1. Background
Blastocystis hominis is the most common intestinal parasite in humans and many other animals (1). Infections with the organism are spread worldwide and it is often the most frequently isolated protozoan in parasitological surveys (2-4). In developing countries, B. hominis has higher prevalence (30-50 %) in comparison with developed countries (1.5-10 %) (5, 6). The pathogenicity of B. hominis still has been debated. There are some reports supporting the pathogenic potential of this parasite (7). Clinical features related to B. hominis include nausea, anorexia, abdominal pain, flatulence, and acute or chronic diarrhea (8). However other studies state an opponent view point and it is believed that other factors probably are the causing agents of these symptoms (7, 9-11).
The studies have shown that B. hominis isolates of humans and animals display considerable genetic heterogeneity and have a few subtypes (12). It is supposed that the parasite has 13 subtypes (13), however, to date nine distinct subtypes have been identified (9), which some zoonotic subtypes have found in humans (14, 15). Based on morphologic and pathogenic potentials, there are nine different subtypes, each of them exhibits different features (16-18). Probably each subtype demonstrate its own pathogenicity (19); therefore it is necessary to know specific subtypes of each region.
2. Objectives
The aim of this study was to determine subtypes of B.hominis and relevant prevalence of each in Hamadan city,west of Iran.
3. Materials and Methods
3.1. Samples
Simple random sampling was applied in this study. Forty one samples of B. hominis were detected as positive that was on the basis of an expected prevalence of 37.1 % (20), with a maximum sampling error of 0.15 and a confidence interval (CI) of 95 %. During two months of summer 2011, a total number of 250 fecal samples were collected from the people referred for parasitological examination to Beasat Hospital and a few clinical laboratories of Hamadan city . The samples were transferred to the Parasitology Laboratory of Faculty of Medicine, Hamadan University of Medical Sciences. They were tested for the presence of B. hominis by formalin-ether method. To increase the accuracy, the samples were stained by iodine and trichrome techniques.
3.2. Culture of Blastocystis Isolates
After microscopic observation of the parasite in fecal samples, any debris was removed from positive samples by the use of centrifugation. The positive samples were cultured in Locke-egg (LE) medium and incubated at 37°C for 48-72 hours according to Clark and Diamond (21).
3.3. Extraction of Genomic DNA
Genomic DNA of each isolate was extracted by genomic DNA purification kit (Sinagen Co, Iran) according to the manufacturer’s protocol.
3.4. Genotyping
To identify B. hominis genotypes, seven pairs of Sequences-tagged site (STS) primers [SB83, SB340, SB227, SB337, SB336, SB332, and SB155] were used with PCR technique (22) (Table 1). PCR was performed as following: DNA of 41 isolates was amplified by specific primers. The reaction was carried out within 50 μL final volumes including the following materials: 10 μL DNA, 5 PG of each pair primers, 2.5 mM Cl2Mg, 5 μl PCR buffer pH = 8.3, and 0.5 UI Taq DNA polymerase [Bioprobe]. This combination was entered the cycle described as follows: denaturation at 94˚C for three minutes, and 30 Cycles denaturation at 94˚C for 30 sec, annealing at 56˚C for 30 sec, extension at 72˚C for 30sec, and final extension at 72˚C for five min. The product of PCR was flowed on 1.5 % agarose gel containing ethidium bromide with 100 bp DNA ladder.
