1. Background
In the last two decades the incidence of sexually transmitted infections (STIs) is dramatically increased and remains a major public health problem in developing countries. Trichomoniasis is a sexually-transmitted disorder caused by Trichomonas vaginalis which is a flagellated protozoon. This parasitic infection may lead to vaginitis, cervicitis, pelvic inflammatory infection, and tubal infertility in females as well as urethritis and prostatitis in males (1, 2). In addition, it is also related to cervical cancer and an important complication in pregnancy which has been related with prematurity and low birth weight infants (3). Previous data have shown that more than 10 to 50% of women with trichomoniasis are asymptomatic and probably clinical manifestation will develop after half year of infection in 50% of those individuals (3, 4).
The most common symptoms are vulvar itching and malodorous vaginal discharge with yellow-green in color. Other symptoms that may appear include petechiae on the cervix and erythema of the vagina (5, 6). Typical clinical signs occur only in 12% of patients with T. vaginalis infection (7). Peak years of the prevalence for latter infection occur later in life among 20- to 46-year-olds (4). According to the world health organization data, the world wide prevalence of trichomoniasis would be 174 millions and to account for 10 to 25% of vaginal infections (1). Previous studies demonstrated that the prevalence of T. vaginalis infection was 1 to 42% in different geographical areas of Iran (8). The high rate (42%) has probably been detected in special groups.
However, wet mount/potassium hydroxide (KOH) is the conventional diagnostic method for non-viral disorder in the site of vagina which has been infected by T. vaginalis; the sensitivity of this method has been the case of debate, e.g. 58.8% in microscopy versus 95% in culture (9). Although, gold standard for diagnosis of trichomoniasis is liquid culture medium which has been considered the most accurate method, for early and correct identification novel molecular technique were crucially recommended. In the literature, limited data regarding trichomoniasis are available in Zanjan province. The only available report derived from a MD dissertation revealed the infection rate of 6.25% in women referred to Vali-Asr Hospital of Zanjan (10); but there is no up to date information in this region. In additions, there is no information about prevalence of trichomoniasis in pregnant women.
2. Objectives
The purpose of this study was to determine the prevalence of trichomoniasis in pregnant women using two diagnostic methods including direct microscopic examination (KOH) and in vitro culture.
3. Materials and Methods
In this cross-sectional study a total of 1000 vaginal samples from pregnant women who referred to obstetrics clinics at the Hospitals of Zanjan, were examined for detection of T. vaginalis using direct microscopic examination (KOH) and Dorsset culture medium with observation of the parasite (3, 10) between July 2009 to June 2010. The present study was approved by the University Ethics Committee (code number: 882136) which provided written informed consent, subsequently attending underwent clinical examinations.
Gynecologist taken vaginal discharge samples from the vaginal fornix with 2 sterile wet swabs. Parasitological investigation for diagnosis of T. vaginalis of these samples included a microscopic examination with 0.5 ml of normal saline buffer and a smear that was promptly prepared and observed under a light-field microscope. In addition, culturing of samples into the Dorsset liquid medium was performed. Briefly, this diphasic medium was prepared as following recipe; egg, distilled water (1/10 weight of broken egg), streptomycin (2 drops), starch powder (0.5 g) as a solid phase and ringer or saline buffer as a liquid phase. The second swab samples were inoculated and incubated at 37°C for more than 3 days as serially the liquid culture medium was observed daily with wet smears for investigation of T. vaginalis trophozoites. However, patients with blooding more than spotting were excluded from the study. Statistical analysis of data was performed using chi square test, Fisher’s Exact test and Mann-Whitney Test.
4. Results
During one year follow up, one thousand (n = 1000) pregnant women were enrolled and agreed to participate in our study. The age distribution of those individuals adjusted in the present study was significantly different. Most of the patients were between 20 to 30 years old and the mean age of pregnant women was 26.4 ± 6.2 years. It was 58.4% and 41.6% for urban residents and rural residents, respectively. The portion of none educated subjects was12.4% and the remaining showed different levels of education (Table 1). Most of the women (96.4%) were housewife and only 3.6% had official job. The results have shown that, 33 out of 1000 pregnant women (3.3%) were positive with T. vaginalis based on direct microscopic examination.
