1. Background
Cirrhosis is a pathological condition characterized by diffuse liver fibrosis, pseudolobule formation, and proliferation of intrahepatic and extrahepatic vessels. A decompensation period is characterized by portal hypertension and severe liver function injury. Patients often die of multiple organ failure caused by ascites, gastrointestinal bleeding, sepsis, etc. (1, 2). Multidrug-resistant (MDR) bacteria are important pathogens of nosocomial infection (3) and are also among the most important determinants affecting the prognosis of critically ill patients. Infection is a high-risk factor for complications and death in patients with liver cirrhosis (LC) (4). Bacterial infection is closely related to the clinical course of patients with decompensated LC, which can increase the short-term mortality of patients by 2 - 4 times (5). Many European scholars believe that when bacterial infection occurs in patients with decompensated LC, the proportion of bacteria with multidrug resistance is very high (6). Multidrug-resistant bacterial infection is a common and serious medical problem in patients with decompensated LC, which has a very negative impact on the prognosis of patients (7).
However, at present, scholars both domestically and internationally have focused on the use of empirical drugs, new methods, new ideas, and antibiotics in the study of MDR bacterial infection in decompensated LC (8, 9). There is little analysis on the related factors affecting the occurrence of MDR bacterial infection in such patients, which need to be further studied and discussed. Understanding the risk factors of true MDR bacterial infection in patients with decompensated LC is of great significance to identify the occurrence of MDR bacterial infection and improve the prognosis of patients.
2. Objectives
Therefore, this study analyzed the risk factors of MDR bacterial infection in patients with decompensated LC in order to provide a reference for the prevention of MDR bacterial infection in patients with clinical LC.
3. Methods
3.1. Design, Study Time and Place
This study employed a retrospective design. From January 2017 to December 2020, it was conducted in the Infection Department of the First Affiliated Hospital of Suzhou University in Jiangsu province. Patients with compensatory LC treated in the Department of Infectious Diseases of the First Affiliated Hospital of Suzhou University during the same period were included as the study population.
3.2. Inclusion and Exclusion Criteria
Inclusion criteria for the study were as follows: Patients diagnosed with compensatory stage LC, patients with complete case data, and patients with decompensated LC who experienced MDR bacterial infections during the study period (only the first infection was analyzed). Exclusion criteria included patients with malignant tumor disease, patients with severe cardiac insufficiency and pulmonary dysfunction, and those with MDR bacterial infection prior to admission.
3.3. Diagnostic Criteria
3.3.1. Guidelines for Diagnosis and Treatment of Decompensated Liver Cirrhosis
Refer to the guidelines published by the Chinese Association of Hepatologists in 2019 (10): (1) Have the basis for the diagnosis of LC; (2) portal hypertension-related complications, such as ascites, esophageal gastric vein/variceal bleeding, sepsis, hepatic encephalopathy, hepatorenal syndrome, and others.
3.3.2. Diagnostic Criteria for Multidrug-Resistant Bacteria
Based on the diagnostic criteria of nosocomial infection issued by the Ministry of Health in 2001, more than two tests or more than two consecutive tests must be positive for the same strain. When three or more commonly used antibiotics, which are usually sensitive (anti-Pseudomonas cephalosporins, anti-Pseudomonas carbapenem antibiotics, compound preparations containing β-lactamase inhibitors, fluoroquinolone antibiotics, aminoglycoside antibiotics), show resistance simultaneously, it is diagnosed as a MDR bacterial infection (11).
3.4. Sample Size Estimation
The estimation method of sample size is based on Kendall (12). In multivariate analysis, the sample size can be selected as 5 - 10 times the number of research items. This study contains 23 items, and the sample size is estimated to be between 115 and 230.
3.5. Data Collection Table
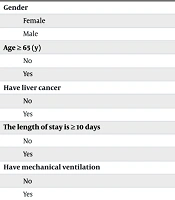
According to the literature and clinical experience, the research team designed a general data questionnaire (Table 1) after discussion and collected the following data from patients who met the inclusion criteria: (1) Basic Information of the patient: Age, sex; (2) disease-related data: Primary disease of LC, length of hospital stay, mechanical ventilation, admission to ICU, use of hormones, use of antibiotics for ≥ 5 days, diabetes mellitus, oral fungal infection, invasive operation, hospitalization within three months, septic shock; (3) laboratory Indicators: Serum albumin, serum sodium.
After obtaining consent from the department, the researchers used the case data management system to query the hospitalization numbers of patients with decompensated LC in the Infection Department of the First Affiliated Hospital of Suzhou University in Jiangsu province from January 2017 to December 2020. The researchers screened the participants and used the electronic medical system and nursing record sheets to query, collect, and input patient data.
