1. Background
Influenza, caused by viruses of the Orthomyxoviridae family, is a significant global health concern that leads to seasonal epidemics and occasional pandemics (1). Globally, seasonal influenza contributes to an estimated 290,000 to 650,000 respiratory deaths annually (2, 3). Among children under five with influenza-related lower respiratory tract infections, an overwhelming 99% of deaths occur in developing countries (3). Influenza A and B viruses are the primary contributors to human disease, with influenza A being more virulent due to its capacity for antigenic shift and drift (4). These mechanisms facilitate the evasion of immune responses, resulting in annual outbreaks and necessitating periodic vaccine reformulation (5).
The public health impact of seasonal influenza is particularly pronounced among healthcare workers, such as nurses, who are at elevated risk due to occupational exposure and their critical role in patient care. Healthcare workers, including nurses, represent a frontline defense in managing influenza outbreaks, making them a priority group for seasonal influenza vaccination. Unlike some countries where seasonal influenza vaccination for healthcare workers is either voluntary or strongly recommended, it is compulsory in Saudi Arabia (6). This mandatory policy is designed to reduce the transmission of influenza within healthcare facilities, safeguarding both healthcare workers and their patients. Compliance requires either proof of annual vaccination or a medical exemption issued by a licensed physician (6).
In resource-limited settings or where vaccine uptake is suboptimal, naturally acquired immunity becomes an essential component of protection against influenza. Antibody prevalence studies among nurses provide valuable insights into the dynamics of infection and immunity in this high-risk group. This is especially relevant in Saudi Arabia, where healthcare professionals frequently encounter diverse patient populations due to the country’s central role in hosting millions of pilgrims annually for Hajj and Umrah (7). The potential introduction of new, unrecognized circulating strains during this annual religious practice could impact the effectiveness of seasonal influenza vaccines, as such strains may not be included in the vaccine formulation (8, 9).
Despite the importance of influenza immunity, there is limited research on the seroprevalence of seasonal influenza antibodies among healthcare workers in Saudi Arabia, particularly among nurses. Studies have primarily focused on influenza vaccination knowledge, attitudes, and practices (10, 11). A growing body of evidence suggests that the ABO and Rhesus (Rh) blood group systems may influence susceptibility to infectious diseases, including viral infections (12). Blood group antigens, which are expressed on red blood cells and various epithelial and endothelial tissues, may modulate the interaction between host cells and pathogens (13, 14). For instance, certain studies have reported associations between ABO blood groups and susceptibility to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (14, 15). More recently, a study observed significantly higher influenza A than influenza B antibody levels among unvaccinated individuals with the O+ blood group, suggesting a potential role of blood group phenotypes in influenza immunity (16). Furthermore, an inverse relationship was found between age and influenza B IgG levels, reinforcing the influence of host factors on serological outcomes.
2. Objectives
Despite these findings, the relationship between ABO and Rh blood groups and influenza remains insufficiently explored, particularly within Middle Eastern populations. Therefore, this study aims to assess the prevalence of antibodies against influenza A and B viruses among nurses in Saudi Arabia and to investigate potential associations with ABO and Rh blood group phenotypes.
