1. Background
Lower respiratory tract infection remains one of the leading causes of mortality in children in developing countries (1). Mycoplasma pneumoniae is one of the common microorganisms causing pneumonia in pediatric patients, especially at school age (2). This type of pneumonia has different courses, ranging from mild pneumonia to acute respiratory distress syndrome (3). Macrolides have been introduced as the drug of choice for the treatment of M. pneumoniae infection in children. Additionally, the England Thoracic Society has recommended the administration of macrolides for all children who do not respond to other common treatments for pneumonia (3-5). The first report of macrolide-resistant M. pneumoniae (MRM) was published in 1997 (6). Since then, different incidence rates of MRM have been reported, with especially higher rates estimated in Asian countries. Its prevalence reportedly exceeds 80% in children in East Asian countries, while it is approximately 30% in West Asia (7-9).
Additionally, the amount of antibiotic use is high in Iran, and it is necessary to review and plan for the prescription of antibiotics (10). Due to the frequent use of antibiotics, the level of resistance to macrolides is high in Iran (11), and there is a need to limit their use (12). Some studies have reported a longer duration of disease, more severe pneumonia, and higher inflammatory markers in children with MRM. On the other hand, some studies reported no significant differences in the clinical and laboratory findings of children with MRM and macrolide-sensitive M. pneumoniae (MSM) (13, 14). However, more recent studies in adults showed patients with MRM pneumonia have not a severe course of pneumonia (15).
2. Objectives
To the best of our knowledge, this is the first study in Iran evaluating the prevalence of MRM in children with community-acquired pneumonia (CAP) and investigating the association of paraclinical and clinical findings of these patients.
3. Methods
3.1. Study Design and Population
In this cross-sectional study, a total of 222 children with symptoms of pneumonia, such as fever and tachypnea, who were hospitalized because of CAP in 10 different university hospitals in 10 states of Iran and met the inclusion criteria, were enrolled from November 2017 to February 2019. The inclusion criteria were as follows: (1) age range of 3 - 15 years (the most common age of Mycoplasma infection); (2) signs and symptoms of pneumonia; and (3) fever, cough, sputum, chest pain, crackles and wheezing, and infiltration on chest X-ray (CXR) (16). Conversely, the exclusion criteria were as follows: A history of immunosuppression confirmed by a detailed history of severe, persistent, and recurrent infection; a history of radiotherapy, chemotherapy, or cancer; and use of immunosuppressive drugs or corticosteroids. Children with the signs and symptoms of respiratory distress, according to the Infectious Diseases Society of America (IDSA) guidelines, were considered to have severe pneumonia (17). A checklist containing age, sex, family income, and family education was completed by the parents of eligible children.
3.2. Mycoplasma pneumoniae and Macrolide-resistant M. pneumoniae Detection
3.2.1. Sampling and Genome Extraction
In each hospital, a nurse was trained for nasopharyngeal sampling of M. pneumoniae, according to the World Health Organization (WHO) protocol (18). Training was provided using a training video according to the WHO guidelines, which was sent to every nurse in every city. Additionally, B-globin gene polymerase chain reaction (PCR) amplification was applied to observe false-negative results and genome extraction quality using the GH20/PC04 primer sets (19). All of the collected samples from children who were enrolled in this study according to the inclusion criteria were sent to Masih Daneshvari Hospital (Tehran, Iran) to perform PCR assays for Mycoplasma screening. These samples were placed in a buffered solution and stored at -80°C in a laboratory. Real-time PCR was carried out using primers and a probe targeting the community-acquired respiratory distress syndrome (CARDS) toxin gene region, as previously described (20). Genome extraction was conducted using the FavorPrepTM Viral Nucleic Acid Extraction Kit (FAVORGEN Biotech Corp., Taiwan). The extracted nucleic acid was preserved at -20°C until use.