3.6. Quality Control
The inclusion and exclusion of subjects in the dual-center study were conducted according to unified criteria, ensuring that patients who did not meet the inclusion criteria were excluded. Medical records were collected according to a unified standard and accurately recorded in a self-made questionnaire. Another individual reviewed the collected data to ensure that it was complete, true, and reliable.
3.7. Statistical Analysis
SPSS version 21.0 software was used for statistical analysis. The counting data were described by the number of cases and percentage. All observed indicators were then assessed using univariate analysis, employing either the chi-squared test or the corrected chi-squared test as appropriate. Subsequently, variables demonstrating statistical significance in the univariate analysis were included in a binary logistic regression model for multivariate analysis, with P < 0.05 considered statistically significant.
4. Results
4.1. Analysis of Number of Participants
Patients with cirrhosis who met the inclusion criteria in the Infection Department of the First Affiliated Hospital of Suzhou University in Jiangsu province were collected. According to the inclusion and exclusion criteria, 133 patients were ultimately included for analysis.
4.2. Analysis of Two Groups of General Data
There were 33 patients in the MDR bacterial infection group, including 23 males (69.7%), 14 patients aged ≥ 60 years, 19 patients less than 60 years old, 6 cases complicated with liver cancer, 29 cases with infection ≥ 10 days in hospital, 25 cases with mechanical ventilation, 27 cases with ICU infection, 30 cases with hormone infection, 33 cases with antibiotics ≥ 5 days, 11 cases with diabetes and 4 cases with fungal infection. There were 29 cases of invasive operation, 17 cases of 3-month hospitalization, 26 cases of septic shock, 26 cases of albumin ≤ 28 and serum sodium ≤ 130 mmol/L. Statistics showed that the mortality rate of LC decompensated patients with MDR bacteria infection group (19.1%) was higher than that of non-infection group (6.5%).
4.3. Infection Rate and Strain Distribution of Multiple Drug-Resistant Bacteria in Decompensated Liver Cirrhosis
Among the 133 subjects, a total of 33 patients with decompensated LC developed MDR bacterial infection, with an infection rate of 24.81%. Among them, 16 cases were infected with carbapenem-resistant Acinetobacter baumannii (CR-AB), accounting for the majority (49%). The remaining cases of MDR bacteria included 10 cases of carbapenem-resistant Enterobacteriaceae (CRE), 3 cases of methicillin-resistant Staphylococcus aureus (MRSA), 2 cases of MDR Pseudomonas aeruginosa (MDR-PA), and 2 cases of extended-spectrum beta-lactamases (ESBLs), as shown in Table 1.
| MDR Bacteria Species | Number of Bacteria (Strains) | Constituent Ratio (%) |
|---|---|---|
| CR-AB | 16 | 49 |
| CRE | 10 | 30 |
| MRSA | 3 | 9 |
| MDR-PA | 2 | 6 |
| ESBLs | 2 | 6 |
Abbreviations: MDR, multidrug-resistant; CR-AB, carbapenem-resistant Acinetobacter baumannii; CRE, carbapenem-resistant Enterobacteriaceae bacteria; MRSA, methicillin-resistant Staphylococcus aureus; ESBLs,β-lactamase; MDR-PA, multi-drug resistant Pseudomonas aeruginosa.
4.4. Univariate Analysis of Risk Factors of Multiple Drug-Resistant Bacteria Infection in Decompensated Liver Cirrhosis
According to the statistics, among the 133 subjects, there were 33 cases of MDR bacterial infection and 100 cases of non-infection in patients with decompensated LC. There was a significant difference between the two groups in terms of hospitalization duration ≥ 10 days, mechanical ventilation, ICU admission, hormone use, invasive operation, septic shock, and albumin ≤ 28 g/L (Table 2).