3. Methods
3.1. Participants and Sample Collection
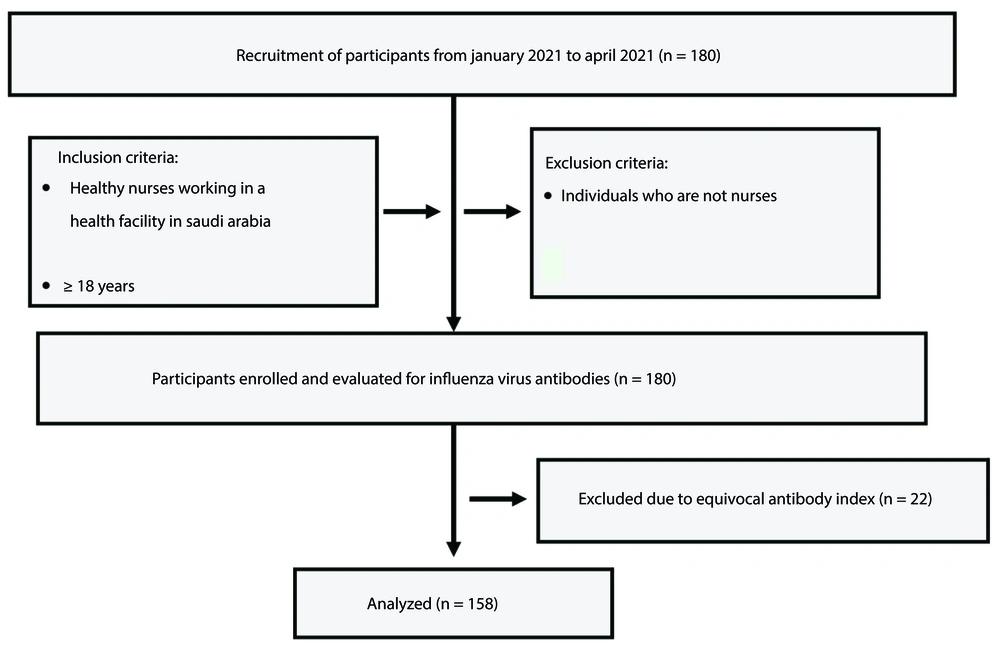
This study was conducted between January and April 2021 using a simple random sampling method. Eligibility was limited to healthy nurses aged 18 years and older who were employed at a medical facility in Najran. Individuals under 18 years of age and those not working in the nursing profession were excluded. A total of 180 participants were recruited to assess the presence of influenza virus antibodies (Figure 1). Participants were from four healthcare facilities in Najran, the capital city of Najran province in the southwest of Saudi Arabia. The facilities included Specialized Najran Hospital, King Khalid Hospital, Najran General Hospital, and the Maternity and Children’s Hospital. Demographic data, such as age, gender, nationality, and influenza vaccination status, were collected using a structured questionnaire. Venous blood samples (5 mL) were obtained from each participant using plain tubes. The serum was separated, aliquoted into 1.5 mL tubes, and stored at -20°C until analyzed for antibody levels.
3.2. Influenza Immunoglobulin G Detection
The levels of influenza A and B immunoglobulin G (IgG) in the samples were measured using enzyme-linked immunosorbent assay (ELISA) following the manufacturer’s protocol (Vircell, Granada, Spain; catalog numbers G/M1007-EN-02 and G/M1008-EN-02, respectively). Briefly, 100 μL of serum diluent was added to each well, followed by 5 μL of control samples and test sera. After the addition of reagents, incubation, and washing steps, the ELISA plates were analyzed using the SPECTROstar Nano absorbance reader (BMG Labtech, Germany) at 450/620 nm. Potential confounding factors were minimized by strictly adhering to sample quality standards, including the exclusion of repeatedly freeze-thawed, hemolyzed, lipemic, or contaminated samples. The IgG levels in each sample were expressed as an Antibody Index, calculated using the formula: Antibody Index = (Sample OD/Cut-off serum mean OD) × 10. According to the kit guidelines, an Antibody Index below 9 is classified as negative, an index above 11 as positive, and values between 9 and 11 as equivocal. Equivocal samples were excluded from the analysis.
3.3. Determination of Participants’ Blood Group
ABO and Rh blood group testing was performed using the IH-500 fully automated blood typing system (Bio-Rad Laboratories Inc., USA). This system provides in vitro serological analysis for blood grouping and antibody detection based on results from gel card images.
3.4. Statistical Analyses
The data were assessed for normality before analysis and evaluated using appropriate statistical methods. Categorical variables were analyzed using the chi-square test. The relationship between the influenza IgG Index and participants’ blood groups was examined using the Kruskal-Wallis test, as the normality test revealed that the data were not normally distributed. Similarly, the non-parametric measure, Spearman’s rank correlation test, was employed to assess the association between the influenza IgG Index and participants’ age. All statistical analyses were performed using GraphPad Prism, version 10.0. Statistical significance was defined as P < 0.05.
