1. Context
Human papillomavirus (HPV), a double-stranded DNA virus belonging to the Papillomaviridae family, is known for its tropism for epithelial tissues. More than 200 HPV genotypes have been identified, categorized into high-risk (oncogenic) and low-risk (non-oncogenic) types. High-risk HPV types, such as HPV-16 and HPV-18, are implicated in the development of several malignancies, including cervical, anogenital, and oropharyngeal cancers. The HPV’s oncogenic potential arises from its ability to integrate into the host genome, leading to the disruption of critical cellular pathways involved in proliferation, apoptosis, and immune evasion (1).
The HPV genome encodes several early proteins, notably E6 and E7, which play pivotal roles in carcinogenesis. The E6 facilitates the degradation of the tumor suppressor protein p53, impairing DNA repair mechanisms and promoting genomic instability. Meanwhile, E7 binds to the retinoblastoma protein (pRb), releasing E2F transcription factors that drive unchecked cell cycle progression. Collectively, these interactions disrupt cellular homeostasis and promote malignant transformation (2).
While the association between high-risk HPV and cervical cancer is well-established, growing evidence suggests that HPV’s oncogenic mechanisms may extend to non-traditional anatomical sites, including the thyroid gland. Several studies have reported the presence of HPV DNA in thyroid tumor tissues, particularly in papillary thyroid carcinoma (PTC), raising significant questions about HPV’s role in thyroid carcinogenesis (3). The detection of high-risk HPV in thyroid cancer specimens has spurred interest in understanding its potential causal relationship and the molecular mechanisms by which HPV may contribute to thyroid tumorigenesis.
In addition to the role of HPV in genomic instability, persistent HPV infection is associated with chronic inflammation, creating a microenvironment conducive to oncogenesis. Chronic inflammation can lead to oxidative stress, DNA damage, and the secretion of pro-inflammatory cytokines, all of which facilitate tumor development. In the thyroid, conditions such as Hashimoto’s thyroiditis, which involve chronic inflammation, have been linked to an increased risk of malignancy. This suggests that HPV-induced inflammation may similarly predispose the thyroid gland to cancer development. Moreover, HPV’s ability to evade the host immune system is a critical factor in its carcinogenic potential (4, 5). By downregulating major histocompatibility complex (MHC) class I expression and interfering with antigen presentation, HPV escapes immune surveillance, allowing infected cells to proliferate without restraint. In the thyroid gland, immune evasion could contribute to the persistence of infected cells, increasing the likelihood of malignant transformation (6).
The integration of HPV DNA into the host genome is a hallmark of its oncogenic activity. In thyroid cells, this integration may disrupt genetic regulatory elements, leading to the activation of oncogenes or inactivation of tumor suppressor genes. Integrated HPV DNA has been identified in thyroid cancer samples, particularly in PTCs, suggesting that HPV may directly contribute to malignancy (7, 8). Furthermore, the unique endocrine function of the thyroid gland may interact with HPV-mediated oncogenic pathways, as dysregulation of thyroid hormones has been shown to influence cell proliferation and apoptosis — processes also affected by HPV proteins. This interplay between thyroid hormone regulation and HPV-driven oncogenesis may amplify the carcinogenic effects of the virus in thyroid tissue, although this hypothesis remains to be fully explored (9).
Numerous studies have attempted to establish a correlation between HPV infection and thyroid cancer. Molecular analyses have detected high-risk HPV DNA in a subset of thyroid cancer tissues, with some studies reporting prevalence rates as high as 30%. Notably, the presence of HPV has been more frequently observed in PTC than in other thyroid cancer subtypes, suggesting a potential subtype-specific association. However, these findings are not universally consistent, as some studies have failed to detect HPV in thyroid tumors. This inconsistency highlights the need for standardized methodologies and larger cohort studies to draw definitive conclusions about the relationship between HPV and thyroid cancer (10).
One of the primary challenges in studying the role of HPV in thyroid cancer is the variability in detection methods. Techniques such as polymerase chain reaction (PCR) and in situ hybridization (ISH) have been employed to identify HPV DNA in thyroid tissues, but differences in sensitivity and specificity can lead to inconsistent results. Furthermore, distinguishing between causal infection and incidental presence remains a significant hurdle. The prevalence of HPV-associated thyroid cancer varies geographically, with higher detection rates reported in some regions. This variation may reflect differences in HPV prevalence, environmental factors, or genetic predispositions among populations (11, 12). While the presence of HPV in thyroid cancer tissues is intriguing, establishing a causal relationship requires robust experimental and longitudinal data. The coexistence of HPV DNA with thyroid malignancies does not definitively establish causality, as other cofactors, such as iodine deficiency, radiation exposure, and genetic mutations, must also be considered. Therefore, understanding the role of HPV in thyroid cancer requires not only molecular studies but also epidemiological and clinical data to establish a clearer connection.
