1. Background
Fungal sinusitis (FS) is an infection or inflammation of the sinuses caused by different species of fungi, including Aspergillus, Penicillium, Mucor, Rhizopus, and Phaeohyphomycetes (1). This disease can be classified into five different manifestations: Invasive, chronic invasive, fungal ball, saprophytic, and allergic fungal (2, 3). Fungal sinusitis infections begin in the paranasal sinuses. The paranasal sinuses consist of four pairs of air-filled cavities at the entrance to the upper airway, including the maxillary, frontal, sphenoid, and ethmoid sinuses (4). In recent years, molecular biology has found its way into medical mycology and opened very promising horizons for specialists in this field (5). Ribosomal DNA sequencing, as a fungal detection method, can be applied to indicate the identification of a large mutation in the fungal genome (6).
The fungal genome contains specific regions that have been found to be very helpful in species identification, molecular epidemiology, and fungal taxonomy because of their nucleotide sequence diversity in different species of the same genus (7). These regions include the internal transcribed spacer, beta (β)-tubulin, IGS, and gene encoding elongation factor 1 (eEF-1α) regions (8-10). Polymerase chain reaction (PCR)-based methods can be optimal for fungal detection and exhibit greater susceptibility rates than other methods. In addition to molecular identification of fungal, they provide researchers with significant information regarding drug resistance, fungal taxonomy, and molecular epidemiology (11).
Three types of antifungals are mainly used for the treatment of FS: Polyenes, azoles, and echinocandins (8). Azoles are useful for all filamentous fungi except fluconazole (12). However, posaconazole has exhibited its activity against Mucor spp (13). Except for Mucorales, echinocandins are highly active antifungals against all fungal agents, but they have not yet been widely used, especially in Iran (14). Fluconazole and flucytosine (5-fluorocytosine) are inactive against filamentous fungi (15, 16). Recently, luliconazole and lanoconazole have exhibited good In vitro antifungal properties against filamentous fungi (17). Currently, the Clinical and Laboratory Standards Institute (CLSI) has recommended standard methods for antifungal susceptibility testing (AFST) in the CLSI document M38-A2 for filamentous fungi to provide reproducible results (18). The AFST provides insight into the susceptibility profiles of collected isolates and shows drug resistance of clinical strains (19).
2. Objectives
The present study was aimed at molecular identification and drug susceptibility evaluation of fungal strain isolated from FS.
3. Methods
3.1. Fungal Isolates
This study was designed in medical mycology and parasitology department, School of Medicine, Babol University of Medical Sciences in north of Iran from January 2017 to January 2023. Fungal isolates studied in this research included 61 strains, including 50 Aspergillus spp and 11 isolates of Rhizopus spp. All isolates were collected from Mazandaran, Mashhad and Tehran provinces. All patients’ data were processed anonymously, and the ethics committee waived its informed consent form. Fungal isolates were stored in 20% glycerol solutions at -80℃ for further investigation.
3.2. Phenotypic Identification
The suspensions of spores or mycelium were inoculated onto Sabouraud Dextrose Agar (SDA) (HiMedia, India) plates and incubated at 37℃ for 5 - 7 days, as previously described. Microscopic slides were prepared using the methylene blue staining procedure and examined by light microscopy.
3.3. Molecular Identification
DNA extraction from the isolates grown in SDA for 3 - 7 days at 37°C was performed as previously method described by Dehqan et al. (20). For Rhizopus spp. isolates, the rDNA ITS region was amplified by primers ITS1 and ITS4 (21). In addition, for Aspergillus spp, the part of the BenA gene that encoded β-tubulin was amplified using primers βtub1 and βtub2 (11). The final volume of the PCR was 25 μL, containing 0.25 μM of 10-pmol primer, 12.5 μL of 2× master mix (Ampliqon, Denmark), 1 μL of DNA template, and deionized water. Moreover, 1% agarose gel electrophoresis was performed to detect gene amplification in the samples, and images were taken with a UV transilluminator. The isolates were identified at the species level and for further analysis by importing the obtained sequence data into MEGA software (version 6). The ambiguously aligned regions were adjusted manually to improve alignment accuracy. Furthermore, the final identification of the isolates was performed by comparing the obtained sequences with the National Center for Biotechnology Information (NCBI)’s reference sequence (RefSeq) database.