4. Results
4.1. Characteristics of the Study Participants
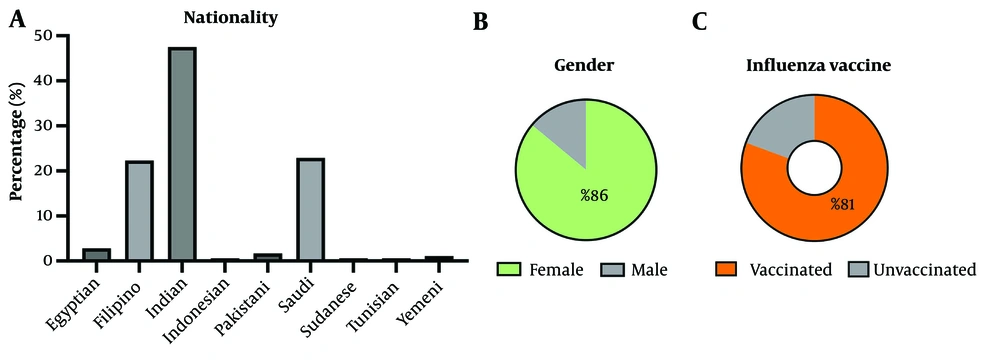
The study participants were adults aged 25 to 62 years, with the majority being female (86%) (Figure 2). The group comprised Saudi and non-Saudi nurses working in healthcare facilities across Najran, with Indians representing the largest proportion (47.5%). Most participants reported having received the influenza vaccine (Figure 2).
4.2. Influenza A and B Immunoglobulin G Antibodies Serological Status and Association with Demographic Factors
All study participants (n = 180) were tested for influenza A and B IgG antibodies. Samples with equivocal results for influenza A (22 out of 180) and influenza B (22 out of 180) were excluded from further analysis, leaving 158 participants for evaluation for each of the influenza types. A moderate seropositivity of influenza A and B antibodies (51.6% and 56.3%, respectively) was found. Overall, seropositive cases outnumbered seronegative ones, with a higher proportion of participants testing positive for influenza B compared to those testing negative across both genders (Table 1). However, among males, seronegativity for influenza A was more prevalent. In terms of age groups, participants aged 21 - 30 years showed a notably higher proportion of seropositive cases compared to their seronegative counterparts for both influenza A and B (Table 1). Among Saudi participants, the proportion of seronegative individuals exceeded that of seropositive individuals for both influenza A and B, in contrast to the trend observed among non-Saudi participants. Despite these observations, no statistically significant associations were identified between serological status and the demographic factors analyzed.
| Parameters | Influenza A | Influenza B | ||||
|---|---|---|---|---|---|---|