3.2.2. Polymerase Chain Reaction Amplification and Sequencing of Domain V of 23S rRNA Gene
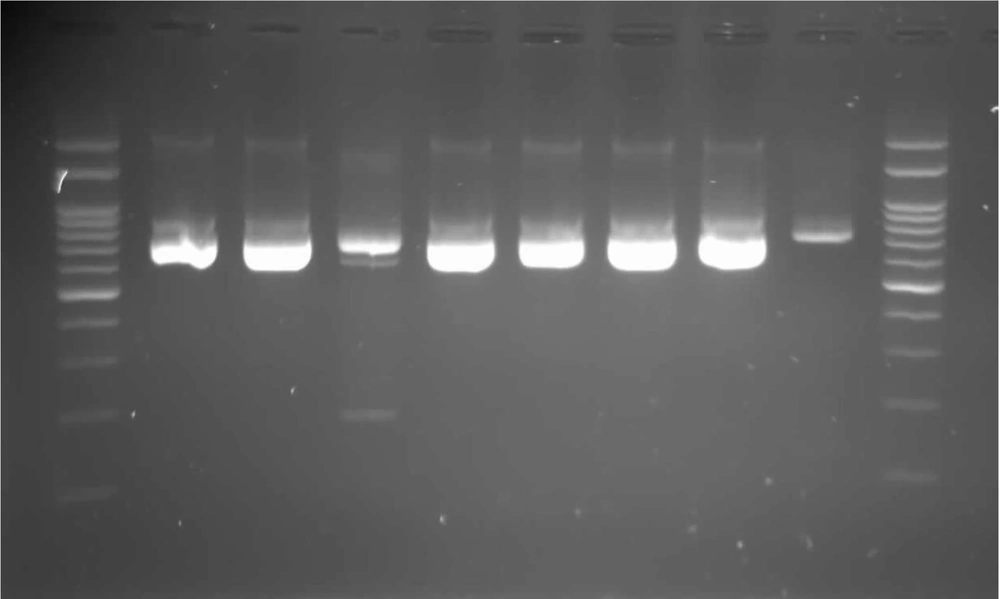
To detect point mutations of domain V of the 23S rRNA gene, some positive samples were subjected to sequencing of a 767-bp fragment (position 1918-2684 based on the accession No. of M. pneumoniae gene, X68422) by conducting a hemi-nested PCR, as previously described. The band size of M. pneumoniae n electrophoresis was 360bp. (Figure 1) (21).
3.3. Paraclinical Studies
3.3.1. C-reactive Protein Level
The C-reactive protein (CRP) level was measured quantitatively by the particle-enhanced turbidimetric immunoassay method (22).
3.3.2. Chest X-ray Recording
To eliminate discrepancies in radiology reports, CXRs were sent to all 10 children's hospitals. The findings of CXR were described as unilateral or bilateral involvement, and the type of involvement was described as lobar consolidation, patchy consolidation, and parapneumonic effusion (16). All CXRs were reviewed and reported by a single radiologist.
3.4. Statistical Analysis
The quantitative variables were reported as mean and standard deviation, while the qualitative variables were reported as frequency and percentage. The normality of the quantitative variables was assessed using the Kolmogorov-Smirnov test, and it appears that only the chi-square test was used for Table 1. To analyze the data, Mann-Whitney and Fisher’s exact tests were used as nonparametric tests, as the data did not have a normal distribution. A logistic regression analysis was also performed to evaluate the association of infection severity with CRP level in children with M. pneumoniae. Categorical data are presented as percentages. All the collected data were analyzed using SPSS version 21. P-values less than 0.05 were considered statistically significant.
| Variables | MP | MN | P-Value |
|---|---|---|---|
| Age (y), No. (%) | 0.040 | ||
| 3 - 5 | 1 (4.5) | 40 (20) | |
| 5 - 10 | 12 (54.54) | 110 (55) | |
| > 10 | 8 (36.3) | 50 (25) | |
| Sex, No. (%) | 0.08 | ||
| Male | 12 (54.54) | 150 (67.56) | |
| Pneumonia severity | 0.20 | ||
| Severe | 14 | 101 | |
| Non-severe | 7 | 100 |
Abbreviations: MP, mycoplasma positive; MN, mycoplasma negative.
a Values are expressed as No. (%) unless otherwise indicated.
4. Results
Mycoplasma pneumoniae was detected in 21 (9.4%) out of 222 children who met the inclusion criteria of this study. The demographic information of these children is summarized in Table 1. The MRM gene was detected in 17 (77.27%) cases. In patients with M. pneumoniae, the DNA load was < 103 in 19.04% of the patients, 103 - 105 in 47.61% of the patients, and ≥ 105 in 33.35% of the patients.
The mean CRP level was 35.5 ± 27.84 mg/L in M. pneumoniae-positive patients and 40.65 ± 55.73 mg/L in M. pneumoniae-negative patients. The results of the data analysis showed no significant differences between the two groups in terms of the CRP level (P = 0.71). Based on the results, the CRP level (43.90 mg/L) was higher in M. pneumoniae-positive patients with severe pneumonia compared to those with non-severe M. pneumoniae infection (14.75 mg/L); the difference, however, was not significant (P = 0.09). Additionally, a regression analysis was performed to evaluate the association of CRP level with the severity of M. pneumoniae. By adjusting for the DNA load (B = 0.54; 95% CI: -4.6 - 80.52; P = 0.07) and DNA load plus age and sex (B = 0.53; 95% CI: -12.88 - 87.78; P = 0.12), no significant association was found between the CRP level and M. pneumoniae infection severity. According to the CXR reports, there were no significant differences between M. pneumoniae-positive and M. pneumoniae-negative groups. Children with MRM pneumonia did not develop severe pneumonia (P > 0.99). Also, the CRP level of this group was not significantly higher than that of patients with MSM pneumonia (P = 0.08). Similarly, the CXR changes of these two groups were not significantly different (P = 0.07).