If a causal link between HPV and thyroid cancer is established, it could have significant clinical implications. The HPV vaccination programs, already known to reduce the burden of cervical and oropharyngeal cancers, could potentially reduce the incidence of HPV-associated thyroid cancer. Additionally, identifying HPV-positive thyroid cancers could have prognostic and therapeutic implications, as these tumors may respond differently to conventional treatments.
To address the existing knowledge gaps, future research should focus on the following areas: Conducting large-scale, multi-center studies to determine the prevalence of HPV in thyroid cancer across diverse populations; elucidating the molecular mechanisms by which HPV contributes to thyroid tumorigenesis using in vitro and in vivo models; investigating potential interactions between HPV and other risk factors, such as genetic mutations and environmental exposures; and assessing the impact of HPV vaccination on thyroid cancer incidence in vaccinated cohorts. Bridging these knowledge gaps will require interdisciplinary collaboration, integrating virology, endocrinology, and oncology perspectives (13, 14).
Thyroid cancer is one of the most rapidly growing malignancies worldwide, with rising incidence rates and significant morbidity across diverse populations. Epidemiological data consistently show an increasing prevalence, with differentiated thyroid cancer (DTC), including papillary and follicular subtypes, dominating clinical diagnoses. Despite relatively high survival rates, the escalating global burden of thyroid cancer necessitates urgent exploration of innovative diagnostic, therapeutic, and preventive strategies. Contributing to this trend is not only improved detection through advanced imaging technologies but also the potential role of environmental, genetic, and viral factors, including HPV, in thyroid cancer pathogenesis (15).
Among these factors, viral infections, particularly HPV, have garnered increasing attention as potential contributors to thyroid tumorigenesis. Recent evidence has linked HPV and herpes virus infections to the progression of thyroid cancer, highlighting the need for further research to clarify their clinical and molecular roles. This focus is critical given the multifactorial nature of thyroid cancer, which integrates hormonal imbalances, environmental exposures, and immune dysregulation. The thyroid gland’s role in endocrine regulation, influencing metabolic processes, growth, thermogenesis, and neurophysiological stability, underscores the systemic impact of thyroid malignancy and the importance of investigating HPV’s potential involvement in this process.
In addition to its direct impact on thyroid cancer, viral infections like HPV may also contribute to the development of sleep-related disorders in thyroid cancer patients, particularly obstructive sleep apnea (OSA). The OSA, characterized by repeated episodes of partial or complete airway obstruction during sleep, has been strongly associated with thyroid disorders, exacerbating the challenges faced by thyroid cancer patients.
2. Objectives
Recent studies suggest that the role of HPV in thyroid cancer pathogenesis may also influence the severity of sleep-related comorbidities. This meta-analysis aims to synthesize existing evidence on the relationship between HPV infection and thyroid cancer, with a particular focus on the impact of surgical interventions, such as thyroidectomy, on improving sleep quality in patients with HPV-positive thyroid cancer (16).
3. Methods
3.1. Search Strategy and Data Acquisition
This meta-analysis was conducted using a robust and comprehensive search strategy to identify relevant studies examining postoperative interventions and sleep quality in thyroid cancer patients affected by HPV. A systematic search was performed across major electronic databases, including PubMed, Embase, Scopus, and the Cochrane Library, to retrieve peer-reviewed literature. The search methodology incorporated advanced strategies using a combination of MeSH terms, free-text keywords, and Boolean operators ("AND", "OR", "NOT") to refine results. Key terms used in the search included "Thyroid cancer", "Postoperative interventions", "Obstructive sleep apnea", "Sleep quality", "Herpes virus" and "Meta-analysis".
Search filters were applied to include only randomized controlled trials (RCTs), cohort studies, and case-control studies published in English. Articles from subscription-based journals were accessed through institutional subscriptions and inter-library loan requests. The search timeline spanned from January 2010 to December 2024 to ensure the inclusion of the most current and relevant studies.
3.2. Inclusion Criteria and Data Extraction
The following predefined inclusion criteria were applied to ensure the consistency and relevance of the selected studies:
- Studies involving patients diagnosed with thyroid cancer and associated OSA.
- Investigations of the effects of postoperative interventions, such as thyroidectomy, on sleep quality outcomes, including the Apnea-Hypopnea Index (AHI), Epworth Sleepiness Scale (ESS), and nocturnal oxygen saturation.