| IgG Positive (%) | IgG Negative (%) | P-Value | IgG Positive (%) | IgG Negative (%) | P-Value | |
| Gender | 0.3894 | 0.2675 | ||||
| Male | 9 (5.73) | 12 (7.64) | 16 (10.13) | 8 (5.06) | ||
| Female | 72 (45.86) | 64 (40.76) | 73 (46.20) | 61 (38.61) | ||
| Total | 81 (51.59) | 76 (48.41) | 89 (56.33) | 69 (43.67) | ||
| Age | 0.4327 | 0.2739 | ||||
| 21 - 30 | 39 (25.16) | 28 (18.06) | 42 (27.27) | 25 (16.23) | ||
| 31 - 40 | 31 (20.00) | 34 (21.94) | 37 (24.03) | 27 (17.53) | ||
| > 40 | 11 (7.10) | 12 (7.74) | 10 (6.49) | 13 (8.44) | ||
| Total | 81 (52.26) | 74 (47.74) | 89 (57.79) | 65 (42.21) | ||
| Nationality | 0.1472 | 0.0744 | ||||
| Saudi | 15 (9.55) | 22 (14.01) | 15 (9.55) | 20 (12.74) | ||
| Non-Saudi | 65 (41.40) | 55 (35.03) | 73 (46.50) | 49 (31.21) | ||
| Total | 80 (50.96) | 77 (49.04) | 88 (56.05) | 69 (43.95) | ||
Seroprevalence of Influenza A and B Virus Immunoglobulin G Antibodies Among Nurses with Respect to Demographic Factors a
4.3. Comparison of Influenza A and B Immunoglobulin G Antibody Levels Based on Vaccination Status Among Seropositive Participants
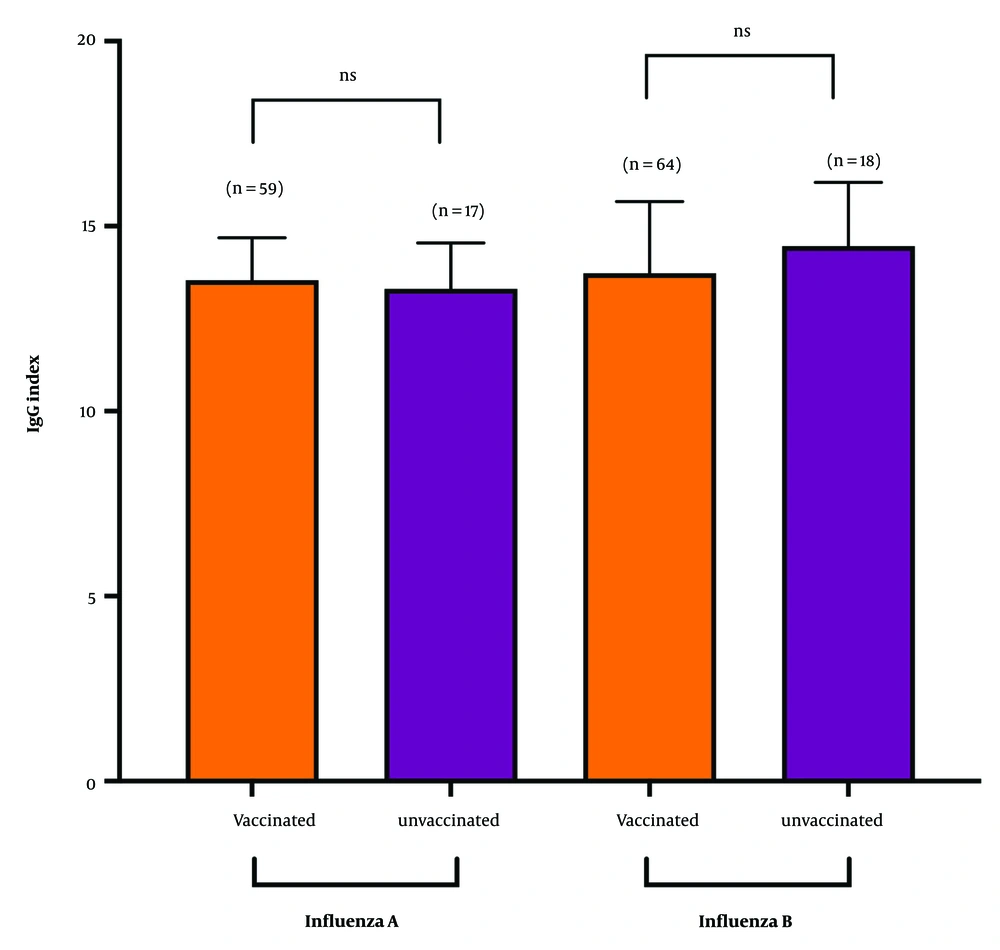
We examined whether antibody levels among seropositive participants varied based on their vaccination status. Of the participants who provided vaccination information, approximately 82% reported being vaccinated. Analysis revealed that influenza A antibody levels, represented by the IgG Index, were comparable between seropositive vaccinated (13.54 ± 1.14) and unvaccinated individuals (13.31 ± 1.24) (Figure 3). For influenza B, antibody levels were lower in vaccinated participants compared to their unvaccinated counterparts. However, these differences in antibody levels between vaccinated and unvaccinated groups were not statistically significant for either influenza A or B (P > 0.05).
