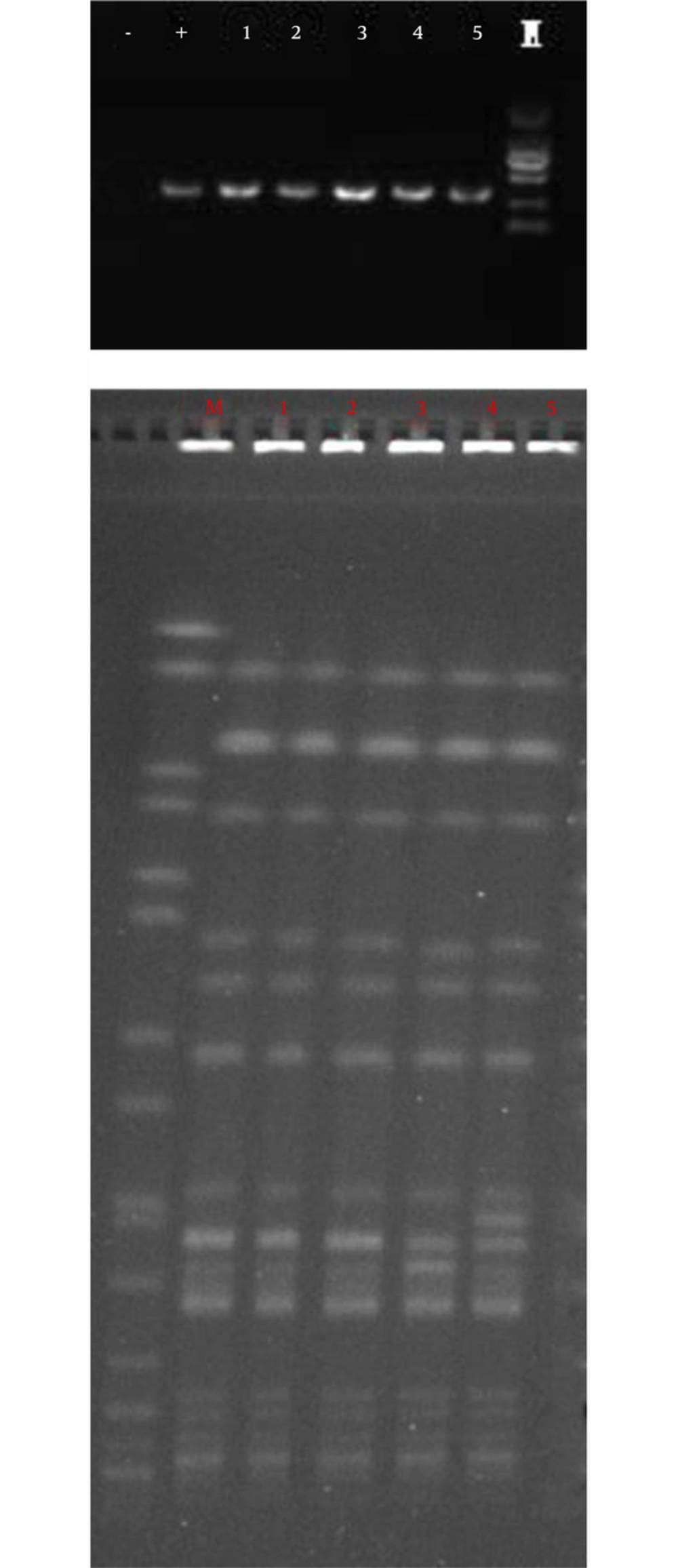
The antibiotics susceptibility against 5 K. pneumoniae strains were the same (Table 1). The K. pneumoniae was resistant to all antibiotics that we tested except polymyxin B and tigecycline, as it was called carbapenem-resistant K. pneumonia. In addition we detected the resistant genes of carbapenem by PCR (5) and DNA sequence. They were all positive for the blaKPC gene (Figure 2A) and negative for blaSME, blaVIM, blaIMP, blaNDM, blaGIM, blaSPM, blaSIM, and blaOXA genes (data not shown). The resistant gene was blaKPC-2 by sequencing. Pulsed field gel electrophoresis (PFGE) (6) demonstrated that the 5 K. pneumoniae isolates belonged to the same clone (Figure 2B).
| Antibiotics | MIC, μg/mL |
|---|---|
| Ampicillin | ≥ 32 |
| Cefazolin | ≥ 64 |
| Gentamicin | ≥ 16 |
| Tobramycin | ≥ 16 |
| Cefepime | ≥ 64 |
| Ceftriaxone | ≥ 64 |
| Cefoxitin | ≥ 64 |
| Imipenem | ≥ 16 |
| Ertapenem | ≥ 8 |
| Amikacin | ≥ 64 |
| Ciprofloxacin | ≥ 4 |
| Levofloxacin | ≥ 8 |
| Trimethoprim/sulfamethoxazole | ≥ 16/304 |
| Amoxicillin/clavulanate | ≥ 32/16 |
| Piperacillin/tazobactam | ≥ 128/4 |
| Tigecycline | 2 |
| Aztreonam | ≥ 64 |
| Polymyxin B | 0.5 |
A, PCR of blaKPC Gene of Five K. pneumoniae Isolates. Lane -: Negative Control, Lane +: Positive Control, Lane M: Marker DL 2000; B, PFGE of Five K. pneumoniae Isolates. Lane M: Salmonella Serotype Braenderup H9812. Lane 1 ~ 5: K. pneumoniae Isolated from Stool, Blood, Sanies, Throat Swab, and Urine
3. Discussion
As we all know, K. pneumoniae is one of the most common and clinically important pathogens worldwide, causing abscess (especially liver abscess) (7, 8), and then invades into blood causing multi-sites infection. It can also cause an endogenous infection in diabetes mellitus patients (9-11) as well as cancer patients (12). However, the report of K. pneumoniae in the intestine invading into blood is rare. This is the first time to report a K. pneumoniae isolate invading into the blood from the intestine in a patient who was receiving hemopoietic stem cell transplantation and then causes multi-sites infection. As we know, due to immunosuppress, leukemia patients often received an opportunistic infection through a different pathway. Like the EB virus and Aspergillus infection through respiratory tract (13, 14), urinary tract infection caused by Escherichia coli (15) and derma infection is caused by Herpes Zoster (16). However, infection caused by intestinal microbiology is rare, just a report of intestinal dysbacteriosis (17). As Chun-Ru Hsu et al. (18) reported K. pneumoniae can translocate across the intestinal epithelium; the gut is always the epicentre of antibiotics resistance (19). Therefore, we need to pay attention to the bacteria isolated from the intestine in the immunosuppressed patients.