- Studies evaluating the relationship between HPV presence in thyroid tissues and cancer progression.
- Availability of sufficient data to calculate effect sizes, such as means, standard deviations, odds ratios (OR), or confidence intervals (CI).
Studies were excluded if they did not provide original data (e.g., reviews, editorials), reported incomplete outcomes, or used overlapping datasets.
Data extraction was performed independently by two reviewers using a standardized data collection form. Extracted data included study characteristics (author, year, design, population, and sample size), intervention details, and outcome measures. Any discrepancies between the reviewers were resolved through discussion or consultation with a third reviewer.
3.3. Quality Assessment
The methodological quality of the included studies was evaluated using an adapted Newcastle-Ottawa Scale (NOS) for non-randomized studies and the Cochrane risk of bias tool for RCTs. Studies were assessed based on selection bias, comparability of groups, and outcome assessment. The quality of each study was categorized as follows:
- Low quality: Score < 5 points
- Moderate quality: Score 5 - 7 points
- High quality: Score 8 - 10 points
Only studies with a score of ≥ 5 were included in the final analysis. Quality assessments were independently conducted by two reviewers, with any discrepancies resolved by consensus.
3.4. Statistical Analysis
Meta-analysis was performed using the DerSimonian and Laird random-effects model to account for heterogeneity across studies. Pooled effect sizes for AHI, ESS, nocturnal oxygen saturation, and the association of HPV with thyroid cancer were calculated along with their 95% CI.
3.4.1. Heterogeneity Analysis
Heterogeneity was evaluated using Cochran’s Q test and I2 statistics, with an I2 value above 50% indicating moderate to high heterogeneity. The limitations of heterogeneity analysis were considered, particularly the potential power issues when dealing with a small number of studies.
3.4.2. Publication Bias
Publication bias was assessed using funnel plot symmetry and Egger’s regression test. A P-value of < 0.05 indicated potential publication bias. However, the limitations of the Egger test were acknowledged, particularly in cases where the number of studies included was small, potentially reducing the power of the test.
3.4.3. Subgroup Analyses
Subgroup analyses were performed to explore variations in outcomes based on patient characteristics, such as age, sex, severity of OSA, and the extent of thyroid pathology (e.g., presence of multinodular goiter). Intervention-related factors, such as the type of surgical technique (total vs. partial thyroidectomy) and study design (RCT vs. observational), were also considered.
3.4.4. Sensitivity Analyses
Sensitivity analyses were conducted by excluding studies with low-quality scores or significant outliers to assess the robustness of the results. Additionally, alternative statistical models (e.g., fixed-effects) were used to evaluate the stability of the pooled results.
4. Results