Influenza immunoglobulin G (IgG) seropositivity among vaccinated and unvaccinated subjects. Numbers in parentheses indicate the count of seropositive participants. The IgG Index between these groups was compared using the Mann-Whitney test, and results showing no significant differences were marked as "ns".
4.4. Association Between Influenza Antibody Levels and the ABO/Rh Blood Group of the Seropositive Subjects
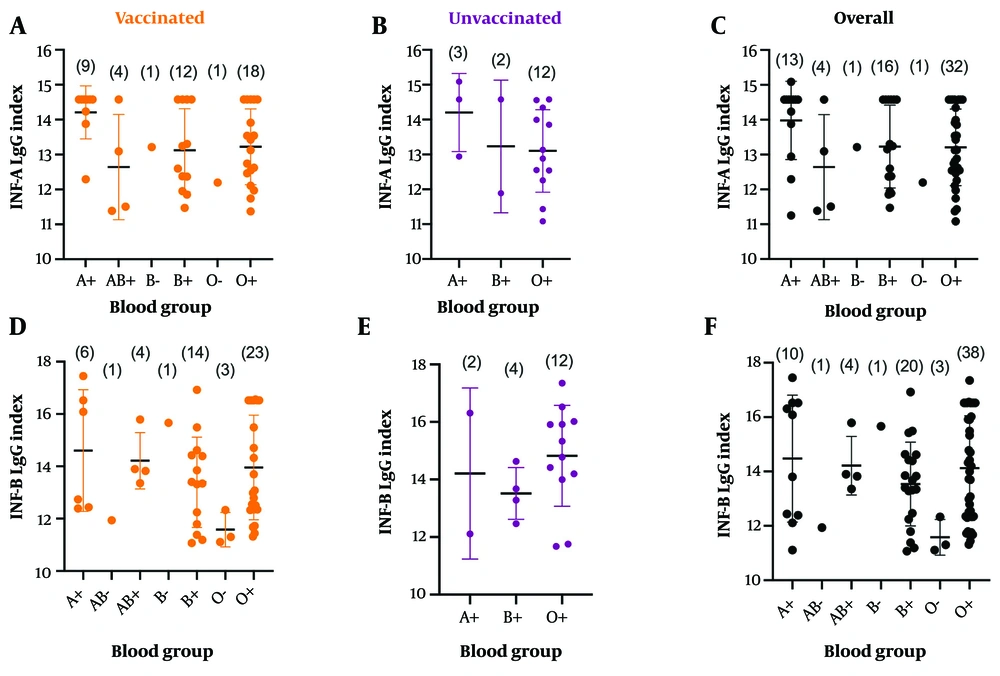
The relationship between influenza antibody levels and participants’ blood groups was further examined. Of the 158 participants with confirmed antibody results, blood group data was unavailable for 20 individuals assessed for influenza A antibodies and 19 for influenza B antibodies. These participants were excluded from the analysis evaluating the association between blood group and antibody prevalence to ensure accurate and reliable results. For both influenza A and B, individuals with the A+ blood group exhibited the highest average antibody levels compared to other groups (Figure 4). Interestingly, among unvaccinated participants, those with the O+ blood group showed higher average antibody levels for influenza B. However, the differences in antibody levels across various blood groups were not statistically significant.
Association between influenza antibody levels of seropositive subjects and their blood groups. A - C, represents analyses conducted for influenza A (INF-A) antibody levels; while D - F, represents those conducted for INF-B antibody levels. Kruskal-Wallis test was used. No significant difference was identified.