| Projects and Groups | Uninfected Group (n = 100) | Infection Group (n = 33) | χ2 | P-Value |
|---|---|---|---|---|
| Gender | 0.006 | 0.940 | ||
| Female | 31 (31.0) | 10 (30.3) | ||
| Male | 69 (69.0) | 23 (69.7) | ||
| Age ≥ 65 (y) | 1.331 | 0.249 | ||
| No | 46 (46.0) | 19 (57.6) | ||
| Yes | 54 (54.0) | 14 (42.4) | ||
| Have liver cancer | 0.240 | 0.876 | ||
| No | 83 (83.0) | 27 (81.8) | ||
| Yes | 17 (17.0) | 6 (18.2) | ||
| The length of stay is ≥ 10 days | 10.354 | 0.001 | ||
| No | 43 (43.0) | 4 (12.1) | ||
| Yes | 57 (57.0) | 29 (87.9) | ||
| Have mechanical ventilation | 47.884 | < 0.001 | ||
| No | 87 (87.0) | 8 (24.2) | ||
| Yes | 13 (13.0) | 25 (75.8) | ||
| Admission to ICU | 14.997 | < 0.001 | ||
| No | 57 (57.0) | 6 (18.2) | ||
| Yes | 43 (43.0) | 27 (81.8) | ||
| Have the use of hormones | 19.624 | < 0.001 | ||
| No | 53 (53.0) | 3 (9.1) | ||
| Yes | 47 (47.0) | 30 (90.9) | ||
| Use antibiotics for more than 5 days | 3.782 | 0.052 | ||
| No | 19 (19.0) | 1 (3.0) | ||
| Yes | 81 (81.0) | 32 (97.0) | ||
| Have diabetes | 2.468 | 0.116 | ||
| No | 80 (80.0) | 22 (66.7) | ||
| Yes | 20 (20.0) | 11 (33.3) | ||
| There is oral fungal infection | 0.134 | 0.714 | ||
| No | 92 (92.0) | 29 (87.9) | ||
| Yes | 8 (8.0) | 4 (12.1) | ||
| Intrusive operation | 9.243 | 0.002 | ||
| No | 41 (41.0) | 4 (12.1) | ||
| Yes | 59 (59.0) | 29 (87.9) | ||
| Hospitalization experience within three months | 1.869 | 0.172 | ||
| No | 62 (62.0) | 16 (48.5) | ||
| Yes | 38 (38.0) | 17 (51.5) | ||
| Complicated with septic shock | 62.321 | < 0.001 | ||
| No | 91 (91.0) | 7 (21.2) | ||
| Yes | 9 (9.0) | 26 (78.8) | ||
| Albumen ≤ 28 g/L | 7.074 | 0.008 | ||
| No | 57 (57.0) | 10 (30.3) | ||
| Yes | 43 (43.0) | 23 (69.7) | ||
| Serum 130 mmol | 0.029 | 0.865 | ||
| No | 88 (88.0) | 28 (84.8) | ||
| Yes | 12 (12.0) | 5 (15.2) |
a Values are expressed as No. (%).
4.5. Logistic Regression Analysis of Multiple Drug-Resistant Bacteria Infection in Decompensated Liver Cirrhosis
Taking the occurrence of MDR bacterial infection as the dependent variable, seven statistically significant factors were identified in the univariate analysis: (1) Length of stay ≥ 10 days; (2) mechanical ventilation; (3) hormone use in the ICU; (4) use of hormones; (5) invasive procedures; (6) septic shock; (7) albumin ≤ 28 g/L. These factors were used as independent variables for logistic regression analysis. The statistical results indicated that a hospital stay of ≥ 10 days (OR: 0.184, 95% CI: 0.45 - 90.748, P = 0.018) and septic shock lasting ≥ 10 days (OR: 0.027, 95% CI: 0.009 - 0.084, P < 0.001) were independent risk factors for MDR bacterial infection in patients with decompensated LC (Table 3).
| Risk Factors | Β-Value | SE | Wald Chi-square Value | OR-Value | OR Value (95% CI) | P-Value |
|---|---|---|---|---|---|---|
| Admission to ICU | 0.034 | 0.821 | 0.002 | 1.034 | 0.207 - 5.174 | 0.967 |
| There are invasive procedures. | 0.128 | 0.819 | 0.024 | 1.136 | 0.228 - 5.651 | 0.876 |
| Albumin ≤ 28 g | 0.454 | 0.607 | 0.561 | 0.635 | 0.193 - 2.084 | 0.454 |
| With mechanical ventilation | 0.862 | 0.748 | 1.327 | 0.422 | 0.097 - 1.831 | 0.249 |
| Use of hormones | 1.186 | 0.765 | 2.401 | 0.306 | 0068 - 1.369 | 0.121 |
| Hospital stay ≥ 10 days | 1.693 | 0.716 | 5.596 | 0.184 | 0.45 - 0.748 | 0.018 |
| Septic shock was complicated | -3.623 | 0.583 | 38.652 | 0.027 | 0.009 - 0.084 | < 0.001 |
5. Discussion
5.1. Patients with Decompensated Liver Cirrhosis Are Likely to be Complicated with Multidrug-Resistant Bacterial Infection
Decompensated cirrhosis significantly increases susceptibility to infection, frequently leading to sepsis and organ failure. This heightened vulnerability stems from LC-induced immune dysfunction. Further contributing to this risk are gut dysbiosis and impaired intestinal barrier function, which promote bacterial translocation and systemic inflammation (13, 14). Clinically, empirical antibiotic treatment is often necessary in cirrhotic patients due to gastrointestinal bleeding or suspected infection; however, this practice has inadvertently accelerated the emergence of MDR organisms. The resulting increase in bacterial resistance has consequently elevated the incidence of MDR infections in cirrhotic patients (15). In patients with established MDR infections, the pre-existing immunosuppression, coupled with a robust inflammatory response, creates a critical imbalance, hindering effective infection control and increasing the risk of multi-organ failure (16).
