1. Background
Cryptosporidiosis is a major public health problem in immunosuppressed human being as well as in neonatal livestock worldwide. Cryptosporidium parvum is transmitted via contaminated food or water, which may infect intestinal epithelial cells and results in cryptosporidiosis. Cryptosporidiosis is recognized as an emerging infectious disease by the centers for disease control and prevention (1). It is a self-limited disease, but may lead to a chronic infection and even become life-threatening in the immunocompromised individuals. It is estimated that cryptosporidiosis causes 5 to 10 million deaths each year (2); 13% to 74% prevalence is reported in HIV-positive children with diarrhea in sub-Saharan Africa (3), and 7. 8% to 10.3% in patients with HIV aged > 85 years in the United States (4).
Since the number of patients with AIDS is increasing in the developing countries, the significance of prevention and treatment of C. parvum is remarkable. Cryptosporidium parvum is a waterborne and zoonotic infection that can be transmitted to human via infected cattle, calves, sheep, etc. (5-8). In the developing countries, a major obstacle for disease control is the lack of effective methods to curb cryptosporidiosis and reduce environmental contamination with oocysts (9). Cryptosporidium parvum can be spread via food handlers, contaminated foods, fruits, vegetables, and unpasteurized cow milk (10-13). The epidemiology of C. parvum is investigated in Iran. The detection of C. parvum reported in cows is about 70.8% (14). The incidence of C. parvum in domestic animals was reported 59%; also the incidence of cryptosporidiosis in the exposed children was estimated 14.5% in the Southwest of Iran (14, 15). In the light of related diseases to C. parvum, it is required to conduct the periodical studies on the farm animals to prevent the spread of C. parvum in humans and animals.
Several animal model systems are described for clinical manifestation and drug designing against C. parvum so for, animals models included newborn BALB/c mice (16), rat, guinea pigs (17), calves (18), hamsters (19), and Arc/Swiss mice (20). At present, rats are used as animal model laboratory for in vivo studies of C. parvum to determine the incubation period, pathogenesis, immune response, and drug testing. Therefore, the current study aimed at evaluating the infectivity of C. parvum in the rats as an animal model.
2. Objectives
The current study aimed at evaluating the infectivity of C. parvum in the rats as an animal model.
3. Methods
Viable C. parvum oocyst Iowa strain was purchased from BTF Company (Sydney, Australia). Thirty neonatal Wistar rats aged 2 days were purchased from Razi vaccine and serum research institute, Karaj, Iran. A dose of 100,000 - 1,200,000 C. parvum was orally inoculated using gastric tube. Eight days post infection, the neonatal rats were scarified with ether and jejunum, ileum, caecum, colon, and rectum were removed; the contents were pooled and put in a Petri dish. Contents were homogenized (with an Ultra-Turrax homogenizer, 3 times for 10 second), Sputasol (2 mL/50 mL phosphate-buffered saline for 10 to 13 rats) was added and homogenized vigorously using bar mix (21).
The contents were mixed with 0.2 mL of homogenized suspension and stained by the Ziehl-Neelsen technique. The final purification of oocysts was conducted by sucrose gradients described by Lumb et al. Briefly, the Sheather sucrose solution was diluted 1:2 and 1:4 with sterile PBS (0.1 M, pH 7.2). The sucrose gradient was prepared by placing 10 mL of the 1:2 solution into 50 mL of polypropylene centrifuge tubes (Falcon; Becton Dickinson, Franklin Lakes, NJ) and, then, slowly adding 10 mL of the 1:4 solution. A 30 mL of the oocyst suspension (1.5 × 106/mL) was layered onto the 1:4 gradient. The sucrose gradient was centrifuged at 1, 700X g for 30 minutes at 48°C. Following the centrifugation, the potassium dichromate layer and half of the 1:4 gradient were collected with a pipette and, then, discarded. The remainder of the 1:4 gradient and 0.5 mL of the 1:2 gradient above the interface were recovered and dispersed into 80 mL of PBS, and the purified oocysts were counted. The suspension of oocysts per 1 mL was enumerated by a Neubauer hemocytometer.