4.5. Correlation Between Influenza Antibody Levels and the Age of Seropositive Subjects
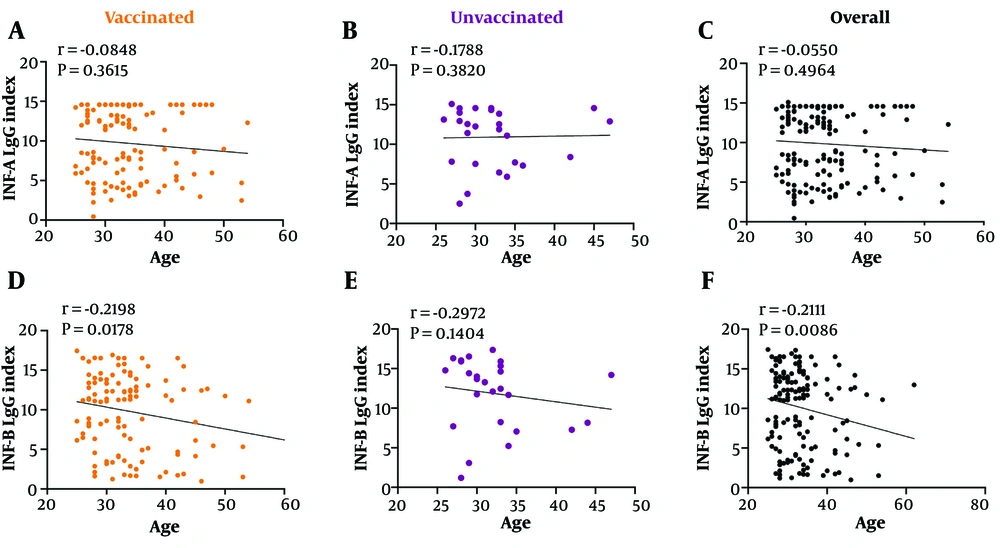
To evaluate the relationship between antibody levels and the ages of seropositive participants, a Spearman correlation analysis was conducted (Figure 5). A negative correlation was identified for both influenza A and B antibody levels in relation to participants’ age. Notably, unlike influenza A antibody levels, influenza B antibody levels showed a significant negative correlation with age (r = -0.2111, P = 0.0086) (Figure 5F). This significant correlation was also evident within the vaccinated subgroup (r = -0.2198, P = 0.0178) (Figure 5D).
Correlation between influenza antibody levels and the age of seropositive subjects. A - C, represents analyses conducted for influenza A (INF-A) antibody levels; while D - F, represents those conducted for INF-B antibody levels. Spearman correlation analysis was conducted. The INF-B levels significantly correlated.
5. Discussion
This study revealed a moderate seroprevalence of influenza antibodies among nurses, with a notable proportion being seropositive for both influenza A and B. Interestingly, our findings indicated a slightly higher seropositivity rate for influenza B compared to influenza A. This pattern aligns with a study conducted among children in the United Arab Emirates, which also reported greater seroprevalence for influenza B (17). In contrast, a study from Thailand involving older adults aged 60 to 95 years demonstrated a higher prevalence of influenza A (18). These contrasting observations highlight the variability in population-level immune responses to different influenza virus subtypes, potentially influenced by factors such as age, regional virus circulation patterns, and previous exposure histories (19, 20). Despite the differences in seroprevalence across gender, age groups, and nationality, no significant associations were observed in this study, underscoring the multifactorial nature of influenza immunity. Additionally, this finding may be attributed to the relatively homogenous occupational environment and lifestyle of the participants, who share similar exposure risks and vaccination practices.
Interestingly, the youngest age group (21 - 30 years) exhibited higher seropositivity rates for both influenza A and B. This could reflect differences in exposure or immune response dynamics, as younger healthcare workers might have more frequent interactions with patients or exhibit stronger immune responses compared to older counterparts (21). The absence of significant gender-based differences suggests that both the male and female study cohort are equally exposed and susceptible to influenza. Approximately 82% of the participants with definite antibody results reported receiving the influenza vaccine, with seropositive vaccinated individuals demonstrating comparable influenza A IgG levels to their unvaccinated counterparts. However, influenza B antibody levels were slightly lower among vaccinated participants, although this difference was not statistically significant. These findings suggest that natural infection may play a crucial role in maintaining higher antibody levels, particularly for influenza B, in settings with suboptimal vaccine efficacy or uptake (22, 23). Furthermore, the absence of significant differences in antibody levels between vaccinated and unvaccinated groups suggests that both natural and vaccine-induced immunity contribute comparably to overall seropositivity.