3.4. Antifungal Susceptibility Evaluation Based on CLSI-M38-A2 Guidelines
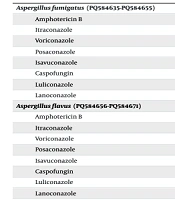
The in vitro minimum inhibitory concentrations (MICs) for filamentous fungi were determined using the broth microdilution method according to the CLSI-M38-A2 document (22). Eight antifungal drugs, including amphotericin B, itraconazole, voriconazole, posaconazole, isavuconazole, caspofungin, luliconazole, and lanoconazole (Sigma-Aldrich, USA) were obtained as reagent-grade powders from the particular producers for preparation of the CLSI microbroth dilution trays. The drugs were diluted in the RPMI-1640 medium adjusted to pH = 7.0 with M-morpholinepropanesulfonic acid (MOPS) (Sigma-Aldrich, USA) with Lglutamine and dispensed into 96-well microplates at a final concentration of 0.032 - 16 μg/mL for polyene and azoles; 0.016 - 8 μg/mL for caspofungin.
The spore suspensions were prepared from fresh colony of isolates grown on SDA, spectrophotometrically at 530 nm wavelengths to an optical density that ranged from 0.15 - 0.17 for Rhizopus isolates and from 0.09 - 0.13 for Aspergillus strains. The MICs endpoints for polyene and azole were defined as the lowest concentration of antifungal that inhibited identifiable growth (100% inhibition growth) for all fungal strains. However, for Aspergillus and Rhizopus strains, minimum effective concentration (MEC) endpoints for caspofungin were determined microscopically as the minimal drug concentration that produced noticeable morphological modifications of the septate and non-septate hyphae, respectively. The values of MIC50/MEC50, MIC50/MEC90, GMs, and MICs range were calculated by importing the raw data of each antifungal into Excel software (version 2018). Strains Candidaparapsilosis (ATCC22019) and C.krusei (ATCC6258) were used as test controls. The raw data MEC/MICs were entered into SPSS version 22 and were then analyzed using descriptive statistics and cross arrangement.
4. Results
The patients had an age range of 28 to 71 years and a mean age of 59 years. Of these patients, 38 patients were male and 33 were female. Fungal involvement of the paranasal sinuses is commonly was observed in the patients. The headache (40.1%), fever (32.8%), nasal discharge (29.5%) and facial pain (23%) were the most clinical signs. A total of 61 strains, including 21 isolates of Aspergillus fumigatus, 16 isolates of Aspergillus flavus, 13 isolates of Aspergillus niger, and 11 isolates of Rhizopus arrhizus were identified by DNA sequencing. All R. arrhizus isolates were isolated from the patients with underlying COVID-19 and diabetes diseases.
Table 1 presents the GM/MIC/MEC90/MIC/MEC50 values and the dilution range of 8 different antifungal drugs (amphotericin B, itraconazole, voriconazole, posaconazole, isavuconazole, caspofungin, luliconazole, and lanoconazole) for different fungal species. For all isolates, GM-MIC/MEC, from lowest to highest, was obtained for luliconazole (0.047 μg/mL), lanoconazole (0.070 μg/mL), posaconazole (0.150 μg/mL), itraconazole (0.347 μg/mL), voriconazole (0.695 μg/mL), caspofungin (0.634 μg/mL), isavuconazole (1.146 μg/mL), and amphotericin B (1.172 μg/mL).
| Species/Accession Numbers and Antifungal Agent | MIC/MEC (µg/mL) | |||
|---|---|---|---|---|
| 50% a | 90% a | GM b | Range | |
| Aspergillusfumigatus (PQ584635-PQ584655) | ||||
| Amphotericin B | 1 | 1 | 0.847 | 0.125 - 2 |
| Itraconazole | 0.25 | 0.5 | 0.294 | 0.025 - 0.5 |
| Voriconazole | 0.25 | 0.5 | 0.285 | 0.025 - 1 |
| Posaconazole | 0.064 | 0.125 | 0.082 | 0.064 - 0.25 |
| Isavuconazole | 0.5 | 1 | 0.629 | 0.5 - 2 |
| Caspofungin | 0.5 | 0.5 | 0.423 | 0.125 - 1 |