| SB83 Sub I | 351 | F:GAAGGACTCTCTGACGATGA | AF166086 |
| R:GTCCAAATGAAAGGCAGC | |||
| SB340 Sub II | 704 | F:TGTTCTTGTGTCTTCTCAGCTC | AY048752 |
| R:TTCTTTCACACTCCCGTCAT | |||
| SB227 Sub III | 526 | F:TAGGATTTGGTGTTTGGAGA | AF166088 |
| R:TTAGAAGTGAAGGAGATGGAAG | |||
| SB337 Sub IV | 487 | F:GTCTTTCCCTGTCTATTCTTGCA | AY048750 |
| R:AATTCGGTCTGCTTCTTCTG | |||
| SB336 Sub V | 317 | F:GTGGGTAGAGGAAGGAAAACA | AY048751 |
| R:AGAACAAGTCGATGAAGTGAGAT | |||
| SB332 Sub VI | 338 | F:GCATCCAGACTACTATCAACATT | AF166091 |
| R:CCATTTTCAGACAACCACTTA | |||
| SB155 Sub VII | 650 | F:ATCAGCCTACAATCTCCTC | AF166087 |
| R:ATCGCCACTTCTCCAAT |
4. Results
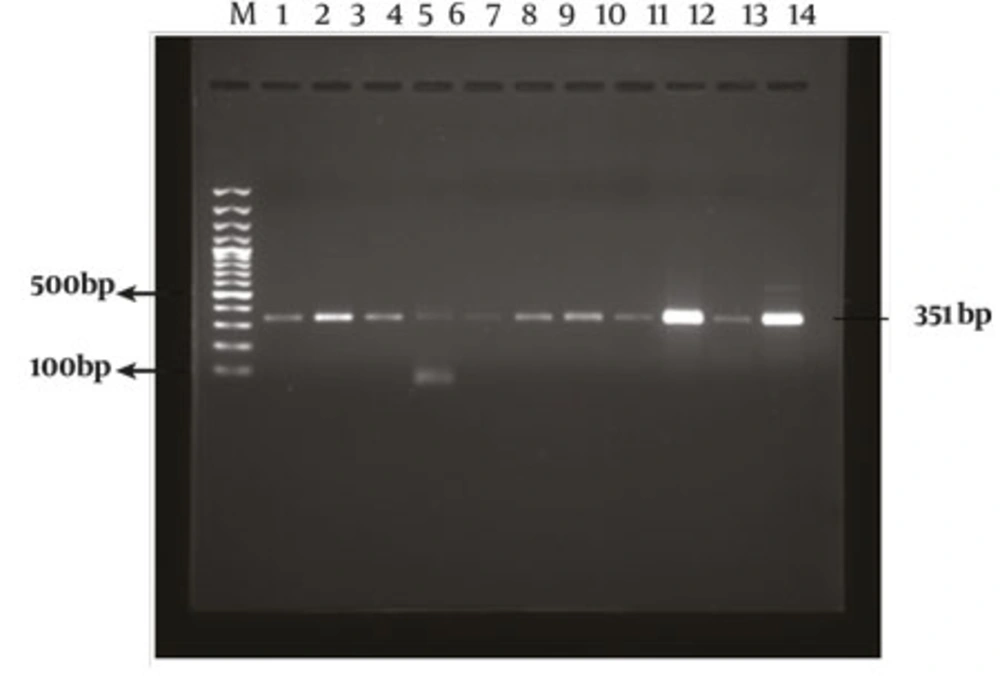
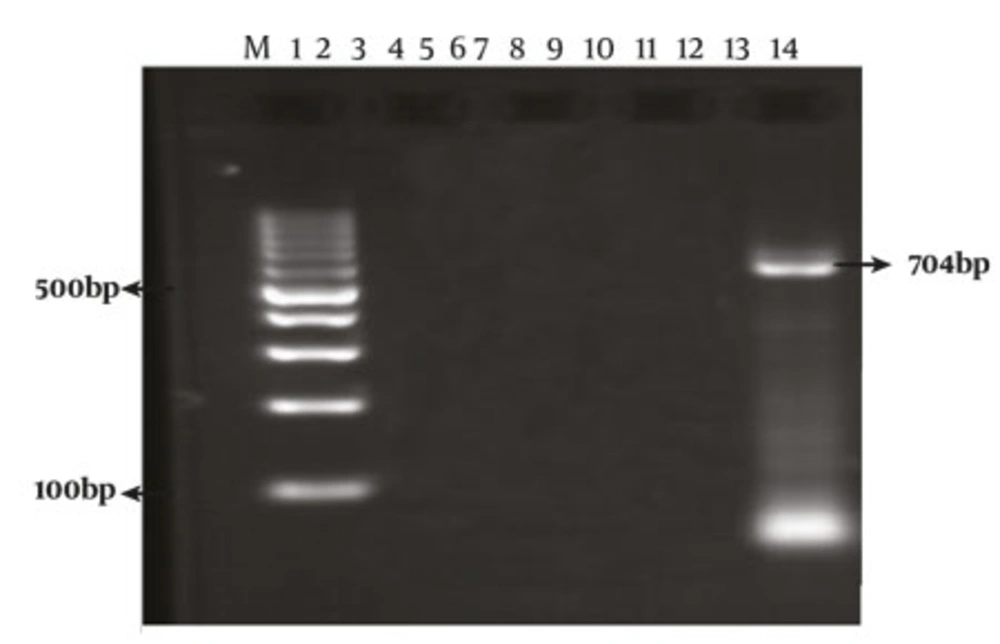
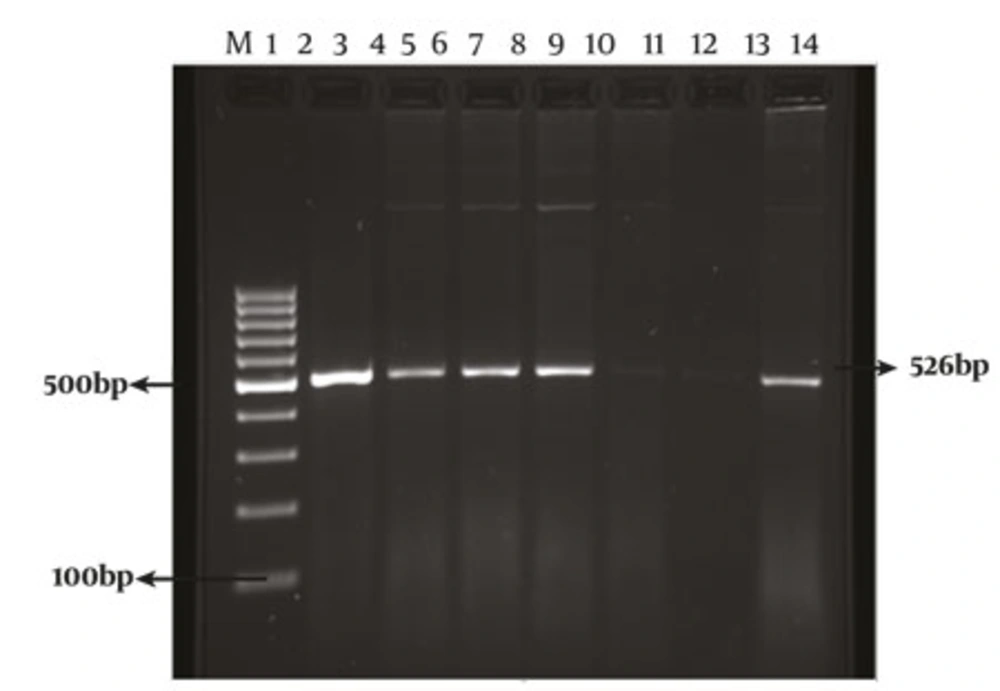
According to table 2, the genotype SB83 was the most identified genotype representing 56.1 % of isolates, followed by genotype SB227 [22 %], mixture of SB83 and SB227 genotypes [14.6 %], and genotype SB340 [7.3 %]. Other genotypes were not detected in this study. In serial order, subtypes SB83 and SB227 were the most frequent isolates in this research. The PCR amplification of B. hominis isolates with the primers SB83 [351 bp], SB340 [704 bp], and SB227 [526 bp] were shown in Figures 1,2,3.
| 1 [SB83] | 23(56.1) |
| 2 [SB340] | 3(7.3) |
| 3 [SB227] | 9(22) |
| 1 [SB83] and 3 [SB227] | 6(14.6) |
| Other genotypes | 0(0) |
| Total | 41(100) |
5. Discussion
Some studies have been conducted on prevalence and pathogenesis of B. hominis in Iran. Prevalence rates of B.hominis have been reported from 0.08 % to 54.5 % (23-29). However, there are few studies with focus on the pathogenesis aspect of B. hominis (25, 27, 30). In this study, the pathogenesis of B. hominis subtypes is not investigated but some differences in virulence between Blastocystis subtypes was shown (9, 20, 31, 32). In many studies, pathogenic potential of subtype 3 has been reported (16, 31, 33-35). Also, some investigations have demonstrated that other subtypes such as subtype 1 were associated with symptoms (20, 31, 34, 36).