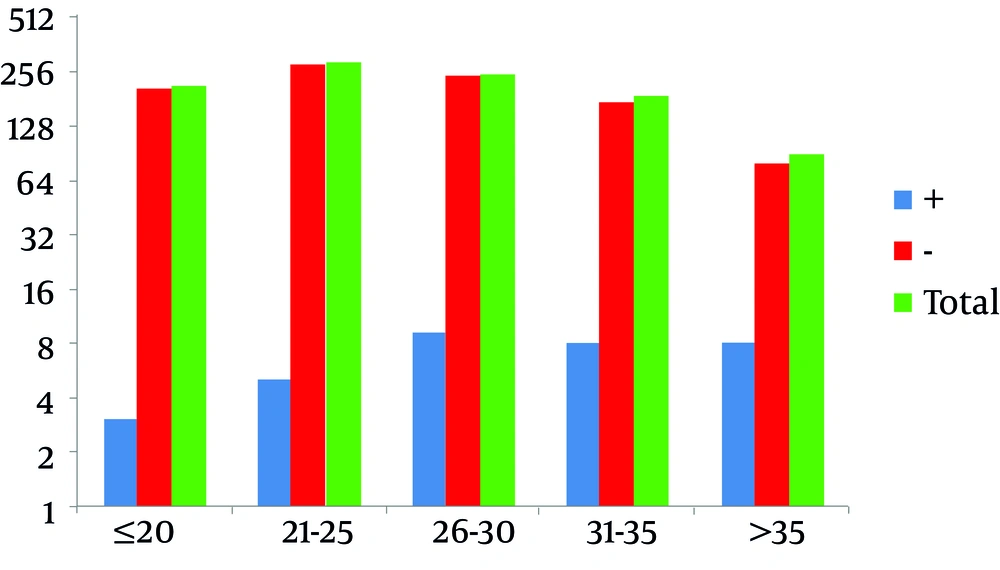
The parasite was consistently observed in 33 out of 1000 samples in Dorsset media culture for T. vaginalis . The results revealed a 100% agreement and correlation between these two performed methods in detection of T. vaginalis. Obtained data have demonstrated different characteristics of the patients with trichomoniasis. Figure 1 shows a significant variation between infected age groups, it means that the incidence of trichomoniasis in oldest individuals was higher than that of younger age groups (P = 0.006) (Table 2). Gestational age in infected women (36.5 ± 4.5) at delivery time was lower than that of healthy women (39 ± 1.9) (P = 0.009). The infected women parity (1.3 ± 1.3) was higher than that of non- infected women (0.7 ± 0.9) (P = 0.004).
As it is shown in Table 2, the prevalence of trichomoniasis in urban residents was high, comparing to infected women in the rural residents (P = 0.04). However, no significant associations were observed between trichomoniasis and occupation (P = 0.288; Table 2), income (P = 0.969; Table 2) and education (P = 0.059; Table 1).
| Education | Trichomoniasis | Total | |
|---|---|---|---|
| Positive | Negative | ||
| No Education | 7 (5.6%) | 117 (94.4%) | 124 (100%) |
| Under Diploma | 23 (3.9%) | 574 (96.1%) | 597 (100%) |
| Diploma | 3 (1.5%) | 194 (98.5%) | 197 (100%) |
| University | 0 (0%) | 82 (100%) | 82 (100%) |
| Total | 33 (3.3%) | 967 (96.7%) | 1000 (100%) |
| Life Features | Trichomoniasis, No. (%) | Total, No. (%) | P value | ||
|---|---|---|---|---|---|
| Positive | Negative | ||||
| Residential Place | Urban | 25 (4/3) | 559 (95.7) | 584 (100) | 0.04 |
| Rural | 8 (1/9) | 408 (98.1) | 416 (100) | ||
| Total | 33 (3/3) | 967 (96/7) | 1000 (100) | ||
| Occupation | Housewife | 33 (3.4) | 935 (96.6) | 968 (100) | 0.288 |
| Other | 0 (0) | 32 (100) | 32 (100) | ||
| Total | 33 (3.3) | 967 (96.7) | 1000 (100) | ||
| Income (US$/mo) | < 200 | 16 (3.2) | 490 (96.8) | 506 (100) | 0.969 |
| 200 - 300 | 13 (3.5) | 363 (96.5) | 376 (100) | ||
| > 300 | 4 (3.4) | 114 (96.6) | 118 (100) | ||
| Total | 33 (3.3) | 967 (96.7) | 1000 (100) | ||
5. Discussion
Our results showed 3.3% prevalence of T. vaginalis infection in pregnant women in Zanjan based on both methods of direct microscopy and in vitro culture. Higher age, higher parity age and urban residency were the studied variables that were significantly associated with higher rate of trichomoniasis. Differences in the infection rates were not significant among different education levels, income levels and occupation. Similar to other studies, increased rate of the infection was associated with raising age (11). This may be due to more sexual contact with increasing age. More frequent infection in women with higher parity also may be attributed to more changes in the genital tracts as one of the predisposing factors to the parasite growth.