5. Discussion
The present findings showed that the prevalence of MRM pneumonia is 77.27% in Iranian children with CAP. The severity of pneumonia, changes in CXR, and CRP level were not significantly different between children with M. pneumoniae and those with other types of CAP. Similarly, the severity of pneumonia, CRP level, and CXR changes were not significantly different between patients with MRM and MSM pneumonia. The present study revealed that 9.4% of pediatric CAP patients are hospitalized due to M. pneumoniae. This finding is consistent with the prevalence of M. pneumoniae in other parts of the world (23, 24). Kutty et al. found that viral pathogens were co-pathogens in 28% of pediatric M. pneumoniae cases (25). In the present study, the radiological findings of pediatric patients with M. pneumoniae were not different from the CXR findings of children with CAP caused by other microorganisms. Evidence shows that the radiological findings of children with M. pneumoniae and viral pneumonia are similar (26). However, we did not isolate viral and other bacterial pathogens of CAP in our samples, which is a limitation of this study.
Researchers have attempted to find some markers to distinguish bacterial pneumonia from nonbacterial pneumonia. However, studies on the differentiation of typical pneumonia from atypical pneumonia have yielded discrepant results. In this regard, Olson et al. reported increased CRP levels in pediatric patients with pneumonia; however, this rise was not significant and could not differentiate M. pneumoniae from other bacteria (27); consistently, another study reported similar results (28). In our Iranian pediatric population with CAP, the mean CRP level was higher than that of patients with other types of CAP, although the difference was not significant; this result is in line with the findings of previous research. However, another study in pediatric China with pneumonia showed macrolide resistance pneumonia must be taken into consideration in children with pneumonia who did not respond to usual treatment and had higher levels of inflammatory markers (29).
Since 2000, the prevalence of MRM has been rising, especially in Asia (30). In the present study, 77.27% of children with M. pneumoniae showed macrolide resistance, which is consistent with the data reported in Korean and Chinese children (7, 31). The 23rRNA transition in Mycoplasma resulted in macrolide resistance (32), and high-level macrolide resistance was induced by A2063G, and A2064G transitions in the domain V of rRNA. All participants with MRM were considered high-level macrolide resistant because of the A2063G transition. In a recent study in Germany, Hubert et al. found the mutation in A2058G in macrolide resistance M. pneumonia in an outbreak in school; in our study, this mutation could not be found (33). Comparison of Mycoplasma genome with other bacteria showed that Mycoplasma only contains a single 23rRNA operon, which leads to the emergence of antibiotic resistance owing to antibiotic use (32). In Iran, macrolide use is high, especially in children, which can account for the high prevalence of MRM pneumonia in Iranian children. The results of the present study revealed that the severity of pneumonia was not different between MRM and MSM pneumonia patients. In this regard, some studies have shown that patients with MRM pneumonia may experience a more severe disease because of higher levels of interleukin-6 (IL-6) and IL-8 (34), while some others could not corroborate this result (35).
This finding is in line with a study in Taiwan (9). Commonly, antibiotic-resistant microorganisms do not cause severe diseases. Nonetheless, the number of samples with MRM and MSM pneumonia was limited in our study, which may be a limitation of our study. In the current study, CXR changes were not significantly different between children with MRM pneumonia and those with MSM pneumonia, which is concordant with the findings of previous research (16, 36). In the present study, although children with MRM pneumonia had higher levels of CRP, the difference was not significant and could not differentiate MRM from MSM pneumonia; this result is consistent with the findings reported by Tumgor et al. and Seo et al. (37, 38). Moreover, in a study conducted by Nabovati et al. in Iran in 2021, it was concluded that the consumption of antibiotics in Iran, including pediatric wards, was high (66%) and that these prescriptions needed to be restricted, as reported in the present study (10). Besides, in a study by Pourakbari et al. in 2018, the rate of resistance to macrolides, including erythromycin, was 65% in Iran, which is consistent with our study (11). In another study by Big Mohammadi et al. in 2020 in Iran, the rate of resistance to macrolides was high, and rational and limited prescriptions were considered necessary, as similarly described in our study (12).
The limitations of this study include the lack of isolation of viral or bacterial factors of CAP, non-evaluation of the clinical outcomes of CAP, and lack of funding. On the other hand, sampling from different regions of Iran and the use of PCR for the detection of M. pneumoniae are the strengths of this study.
5.1. Conclusions
The prevalence of high-level MRM pneumonia in children is high in Iran, similar to other Asian countries. However, this type of Mycoplasma infection was not associated with the severity of CAP and did not exert significant effects on CXR changes or CRP levels in our patients. In this study, the rate of MRM was 77.27%, which is due to the excessive use of macrolides.