1. Introduction
The Cryptococcus genus is a diverse group of fungi, with over 100 species identified to date, yet only a few of them are known to cause human diseases. Unlike other opportunistic pathogenic fungi, Cryptococcus is a deadly fungus with a high mortality rate once infection occurs (1, 2). In the late 19th century, the first documented cases of diseases in humans and animals caused by Cryptococcus were reported (3, 4). Subsequently, from 1940 to 1960, the incidence of cryptococcosis in Africa began to rise, which was believed to be linked to the emergence of the human immunodeficiency virus (HIV) (5). For a prolonged period, cryptococcosis was considered an HIV-associated disease. In reality, cryptococcosis does account for one-fifth of AIDS-related deaths (6).
Cryptococcus has the ability to cause pulmonary or disseminated infections, with cryptococcal meningitis being one of the most severe diseases it causes. It is estimated that there are 223,000 new cases annually, leading to the deaths of 181,100 HIV-infected individuals (7). With the improvement in diagnostic capabilities and advancements in immunotherapy, an increasing number of cases of cryptococcosis are being observed in non-HIV patients, with reports indicating that up to 20% of cases occur in immunocompetent individuals (8). The clinical manifestations of cryptococcal meningitis include acute or subacute fever, headache, vomiting, and focal neurological deficits (9), which lack distinct characteristics, posing a challenge to early diagnosis.
Here, we present a case of cryptococcal meningitis in a patient who exhibited noticeable psychiatric abnormalities before diagnosis. Through the description of this case, our aim is to enhance the understanding of the clinical manifestations and management of cryptococcal meningitis, thus aiding in the early diagnosis of this condition.
2. Case Presentation
2.1. Clinical Feature
A male patient in his 50s developed fever symptoms 10 days ago and underwent examination and treatment at a local hospital 7 days ago. He was diagnosed with infectious fever and received combination therapy with benzylpenicillin sodium and levofloxacin, but showed no improvement. During the treatment, he continued to experience recurrent fevers, accompanied by headaches, occasional cognitive impairment, nocturnal restlessness, irritability, and even aggression. Seeking further treatment, the patient was transferred to Zhejiang Provincial People’s Hospital.
Upon reviewing his medical history, we discovered that the patient had been diagnosed with nasopharyngeal cancer two years ago, had undergone chemotherapy, and subsequently developed lung metastases, receiving long-term immunotherapy since then. Previous behavioral abnormalities were attributed to the stress of cancer. After admission, in view of the patient's abnormal mental performance, we consulted clinical psychologists, who diagnosed him with an organic mental disorder. In addition, we conducted a comprehensive blood and cerebrospinal fluid (CSF) examination, with results shown in Table 1. Elevated infection markers combined with the results of cryptococcal capsular antigen testing (BIO-KONT, WK3023Q) led us to suspect cryptococcal infection in the patient. Considering his abnormal behavioral symptoms, we tentatively diagnosed him with cryptococcal meningitis.
| Laboratory Indicators | Result | Reference Range |
|---|---|---|
| Lymphocyte count (PB) | 0.45 × 109/L ↓ | 1.1 - 3.2 × 109/L |
| C-reactive protein (PB) | 107.3 mg/L ↑ | ≤ 10.0 mg/L |
| Serum total protein | 57.3 g/L ↓ | 65.0 - 85.0 g/L |
| Serum albumin | 32.9 g/L ↓ | 40.0 - 55.0 g/L |
| Serum procalcitonin | 0.55 ng/mL ↑ | ≤ 0.25 ng/mL |
| CD3+ cell count (PB) | 305 × 106/L ↓ | 952 - 2128×106/L |
| CD19+ cell count (PB) | 43 × 106/L ↓ | 173 - 447×106/L |
| CD3+CD4+ cell count (PB) | 70 × 106/L ↓ | 537 - 1282 × 106/L |
| CD3+CD8+ cell count (PB) | 219 × 106/L ↓ | 258 - 1042 × 106/L |
| Pan's test (CSF) | Positive | Negative |
| Protein quantification (CSF) | 172.5 mg/dL ↑ | ≤ 45.0 mg/dL |
| Glucose quantification (CSF) | 1.24 mmol/L ↓ | 2.50 - 4.50 mmol/L |
| Lactic dehydrogenase (CSF) | 54 U/L ↑ | 8 - 32 U/L |
| Chloride (CSF) | 115.8 mmol/L ↓ | 120-132 mmol/L |
| Lactic acid (CSF) | 7.7 mmol/L ↑ | 0.5 - 1.7 mmol/L |
| Serum Cryptococcus capsule antigen test | Positive | Negative |
Abbreviations: PB, peripheral blood.