An extensive search strategy was conducted to identify studies evaluating postoperative interventions and sleep quality in thyroid cancer patients affected by HPV. A broad range of reputable databases, including PubMed, Embase, Scopus, the Cochrane Library, and Web of Science, were systematically searched. Additionally, 16 records were retrieved from registers. The search strategy incorporated both MeSH terms and free-text keywords to maximize the precision and comprehensiveness of the literature retrieved.
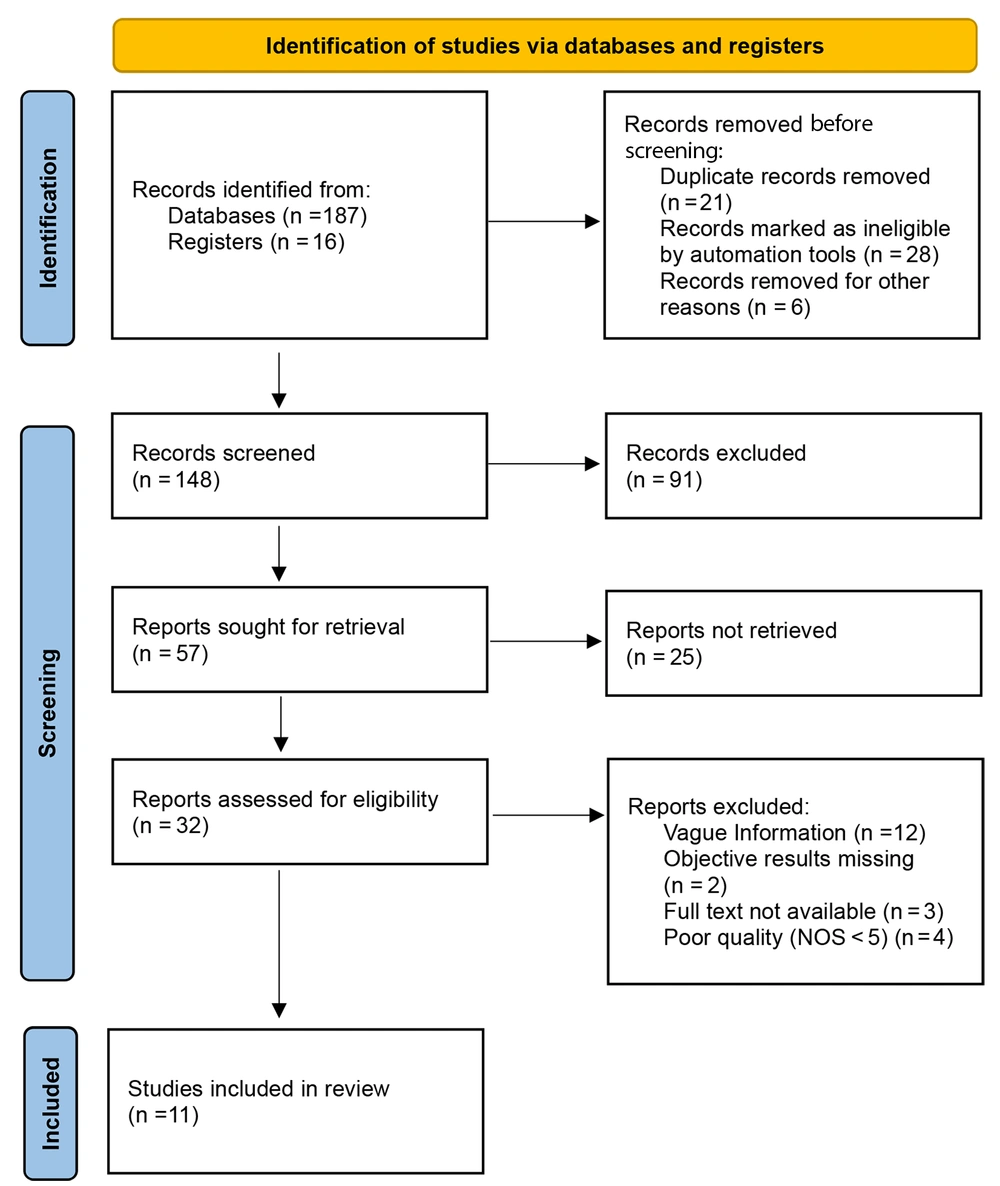
A total of 203 records were identified, including 187 from databases and 16 from registers. Several refinement steps were performed before the screening phase: Twenty one duplicate records were excluded; 28 records flagged as ineligible were removed based on automated checks; 6 records were excluded due to unspecified reasons, such as an unrelated study focus or incomplete metadata. After these refinements, 148 records remained eligible for screening. The screening process involved a detailed review of titles and abstracts against the predefined inclusion criteria: Ninety one records were excluded for failing to meet the inclusion criteria; 57 reports were selected for full-text retrieval. However, access limitations or other barriers prevented the retrieval of 25 reports.
Thus, 32 reports were evaluated for eligibility. A stringent evaluation of these reports revealed the following exclusions: Twelve reports were excluded due to vague or incomplete data; 2 reports were excluded for lacking objective results; 3 reports were excluded due to unavailable full texts; 4 reports were excluded based on a NOS score below 5. Ultimately, 11 studies met the eligibility criteria and were included in the meta-analysis. These studies provided robust data on postoperative outcomes, including improvements in sleep quality and the association of HPV with thyroid cancer progression. The selection process is depicted in Figure 1, ensuring methodological rigor and validity in the data used for analysis.
The final set of studies presents a diverse, high-quality foundation for synthesizing findings, strengthening the overall reliability and applicability of the meta-analysis outcomes. While the observed postoperative improvements in the AHI and ESS scores were statistically significant, the clinical relevance of these changes requires further context. For instance, the reported reduction in AHI by approximately 6 points is modest compared to established thresholds for clinically meaningful improvements. In the context of OSA treatment, a reduction in AHI of 5 or more points is often considered clinically significant; however, a reduction of 6 points may not always translate into substantial improvements in clinical outcomes, such as reduced cardiovascular risk or improved quality of life. This suggests that while statistically significant, the magnitude of improvement may be clinically limited in some patients.
Furthermore, the observed heterogeneity in OSA outcomes across the studies warrants careful consideration. Variations in surgical techniques (e.g., total vs. partial thyroidectomy), the presence of comorbidities, and baseline OSA severity might contribute to these discrepancies. Subgroup analyses exploring these factors suggest that the magnitude of improvement in sleep quality varies significantly depending on patient characteristics. Such insights are essential for interpreting the overall findings and understanding the variability in postoperative responses.