Many studies have shown that since the 1990s, the probability of MDR bacterial infection in patients with decompensated cirrhosis has increased year by year (17). In recent years, a large European multicenter observational study showed a significant increase in MDR bacterial infections in patients with decompensated cirrhosis, from 29.2% in 2017 to 38% in 2011 - 2018 (8). In this study, 33 patients with decompensated LC were complicated with MDR bacterial infection, with an infection rate of 24.81%. Among them, CR-AB and CRE infections were the most frequent, with 16 cases (49%) and 10 cases (30%), respectively.
The infection rate was similar to that reported by foreign scholars in 2017 - 2018 for decompensated patients with LC complicated with MDR bacterial infection (18). However, it is worth noting that there are obvious differences in the distribution of infectious strains, which suggests that there may be regional differences in bacterial species and may also reflect differences in the use of antibiotics in different periods and different medical institutions. In the future, further research should be conducted on the common MDR bacteria and their resistance mechanisms in patients with decompensated cirrhosis in different regions and periods. This will not only help understand the causes of the formation of regional infection spectra but also help guide anti-infection treatment strategies in different regions.
5.2. Analysis of Risk Factors
The length of stay ≥ 10 days is an independent risk factor for MDR bacterial infection in patients with decompensated LC. With the increase in hospitalization time for patients with decompensated LC, the increase in invasive procedures and the use of related antibiotics, the transformation of drug-resistant bacteria in patients, and possible cross-infection among patients, the probability of MDR bacterial infection increases (16). A study that analyzed the correlation between length of hospital stay and acquisition of MDR bacterial infection showed that patients hospitalized for 10 days or more had the highest risk of infection (18), which is consistent with the results of this study. However, this study is a single-center retrospective study, which may have selection bias, and the sample size is relatively limited, which may limit the extrapolation of its findings.
In light of the aforementioned findings, we underscore the critical need for clinical healthcare providers to prioritize and actively implement infection control measures during the hospitalization of patients with decompensated cirrhosis, including proper hand hygiene techniques and timing, correct glove utilization, maintenance of a clean ward environment, routine disinfection of frequently used equipment, single-room isolation when indicated, and judicious antibiotic use to mitigate the incidence of MDR bacterial infection (7).
Septic shock is an independent risk factor for MDR bacterial infection in patients with decompensated LC. Patients with decompensated LC develop LC-related immune dysfunction (19), which leads to decreased immune regulation and anti-infection ability of the body. Under the dual action of pro-inflammatory cytokines and hemodynamic disorders, this will be associated with septic shock (20). Septic shock is a combination of severe cellular, metabolic, and circulatory disorders on the basis of sepsis, with a fatality rate of more than 25%. Some patients are prone to develop multiple organ failure, and it is difficult to cure clinically (21). When patients develop septic shock, antibiotics that may cover all pathogens are needed (22); patients are prone to acute respiratory distress syndrome and use mechanical ventilation and other invasive procedures; these increase the risk and mortality of MDR bacterial infections. This view is also supported by the papers of relevant foreign scholars (23, 24). Therefore, prompt initiation of active treatment for septic shock, encompassing fluid resuscitation and the administration of vasoactive agents, is crucial to stabilize patients’ vital signs and mitigate the incidence of MDR bacterial infection.
While this study employed rigorous methods to mitigate bias, certain limitations remain. Specifically, despite the exclusion criteria stipulating the absence of prior malignancy, 23 patients with a diagnosis of liver cancer were included. Liver cancer is often associated with impaired liver function, potentially elevating the risk of MDR bacterial infection. Consequently, fully distinguishing the independent effects of liver cancer and its associated complications on infection risk may not be feasible, which may introduce confounding bias. However, despite this potential bias, we contend that the primary conclusions of this study remain robust. Future investigations could mitigate these limitations through the inclusion of more homogeneous patient populations or the implementation of refined stratified analyses.
5.3. Conclusions
This study unequivocally demonstrated that a length of hospital stay ≥ 10 days, combined with septic shock, are independent risk factors for MDR bacterial infection in patients with decompensated cirrhosis. These findings offer crucial guidance for clinical practice, including the early identification of high-risk individuals, implementation of proactive infection management strategies, and optimization of hospital care pathways. However, the limitations of this study, primarily its single-center retrospective design and relatively small sample size, warrant acknowledgment. Therefore, future research should employ a multicenter, large-scale prospective study design to validate these findings and explore predictive models and intervention strategies for MDR bacterial infection.