2.2. Imaging Examination
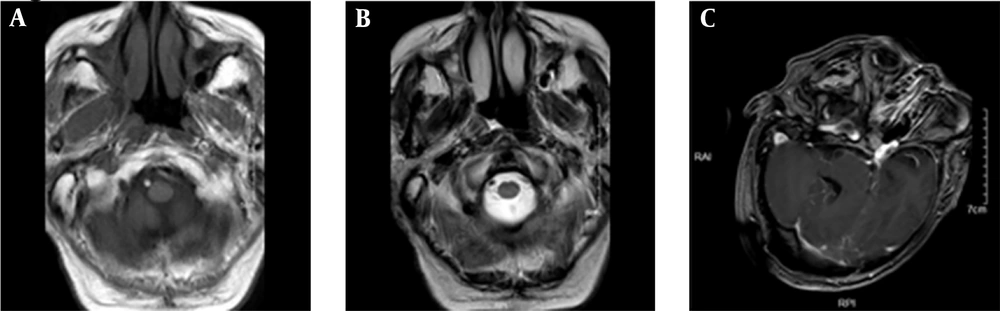
The patient underwent a head magnetic resonance imaging (MRI) examination, which showed severe artifacts. Scattered abnormal signal shadows were observed in the semioval area on both sides and the lateral ventricle. T1WI showed a slightly low signal, while T2WI and FLAIR showed a high signal, with blurred boundaries. There was no edema or mass effect around the lesion, and no obvious abnormal enhancement was observed in the enhanced scan. The third ventricle and lateral ventricle were slightly enlarged, and the cerebral pool and sulcus were slightly widened. The midline structure was not displaced (Figure 1).
2.3. Etiological Examination
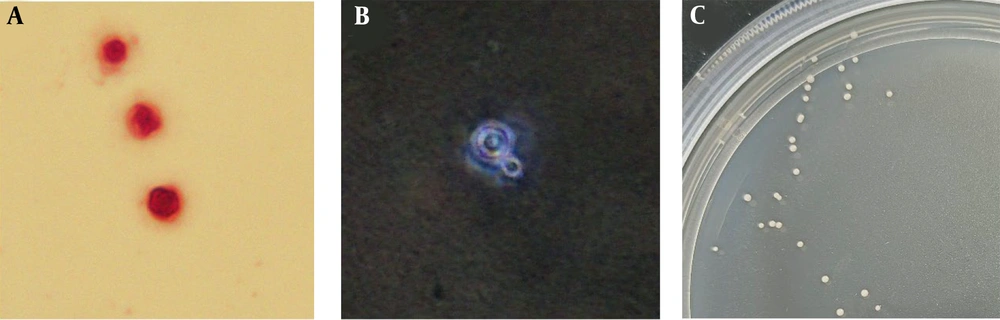
Following the detection of positivity for serum capsule antigen, cerebrospinal fluid was collected from the lumbar region of the patient for examination. Gram staining revealed circular yeast-like fungi under the microscope (Figure 2A), while India ink staining exhibited thick capsules surrounding the fungal cells (Figure 2B). The cerebrospinal fluid was inoculated onto Sabouraud dextrose agar medium using a loop, and after 48 hours of incubation at 37°C, smooth white yeast-like colonies were observed. Additionally, the isolated colony was identified as Cryptococcus neoformans using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS). The Clinical and Laboratory Standards Institute (CLSI) has developed standardized methods for broth microdilution antifungal susceptibility testing of both yeasts and molds (10). We obtained the antibiotic sensitivity of this strain of C. neoformans using this method (Table 2).