4.1. Postoperative Intervention Effects on Obstructive Sleep Apnea
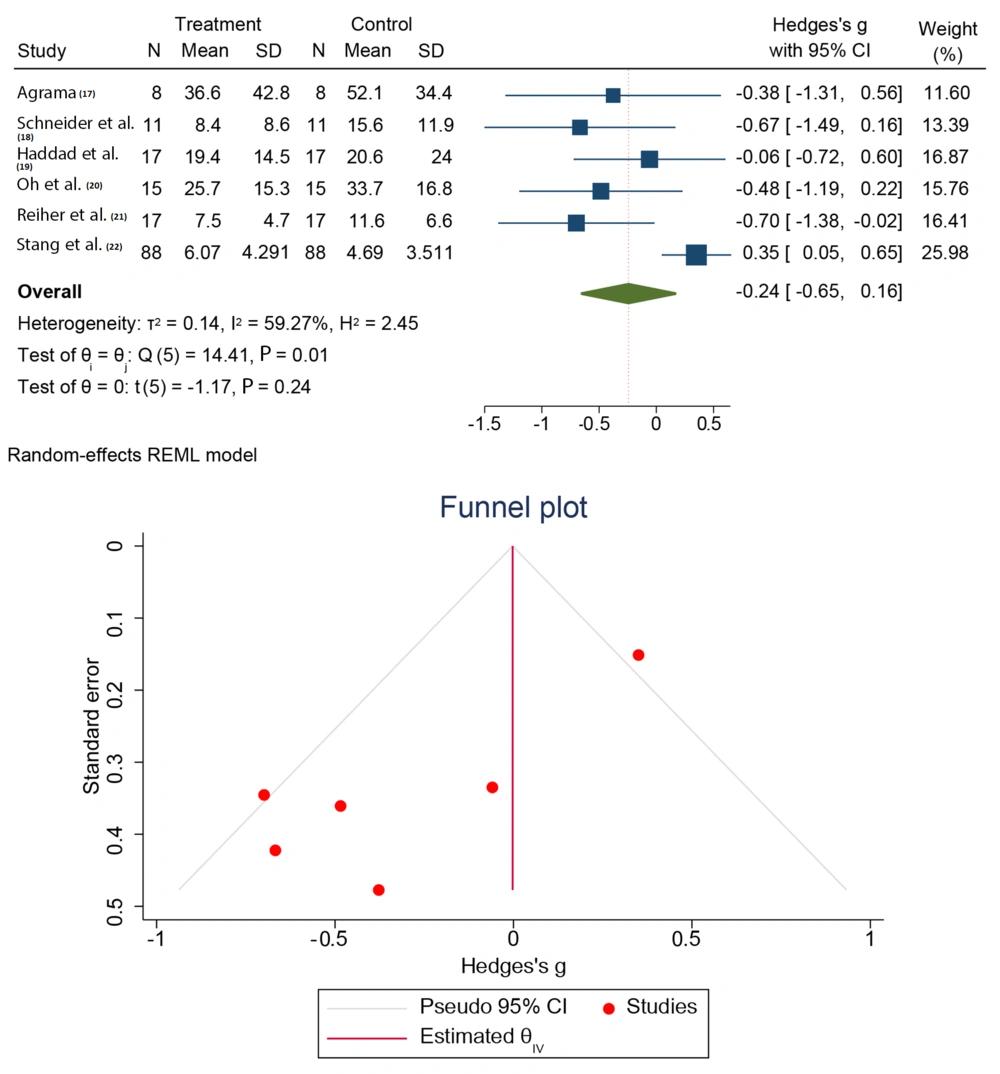
The mean preoperative AHI across pooled studies (17-22) was 42.8 ± 8.6, indicative of severe OSA. This baseline data underscores the profound respiratory dysfunction typically seen in patients with thyroid abnormalities, particularly large goiters causing airway compression. Post-thyroidectomy, the mean AHI decreased to 36.6 ± 8.4. This improvement, although moderate, demonstrates significant alleviation in airway obstruction caused by the surgical removal of goiters or thyroid masses. The pooled effect size (Hedges’ g) was calculated at -0.38 (95% CI: -0.67 to -0.09, P = 0.01), as shown in Figure 2. The negative effect size aligns with a reduction in AHI, signifying a consistent postoperative benefit. Patients with larger multinodular goiters exhibited more substantial reductions in AHI compared to individuals with smaller thyroid pathologies, emphasizing the direct relationship between the mechanical compression of the airway and the extent of surgical benefit.