Exploring the relationship between ABO and Rh blood groups and influenza antibodies revealed interesting, though not statistically significant, trends. For both influenza A and B, individuals with the A+ blood group exhibited the highest antibody levels, while among unvaccinated participants, those with the O+ blood group showed elevated levels of influenza B antibodies. The reason behind the elevated influenza B antibody levels in unvaccinated participants with the O+ blood group remains unclear. This observation may suggest a greater natural exposure or a stronger innate immune response to influenza B in this group. However, current evidence on the role of ABO blood groups in shaping immune responses, particularly against influenza viruses, is scarce and inconclusive. This highlights the need for further research to explore underlying genetic and immunological factors that could account for such patterns.
Nonetheless, prior studies have indicated similar associations between blood groups and susceptibility to infectious diseases, including SARS-CoV-2, where group A individuals were reported to have increased risks of infection, potentially due to differences in antigen expression and immune modulation (14, 15). Although the role of blood groups in influenza remains less established, the observed trends warrant further investigation with larger, more diverse cohorts to confirm or refute these associations. Additionally, our findings underscore the importance of reporting results irrespective of statistical significance, particularly in under-researched areas, as they contribute valuable data that may inform future investigations and cumulative evidence.
Upon probing the association between antibody levels and age, a negative correlation was observed between age and influenza B antibody levels, with older participants showing lower antibody levels. This relationship was particularly significant among vaccinated individuals, suggesting an age-related decline in immune responses to influenza B. Such findings are consistent with immunosenescence, the gradual weakening of the immune system with age, which may affect vaccine efficacy and natural immunity (24, 25). Given that healthcare workers play a crucial role in infection control, these age-related variations underscore the need for tailored vaccination strategies within this group. For instance, the use of high-dose or adjuvanted influenza vaccines may be more effective for older healthcare workers, helping to overcome diminished immune responses and ensure sustained protection. Implementing such targeted approaches could enhance occupational health programs and reduce influenza-related morbidity in healthcare settings.
Continuous surveillance is critical in addressing the ongoing challenges posed by influenza infections in Saudi Arabia. The establishment of the Sentinel Surveillance Program in 2017 and the subsequent implementation of the Integrated Influenza Sentinel Surveillance System (IISS) across the country have significantly enhanced monitoring and response efforts. However, greater focus is needed on Najran, a region bordering Yemen, where cross-border interactions pose unique public health challenges. Yemen’s limited capacity for influenza surveillance increases the risk of unmonitored virus transmission, which can have serious health implications for Najran’s population. Strengthening surveillance in this high-risk area is essential to mitigate these risks and protect public health effectively.
While this study provides valuable insights, certain limitations must be acknowledged. The study’s focus on a specific occupational group may limit the generalizability of the findings. Additionally, the cross-sectional design precludes causal inferences regarding the observed associations. Further, the study did not conduct an a priori power analysis, as the sample size was constrained by the available funding and logistical resources, which limited the number of participants that could be included. As such, while the findings offer important preliminary insights, the sample size may be insufficient to detect small or moderate statistical differences. Future research with larger, prospectively designed samples is recommended to validate these results. Furthermore, the lack of significant differences in antibody levels among vaccinated and unvaccinated participants calls for further investigation into vaccine effectiveness, particularly against influenza B. Molecular studies examining the genetic and immunological underpinnings of blood group associations with influenza could also deepen our understanding of host-pathogen interactions.
5.1. Conclusions
This study highlights the seroprevalence of influenza antibodies among nurses in Najran and explores intriguing trends related to ABO and Rh blood groups. The findings emphasize the critical role of vaccination in maintaining immunity among healthcare workers while raising questions about the nuanced interplay between demographic, genetic, and immunological factors in shaping immune responses. Moving forward, comprehensive studies that integrate these variables are essential to deepen our understanding of influenza immunity. Additionally, the implementation of robust and effective influenza surveillance systems will be crucial for informing targeted public health strategies, especially for high-risk groups such as healthcare workers.