4. Results and Discussion
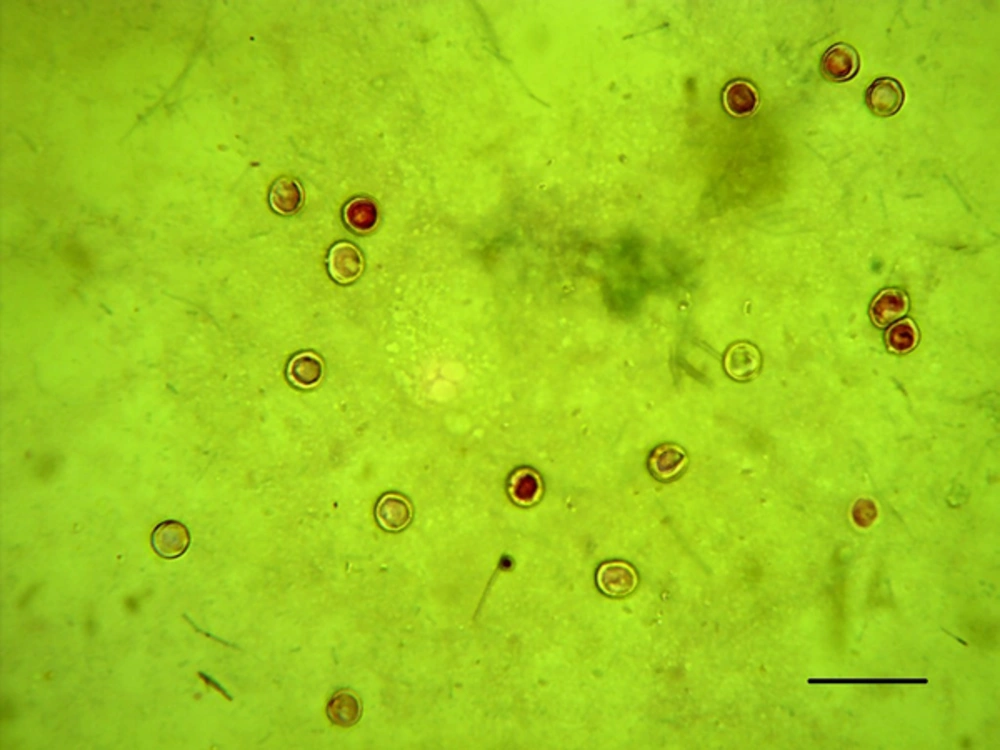
All inoculated neonatal rats showed signs such as watery stool, diarrhea, dehydration, weight loss, with a relative reduction in appetite. The shedding of oocyst in the feces of neonatal rat was observed at 8 days postinfection and confirmed by the Ziehl-Neelsen staining method (Figure 1). The results of oocysts purification by sucrose gradient revealed that about 6 to 12 million oocysts were observed in the samples, 8 days after infection.
The presence of an alternative animal model is important to evaluate further investigations on pathogenesis, immunological, drugs, and vaccine aspects. In the present study the number of oocysts in the neonatal rat was 60 to 100 times higher than the orally inoculated dose. The outcomes of the current study help to maintain infectivity of the oocytes as well as increasing and restoring the number of oocysts at 4°C for future studies. To purify the oocysts from the stool of postinfected rats, each step was carefully evaluated and recorded (22); mass production of C. parvum oocyst from postinfected mice as an animal model and its storage and maintenance at 4°C for a limited time were reported. Most of the studies indicated that mice are suitable as an animal model for infectivity, pathogenesis, and other investigations of the C. parvum oocysts (20, 23).
According to the results of the current study, clinical signs and symptoms of diarrheal were observed in the neonatal rats 8 days after the oral inoculation of C. parvum oocysts. In addition, the observation of 6 to 12 million oocysts indicated the dramatically increase of oocytes 60 to 100 times more than the initial does in the stools of postinfected neonatal mice. Based on the current study results, neonatal rat could be also used as an animal experimental model for the investigation of C. parvum in vivo. Mirza Qhavi et al. reported the peak of infection intensity of C. parvum oocysts with similar patterns of symptoms in neonatal mice and rats on the day 9. They concluded that it was easier to handle rats than mice during the procedure and rats were preferable for in vivo study to mice (24). Petry et al. observed high intensive infectivity of 109C. parvum oocyst in the stools of a group of 10 mice 8-10 days old immunosuppressed with dexamethasone (23). Current and Reese inoculated 3 isolates of C. parvum oocysts obtained from the cave of an immunocompetent individual, and a patient with HIV in mice and reported no difference on the clinical signs and symptoms among the mice infected with C. parvum oocysts with different origins (25).
The current study purified the C. parvum oocysts from the homogenized intestine of neonatal rats using sucrose gradient and recovered 6 to 12 million oocysts. Meloni and Thompson et al. purified 6 to 15 million C. parvum oocysts from the stool of infected neonatal Arc/Swiss mice using Ficoll gradient (20), which was in agreement with the current study findings. Emilio E et al. purified C. parvum oocysts from stool samples of a newborn goat infected with C. parvum using 6%, 16%, and 28% (w/v) KBr gradient in Tris-ethylenediaminetetraacetic acid (EDTA) buffer (26).
5. Conclusions
The results of the current study showed that 6 to 12 million oocysts were observed in the stool of 2-day days neonatal rats after infection with C. parvum (60 to 100 times more than the initial does). Thus, the 2-day old neonatal rats could be also used as an experimental animal model for C. parvum investigations.