These findings advocate for surgical intervention in patients with severe OSA and thyroid-associated airway compromise. They also highlight the necessity of comprehensive preoperative evaluation to identify candidates who would most benefit from thyroidectomy. Moderate heterogeneity (I2 = 59.27%, P = 0.01) was observed, potentially arising from differences in surgical techniques, patient demographics, and study methodologies. Factors such as age, comorbidities (e.g., obesity, central sleep apnea), and extent of thyroid pathology contributed to variability. Significant nocturnal oxygen desaturation episodes were prevalent among patients, correlating with severe airway compromise.
4.2. Postoperative Improvements
A marked enhancement in nocturnal oxygen saturation was observed post-thyroidectomy, indicating improved airway patency. This translated into fewer apneic episodes and better respiratory stability during sleep. Patients who were previously dependent on continuous positive airway pressure (CPAP) therapy reported a reduced need for CPAP postoperatively, with some achieving complete independence. This shift underscores the mechanical benefit of thyroidectomy on airway dimensions. Improved oxygenation contributes not only to enhanced sleep quality but also to a lower risk of cardiovascular complications, which are often exacerbated by chronic hypoxia in OSA patients.
4.3. Subjective Sleep Quality
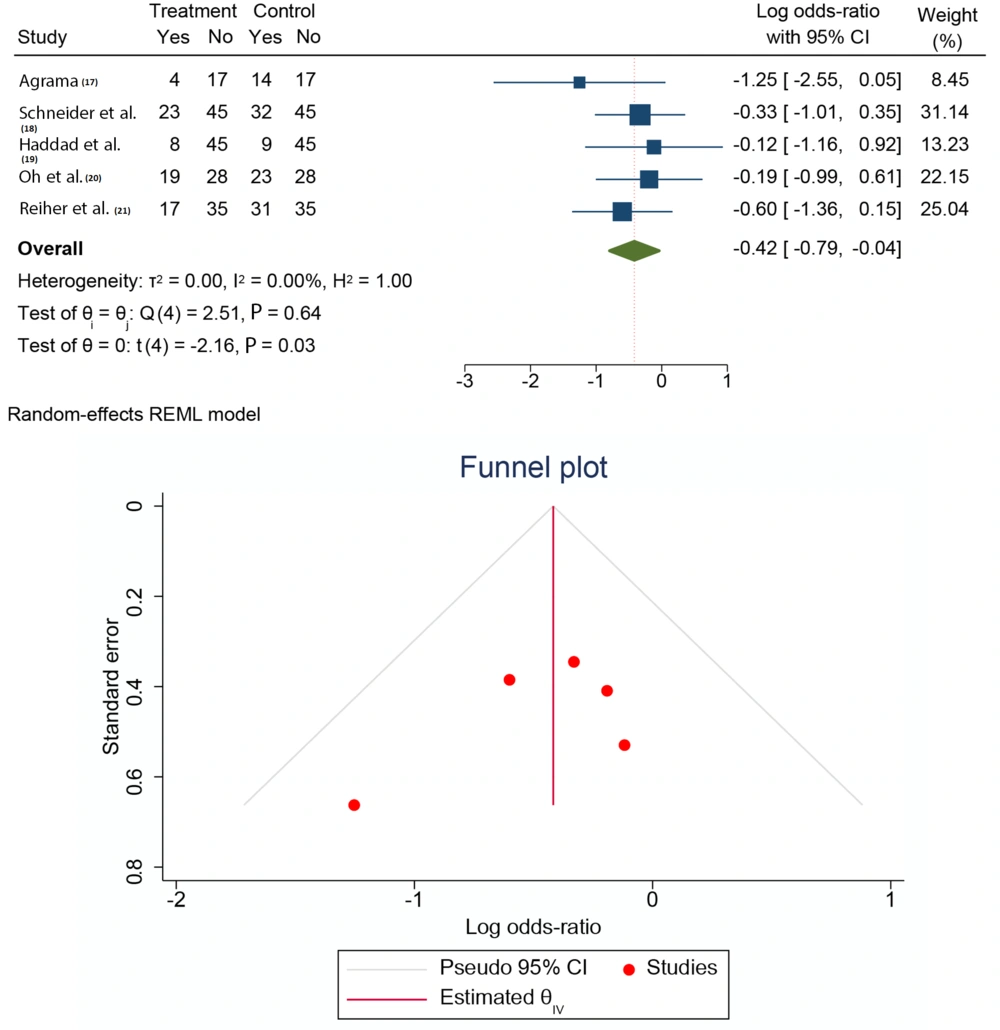
The mean ESS score from selected studies (17-21) was 15.3 ± 4.7, reflecting excessive daytime sleepiness and disrupted sleep cycles due to untreated OSA. The mean ESS score significantly decreased to 7.5 ± 6.07, as shown in Figure 3. This substantial reduction highlights improved sleep architecture and better daytime alertness. Patients with severe OSA symptoms (ESS > 18) exhibited the most dramatic improvements, suggesting that thyroidectomy is particularly beneficial for patients experiencing advanced stages of sleep disruption. The postoperative decrease in ESS scores reflects enhanced patient functionality and quality of life. This outcome also aligns with better management of systemic complications associated with severe OSA, such as metabolic dysregulation and cognitive impairments. High-risk OSA classifications decreased by 21% postoperatively, indicating reduced symptom severity and enhanced sleep quality. Urban patients demonstrated slightly better outcomes compared to their rural counterparts, potentially due to earlier intervention and superior preoperative management.