| Luliconazole | 0.032 | 0.032 | 0.034 | 0.032 - 0.125 |
| Lanoconazole | 0.064 | 0.064 | 0.050 | 0.032 - 0.064 |
| Aspergillusflavus (PQ584656-PQ584671) | ||||
| Amphotericin B | 4 | 4 | 3.668 | 2 - 8 |
| Itraconazole | 0.25 | 1 | 0.310 | 0.125 - 1 |
| Voriconazole | 0.5 | 1 | 0.738 | 0.5 - 1 |
| Posaconazole | 0.125 | 0.25 | 0.210 | 0.25 - 1 |
| Isavuconazole | 1 | 4 | 1.476 | 0.5 - 4 |
| Caspofungin | 0.5 | 0.5 | 0.385 | 0.25 - 1 |
| Luliconazole | 0.032 | 0.032 | 0.036 | 0.032 - 0.125 |
| Lanoconazole | 0.032 | 0.032 | 0.051 | 0.032 - 0.25 |
| Aspergillusniger (PQ584672-PQ584684) | ||||
| Amphotericin B | 1 | 1 | 0.898 | 0.5 - 1 |
| Itraconazole | 0.5 | 1 | 0.528 | 0.032 - 1 |
| Voriconazole | 0.5 | 1 | 0.500 | 0.032 - 1 |
| Posaconazole | 0.125 | 0.125 | 0.181 | 0.064 - 0.5 |
| Isavuconazole | 1 | 4 | 1.531 | 0.5 - 4 |
| Caspofungin | 0.125 | 0.25 | 0.293 | 0.125 - 0.5 |
| Luliconazole | 0.032 | 0.032 | 0.035 | 0.032 - 0.125 |
| Lanoconazole | 0.032 | 0.064 | 0.046 | 0.032 - 0.125 |
| Rhizopus arrhizus (PQ577041, PQ577042, PQ582413-PQ582421) | ||||
| Amphotericin B | 0.5 | 1 | 0.567 | 0.25 - 1 |
| Itraconazole | 0.5 | 0.5 | 0.342 | 0.125 - 1 |
| Voriconazole | 4 | 16 | 5.146 | 2 - 16 |
| Posaconazole | 0.25 | 0.5 | 0.266 | 0.125 - 0.5 |
| Isavuconazole | 2 | 2 | 1.763 | 1 - 4 |
| Caspofungin | 8 | 8 | 7.052 | 4 - 8 |
| Luliconazole | 0.25 | 0.25 | 0.194 | 0.032 - 0.25 |
| Lanoconazole | 0.5 | 0.5 | 0.342 | 0.125 - 0.5 |
a The MIC/MEC50 and MIC/MEC90 values were determined as the minimum concentrations of drugs being able to prevent 50 - 90% of the clinical fungal strains, respectively.
b Geometric mean is a mean or average.
All Aspergillus species were susceptible to posaconazole, luliconazole and lanoconazole. Amphotericin B with GM MIC = 0.847 μg/mL and GM MIC = 3.668 μg/mL exhibited the least effect against A. fumigatus and A. flavus, respectively. Isavuconazole with GM MIC = 1.531 μg/mL and caspofungin with GM MEC = 7.052 μg/mL showed the least effect against A. niger and R. arrhizus, respectively. Only three A. flavus isolates were shown to be simultaneously resistant to amphotericin B, itraconazole, and voriconazole. Out of 50 Aspergillus isolates, 3 isolates (6%) of A. fumigatus and 1 isolate (2%) of A. flavus exhibited resistance to caspofungin. All isolates of R. arrhizus were susceptible to luliconazole, lanoconazole, amphotericin B, posaconazole, itraconazole and isavuconazole. Statistical analysis of the results indicated that there was no significant association amongst MIC across different strains relative to antifungal agents (P < 0.05).
5. Discussion
Fungal sinusitis is a common disorder in patients in hot and humid areas (23). Fungal sinusitis is an opportunistic infection that frequently begins in the sinuses and spreads to the eye and skull, and can cause fatal concerns through the brain and meningeal infections (24). The A.fumigatus and A. flavus are the main causative agents of rhinosinusitis as high- lighted by several reports (25-28). Similarly, in current study, Aspergillus spp was report to be the most commonly isolated fungus from FS (14, 29). However, in the United States, especially in the south and southwest, most cases of FS are associated with black fungus agents such as Curvularia, Bipolaris, and Alternaria (30). In accordance with the present study, A. niger and R. arrhizus are highlighted in some reports about FS (31, 32). In present study, the average age of the patients with positive fungal culture was 59, however, these values for Awan et al. (33), Mohammadi et al. (7), Rehman et al. (34), and Badiei et al. (35) studies were 29.49, 46, 33 and 33.89 years, respectively.