The microscopic morphology of Cryptococcus after different staining techniques was examined. A, after Gram staining, some circular yeast like fungi were found under the microscope; B, pink staining revealed a thick capsule surrounding the pathogen; C, white smooth colonies grow at 37℃ after CSF inoculation.
| Antibiotic | Method | Result | Break Point | Sensitivity Level |
|---|---|---|---|---|
| 5-fluorocytosine | MIC | ≤ 4 μg/mL | - | S |
| Itraconazole | MIC | ≤ 0.125 μg/mL | ≤ 0.25 | S |
| Voriconazole | MIC | ≤ 0.06 μg/mL | ≤ 0.25 | S |
| Amphotericin b | MIC | ≤ 0.5 μg/mL | ≤ 0.5 | S |
| Fluconazole | MIC | ≤ 1 μg/mL | ≤ 8 | S |
Abbreviations: MIC, minimum inhibitory concentration test strip method; S, Sensitive.
2.4. Treatment and Outcome
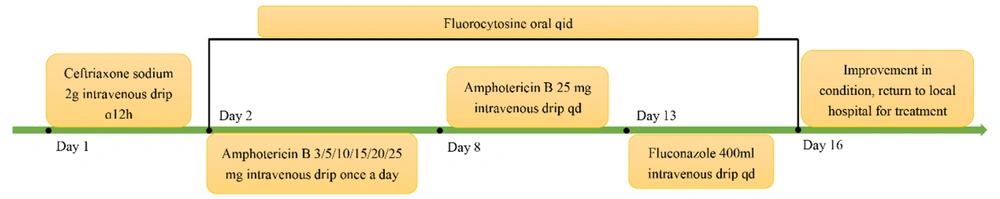
Upon admission, the patient was administered ceftriaxone sodium 0.2 g intravenously for standard anti-infective treatment. Following a confirmed diagnosis, the antibiotic was switched to amphotericin B 3 mg intravenously, gradually increasing to 25 mg by the 6th day (the dose increased daily: 3/5/10/15/20/25 mg). Additionally, the patient's family was instructed to purchase flucytosine tablets for combined antifungal therapy. On the 13th day of hospitalization, treatment was switched to 400 mL (0.2 g/100 mL) fluconazole intravenous infusion. By the 16th day, the patient showed improvement in symptoms with no headaches, no delirium, and no hallucinations. Consequently, it was agreed for the patient to return to the local hospital for further treatment, with a recommendation to continue the original regimen of fluconazole combined with flucytosine for an additional 4 weeks (Figure 3).
3. Discussion
In the latest list of pathogenic fungi issued by the World Health Organization (WHO), Cryptococcus has been classified as a crucial pathogen. It can enter the human body through the respiratory tract, depositing in the alveoli, and then further disseminate to skin tissues, internal organs, and the central nervous system, where the most severe clinical manifestation known as cryptococcal meningitis is observed (11). Cryptococcus neoformans and C. gattii are the main pathogenic fungi, primarily affecting HIV-infected patients (1). However, with advancements in medical technology in recent years, an increasing number of patients are able to receive organ transplants, immunotherapy, and other medical interventions. Consequently, the population with compromised immune systems is expanding, drawing attention to the issue of non-AIDS patients being infected with fungal pathogens.