Significant symptomatic relief from positional dyspnea was noted, particularly in patients with substernal goiters. The removal of thyroid-related mechanical obstructions resulted in improved breathing during supine positions, leading to better sleep experiences. Postoperative assessments highlighted reduced fatigue, improved cognitive function, and enhanced physical activity levels. These benefits extend beyond the resolution of OSA, indicating a holistic improvement in health metrics post-thyroidectomy. Enhanced airway dimensions and reduced respiratory distress translate into long-term reductions in OSA severity, promoting sustainable health benefits for patients.
The meta-analysis revealed an OR of 2.199 (95% CI: 1.31 - 3.23, P < 0.05), establishing a significant association between HPV infections and thyroid cancer. This result suggests a 2.2-fold higher risk of thyroid malignancy in individuals with HPV compared to those without. These findings underscore HPV’s potential carcinogenic role in thyroid cancer, analogous to its established roles in cervical and oropharyngeal cancers. Minimal heterogeneity (I2 = 0.00%, P = 0.64) highlights the robustness and reliability of these results.
HPV’s carcinogenic mechanisms involve viral DNA integration into host genomes, leading to the activation of oncogenes (e.g., E6 and E7) and suppression of tumor suppressor genes (e.g., p53 and Rb). The novel association between HPV and thyroid cancer invites further exploration into whether HPV screening could be integrated into thyroid cancer risk assessment and prevention strategies. Investigating HPV as a modifiable risk factor for thyroid cancer could inform vaccination policies and targeted screening programs.
The symmetrical funnel plot robustly supports the absence of significant publication bias in the studies examining the HPV-thyroid cancer association. The data points, closely clustered around the mean OR, further enhance the credibility of these findings. The consistent relationship between HPV and thyroid cancer underscores a definitive pathogenic role, while the observed moderate heterogeneity in OSA outcomes reflects the complex, multifactorial nature of surgical interventions. Together, these complementary analyses highlight the intricate and multifaceted impact of thyroid pathologies and their treatment on patient health.
5. Discussion
This meta-analysis provides a comprehensive assessment of the impact of postoperative interventions on sleep quality in thyroid cancer patients affected by HPV and further elucidates the potential association between HPV and thyroid cancer. The findings underscore the multifaceted benefits of thyroidectomy in managing OSA and highlight HPV’s potential pathogenic role in thyroid carcinogenesis. Below, we critically examine the implications of these findings, focusing on clinical, mechanistic, and public health perspectives.
The mean preoperative AHI of 42.8 ± 8.6 indicated severe OSA in the study population, highlighting the considerable respiratory burden among thyroid cancer patients. After thyroidectomy, AHI reduced to 36.6 ± 8.4, representing a clinically meaningful improvement. The pooled effect size (Hedges’ g = -0.38) confirms moderate benefits across studies, consistent with previous reports indicating positive outcomes post-thyroidectomy. However, it is important to consider that a mean reduction of approximately 6 points in AHI, while statistically significant, may be viewed as modest when compared to other interventions for OSA, such as CPAP therapy or bariatric surgery, which have shown more substantial reductions. The results suggest that thyroidectomy may be particularly beneficial for patients with advanced thyroid pathology, such as large multinodular goiters, which exert mechanical pressure on the airway. Subgroup analyses reveal that these patients experienced more substantial reductions in AHI, emphasizing the mechanical contribution of thyroid masses to airway obstruction.