Three genotypes were detected in this study including SB83, SB340, and SB227. The results are similar to some other studies performed worldwide (14, 15, 21, 36-38). The frequency of subtype SB83 was more than subtypes SB227 and SB340 that is similar to some other researches (5, 17, 20). The subtypes SB337, SB336, SB332 and SB155 were not detected. In the current study, the most frequent subtype was SB83 that conforms to some other investigations (15, 27, 39). In human isolates, the highest prevalence has been related to subtype SB227 and other subtypes have shown different prevalence rates (9, 20, 21, 37, 39, 40). In human studies, mixed infections with subtypes SB227 and SB83, and with subtypes SB340 and SB337 were reported (41).
This study showed that similar to some other studies (13), the subtype of SB227 exhibits the lowest prevalence rate in this region of Iran [3.7 %]. Furthermore, 14.6 % of the persons were infected by genotypes SB83 and SB227, simultaneously. In some studies, the rate of mixed infections has been observed from 1.1 to 14.3 (5, 19, 21, 39). The frequency of mixed infections with subtypes SB83 and SB340 (5), with SB340 and SB227 (5), and with SB227 and SB336 (39) was low. Because of different growth rates of B. hominis subtypes in culture media, we may have ignored some mixed subtypes in infected patients. Thus, this could be a limitation for current research. Direct PCR method application on DNA obtained from stool samples is suggested (19).
This is a novel study in this region of Iran, which can help the researchers to be aware of epidemiological patterns of this parasite. These data would trigger other epidemiologic and zoonotic studies on different subtypes and hence control clinical manifestations of infection.