Currently, there are well-established and specific methods for the detection of Cryptococcus—capsular antigen testing (serum or cerebrospinal fluid), which can serve as a direct indicator for diagnosing cryptococcal infection (12). Due to the lack of infection-specific clinical manifestations, cryptococcal infection is often not considered immediately when patients are admitted for infection, leading to delayed diagnosis. Hence, early diagnosis remains a significant challenge. The patient we report on presented with elevated inflammatory markers (high-sensitivity C-reactive protein, procalcitonin) on the day of admission. Additionally, abnormal lymphocyte levels were noted, including a deficiency in CD19+ B lymphocytes, CD4+ T lymphocytes, and CD8+ T lymphocytes. This immunocompromised state was attributed to cancer and prolonged immunotherapy, predisposing the patient to cryptococcal infection. Of particular concern is the patient's long-standing mental abnormalities prior to admission, characterized by recurring headaches and occasional hallucinations. Furthermore, the patient exhibited personality changes, irritability, and even instances of physical aggression.
In the study by Seelig et al., patients exhibited similar psychiatric symptoms, initially suspected to be drug-induced mental disorders (13). In our study, these changes were initially attributed to significant psychological stress following the cancer diagnosis. Here, we have collected and summarized some case reports on patients with cryptococcal meningitis (Table 3). We found that cryptococcal meningitis mostly occurs in male patients, and they all exhibit varying degrees of mental abnormalities such as headaches, consciousness disorders, irritability, strong aggression, and hallucinations. Therefore, when managing patients with cryptococcal meningitis, such psychiatric behavioral anomalies should be carefully considered, especially in cases without a history of psychiatric illness or relevant drug usage.
| Year | Country | Age | Gender | Abnormal Mental Manifestations | Reference |
|---|---|---|---|---|---|
| 2009 | USA | 62 | Male | Headaches, dizziness, blurry vision, imbalance, become dull, frequent cursing, shouting at noisy people, gritting one's teeth, getting angry when disliked, having a hot temper, not brushing teeth, not taking a shower, and showing a lack of personal hygiene | (14) |
| 2009 | China | 70 | Male | Depressed mood, loss of interest, fatigue, poor concentration, pessimistic thought, initial insomnia, poor appetite, severe depression | (15) |
| 2011 | India | 49 | Male | Psychosis | (16) |
| 2013 | Singapore | 30 | Male | Solitary personality, ignoring others, anxiety, headache, walking like a zombie, hallucinations | (17) |
| 2014 | China | 78 | Male | Decreased sleep, elevated mood, increased energy, hyperactivity, racing thoughts, and eccentric behaviour (such as being stark naked at home) | (18) |
| 2017 | USA | 45 | Male | Yelling, combative, and not answering questions or following commands | (13) |
| 2020 | USA | 26 | Male | Blurred vision and confused language, unclear consciousness | (19) |
| 2020 | USA | 30 | Male | Headache, blurry vision, hearing loss, and gait imbalance | |
| 2023 | USA | 55 | Male | Progressive headache with unclear consciousness | (20) |
| 2023 | USA | 73 | Male | Headaches, progressive weakness, fatigue, and worsening confusion | (21) |
| 2023 | USA | 44 | Male | Elevated intracranial pressure and stubborn headache | |
| 2024 | China | 50s | Male | Headaches, occasional cognitive impairment, nocturnal restlessness, irritability, and even aggression | Our report |
In June 2022, WHO released new clinical management guidelines for cryptococcal meningitis, strongly recommending the use of single high-dose liposomal amphotericin B therapy combined with 2-week flucytosine and fluconazole as the preferred treatment approach (22). Liposomal amphotericin B is a common first-line drug for managing co-infections in HIV-infected individuals. However, in many low- and middle-income countries with public healthcare systems, the cost of this medication can pose a significant economic burden (23). Therefore, early and prompt diagnosis, proper guidance on medication use, and prevention of disease progression are crucial.
3.1. Conclusions
Cryptococcal meningitis is an extremely fatal disease, characterized by a high mortality rate. However, early diagnosis remains challenging due to the absence of clear clinical manifestations. The psychiatric and behavioral abnormalities exhibited in the early stages are often misdiagnosed as other mental disorders or simply attributed to stress, leading to delayed diagnosis and exacerbating the treatment burden. Therefore, the psychiatric and behavioral presentations in the diagnosis of cryptococcal meningitis should be emphasized.