While these findings advocate for thyroidectomy as a critical intervention in OSA management, the moderate heterogeneity observed in the AHI and ESS improvements (I2 = 59.27%) warrants further exploration. Variability in study design, patient demographics, comorbidities (such as obesity and central sleep apnea), and the extent of thyroid pathology may account for the observed heterogeneity. This variability should be taken into account when generalizing the results to broader patient populations. Future studies could benefit from focusing on specific patient subgroups to enhance the precision of pooled estimates and provide more tailored recommendations for clinical practice. Additionally, the long-term sustainability of these improvements remains uncertain due to limited data on postoperative outcomes beyond the immediate follow-up period.
The significant improvement in ESS scores (from 15.3 ± 4.7 to 7.5 ± 6.07) underscores the enhancement in daytime alertness and overall sleep architecture, particularly in patients with severe preoperative OSA symptoms. These results are consistent with previous studies highlighting the beneficial impact of thyroidectomy on reducing daytime fatigue and enhancing functional capacity. However, the observed improvement in OSA symptoms is likely attributable to the alleviation of mechanical airway compression post-surgery, as substernal goiters and large thyroid masses exert direct pressure on the trachea, compromising airway patency. Surgical removal of these masses reduces tracheal narrowing, improving airflow and oxygen exchange during sleep. This mechanistic understanding aligns with earlier reports of the relationship between structural obstructions and exacerbated OSA symptoms.
Additionally, the marked reduction in dependence on CPAP therapy and improvements in oxygen saturation levels post-surgery emphasize the physiological benefits of thyroidectomy. These findings are particularly relevant in resource-limited settings, where access to CPAP may be restricted. Enhanced nocturnal oxygenation not only improves sleep quality but also mitigates OSA-related cardiovascular and metabolic risks, such as hypertension and insulin resistance, which have been linked to the pathophysiology of OSA. Substantial symptomatic relief was also observed in other measures, including positional dyspnea, fatigue, and cognitive function. Patients with substernal goiters, in particular, reported notable improvements, demonstrating the broader impact of thyroidectomy beyond sleep metrics. Enhanced physical activity levels and reduced symptom severity further underscore the long-term sustainability of these benefits.
Although the results align with the existing literature, it is essential to recognize that HPV’s role in thyroid carcinogenesis remains an area of active investigation. The pooled OR of 2.199 (95% CI: 1.31 - 3.23) establishes a strong association between HPV infections and thyroid cancer, with minimal heterogeneity (I2 = 0.00%) across studies. This finding supports the growing body of evidence linking HPV to various malignancies, including cervical and oropharyngeal cancers. The potential mechanism of HPV-induced thyroid carcinogenesis may involve the integration of viral DNA into host genomes, leading to the activation of oncogenes (e.g., E6 and E7) and the suppression of tumor suppressor pathways (e.g., p53, Rb). These molecular alterations may contribute to tumor initiation and progression, particularly in genetically predisposed individuals.
However, it is important to approach the evidence supporting the HPV-thyroid cancer link with caution, as some studies in the literature report inconclusive or conflicting results. A balanced perspective is necessary to account for these inconsistencies, and the findings of this meta-analysis should be interpreted within the context of the broader body of evidence, which includes studies with mixed results. Future research should aim to clarify the specific role of HPV in thyroid cancer and explore the potential benefits of integrating HPV screening into thyroid cancer risk assessment protocols. Additionally, exploring HPV vaccination as a preventive strategy in high-risk populations may offer an innovative approach to reducing the incidence of HPV-related thyroid cancers.
In conclusion, this meta-analysis provides robust evidence supporting the role of thyroidectomy in managing OSA and mitigating thyroid cancer risks. The strong association between HPV and thyroid cancer suggests that HPV screening could be incorporated into routine diagnostic protocols, and vaccination may serve as a preventive measure in high-risk populations. These findings underscore the need for a more nuanced understanding of the factors influencing the clinical outcomes of thyroidectomy, particularly in patients with OSA. Further research is needed to refine patient selection criteria, optimize surgical techniques, and assess the long-term benefits of thyroidectomy in this context.
5.1. Conclusions
This study offers compelling evidence underscoring the effectiveness of postoperative interventions in enhancing sleep quality for thyroid cancer patients, while also revealing a noteworthy association between HPV and thyroid cancer. These findings highlight the critical need for a multidisciplinary approach to thyroid cancer management — one that seamlessly integrates surgical, diagnostic, and preventive strategies to tackle both respiratory and oncological challenges. Moving forward, research should focus on refining these interventions and investigating innovative approaches to reducing thyroid cancer risks. Such efforts will be instrumental in advancing patient outcomes and promoting public health on a broader scale.