In present study, headache (40.1%) and fever (32.8%) were the most common clinical symptoms among patients. However, congestion and headache were the most clinical finding in Mohammadi et al. study (7). Raiesi et al. reported nasal obstruction and headache were most common signs in their cases with fungal rhinosinusitis (27). The reasons for the difference in results could be due to the number of patients studied, the type of FS, the underlying disease, the type of fungal agent, and the geographical region. In present study, two new antifungal drugs, lanoconazole and luliconazole, had potential effects on fungal isolates from FS origin. Similarly, Abastabar et al. found that luliconazole and lanoconazole had the lowest MIC value against susceptible and resistant isolates of A. fumigatus compared with some other antifungals (36). Omran et al. indicated luliconazole and lanoconazole the most effective drugs against clinical and environmental isolates of A. flavus (17). Our results indicated that the GM-MIC value of luliconazole against all tested strains was lower than that of lanoconazole.
A limitation of luliconazole and lanoconazole are no preparation for systemic administration, in vivo studies in animal models have shown that these antifungal drugs are more effective than other drugs for the management of invasive aspergillosis (37). Jain et al. reported that Aspergillus spp isolated from patients with chronic rhinosinusitis and nasal polyps, 100% were susceptible to amphotericin B, itraconazole, and voriconazole (38). Kumar et al. indicated that A. flavus isolated from paranasal sinus fungal infection were susceptible to amphotericin B and itraconazole (39). In contrast to present study, our results of AFST showed that three isolates of A. flavus was resistant to amphotericin B, itraconazole, and voriconazole. A several mechanisms of resistance to azole antifungals are including existence of mutations CYP51A enzyme leading to a decreased drug affinity, overexpression of cyp51A gene (TR34/L98H) producing an increase CYP51A level and overexpression of the genes coding for efflux pump initiating a decreased intracellular accumulation of antifungals (40).
Sriramajayam et al. reported that out of the 68 fungal isolates collected from fungal rhinosinusitis, 75% were resistant to fluconazole, 13.23% to itraconazole, and 2.94% to amphotericin (41). Jain et al. reported the rates of resistance to amphotericin B, itraconazole, and caspofungin in 53 isolates of Aspergillus were 7.55%, 1.88%, and 1.88%, respectively (42). In the present study, out of 50 Aspergillus isolates, 4 isolates (8%) were resistant to caspofungin. The main identified mechanism of clinical isolates of resistance to echinocandins is point mutations in the FKS1 gene, which encodes the antifungal target (43). In Austria reported the MICs range of itraconazole for different isolates as follows: A. flavus (0.5 - 2 μg/mL), A. niger (2 - 4 μg/mL), and Rhizopus species (4 μg/mL) (44). Our results indicated that these values for itraconazole were 0.125 - 1 μg/mL for A. flavus, 0.032 - 1 μg/mL for A. niger, and 0.125 - 1 μg/mL for R. arrhizus. In contrast to present study, Zhou et al. indicated that the MIC50 and MIC90 of isavuconazole against A. flavus were 2 and 2 mg/L, respectively (45).
Our findings demonstrated that luliconazole with GM MIC (0.194 μg/mL) and posaconazole with GM MIC (0.266 μg/mL) were the most effective drugs against R. arrhizus. In line with the present study, Mammen et al. reported the posaconazole GM MIC value of 3.08 μg/mL for 17 isolates of R. oryzae (46). Kachuei et al. reported the GM MICs/MEC value of 2.28 μg/mL for amphotericin B, 10.76 μg/mL for itraconazole, 8.72 μg/mL for voriconazole and 16 μg/mL for caspofungin against of R. oryzae (47). Dannaoui et al. found that azole drugs are considered ineffective against Zygomycetes, and they reported MIC range 0.06 to 1 mg/L for amphotericin B versus Rhizopus spp (48). Consistent with our result study, Diekema et al. reported that caspofungin is generally considered inactive against Rhizopus spp (49). The reasons for the difference between our AFST results with the others studies can be due to the type of strain, geographical region, source of samples, and number of isolates tested.
There were some limitations in present study. First, the investigation of face covers in current study was not comprehensive, the sample size was small during the Covid-19 pandemic and no present data about antifungal therapy of patients. In addition to clinical and paraclinical findings, rapid identification of the causative agents of FS, along with AFST, is an effective in managing FS infection.
5.1. Conclusions
In conclusion, DNA sequencing can be useful for correct identification of filamentous fungi causative agents of FS. In addition, AFST method can be helpful for management patient with FS infection. Our results indicated posaconazole is the most effective antifungal for the management of FS with Aspergillus spp and R. arrhizus as causative agents. Moreover, caspofungin to be a good excellent for the management of FS, exception against Mucorales. The results of the present study showed that the two drugs, luliconazole and lanoconazole, were very effective on fungal isolates, so with further studies in the future, it is hoped that these two drugs can be used to treat FS.