The parasitic infection in urban resident women, comparing to rural resident women, was almost twice. This difference is difficult to interpret indeed and may require further investigation in terms of analysis of other related factors. A borderline of significant difference (P = 0.059) of the infection rate was seen among women with different education level with inverse association. Similar results were found in the United States (12); they found an inverse association between education and STIs, including trichomoniasis, in white race women but it was not significant in black women.
No significant association between occupation and trichomoniasis was seen, but this outcome cannot be reliable in this study, as most of the subjects had been housewife. In some studies, e.g. Sutcliffe et al. (13), low household income was correlated with T. vaginalis infection. This is not consistent with our results as we found no significant correlation; probably the household income itself and its differences among the study population are not significant and seem not effective on the infection rate. In epidemiological points of view, these sorts of variables may not influence the Trichomonas infection similarly in all communities. In both methods, in vitro culture and direct microscopic examination, all 33 samples were positive. Although direct method has lower sensitivity in comparison with other methods, including culture (14), the results are not consistent among different laboratories that may be affected by different factors such as the time of microscopic observation and possible intervals between sampling and observation times.
In the present study, we prepared and examined the wet mount directly after the swab sampling. This probably causes no missing of any positive sample with this method and indicates that the direct method is valuable if applied properly. Eastern European guideline for laboratory diagnosis of T. vaginalis encourages the utilization of wet mount of vaginal exudates as the first and more important option (15). It has been shown that the positive rates for trichomoniasis with different methods appear to have large confidence intervals because the prevalence of this infection is low in the studied population, in comparison with other genital infections, such as vulvovaginal candidiasis (22.4%) and bacterial vaginitis (21.5%) (16). Based on the published literature, sensitivity for direct examination is ranged from 35% to 80% (17, 18), while in our study the sensitivity of microscopic examinations was the same as in vitro culture method.
According to the literature, no report about the infection in pregnant women in Iran was available but number of studies on non-pregnant women indicate almost similar prevalence, i.e. 2-3% in Hamedan (19), 2.1-2.6% in Yazd (20) and 3.3-3.6% in Tehran (21). The infection rate in some of other countries was higher, e.g. 25% in USA, 16-74% in African countries (22), 3.4-3.8% in Turkey and 5.1% in India (22). High prevalence of the infection also observed in pregnant women of other countries; 20% in America (23), 17.3-18% in Africa (11, 17), 12.1% in HIV-1 infected pregnant women in Europe (24) and 9.8% in immunocompetent pregnant women in Havana (25). We believed that the prevalence rates during pregnancy vary in the different published papers according to the populations examined.
Several studies have suggested that pregnant women infected with T. vaginalis may be at risk of any of adverse effects of the infection such as premature rupture of membranes, increased preterm delivery rates and low-birth weight infants (21, 26-28). Some comparative studies showed that the pregnant women with trichomoniasis have 30% higher risk of delivering baby with low birth weight or delivering preterm than those without the infection (26). Also more prevalence of some STIs has been reported from pregnant women in some areas (11, 29); alteration of vaginal flora during pregnancy may be of relevant consecutive concerns (30). These indicate the importance of trichomoniasis in this group of women. Number of studies showed that the infection in pregnant women was up to 20% in the United States, 17.3% in Africa and 12.1% in Europe (23, 29, 31). A study on immunocompetent pregnant women in Havana showed 9.8% trichomoniasis (25).
Several factors like hygienic conditions, life styles, living environment and sexual and cultural behaviors can be responsible for these variable levels of infections; however, further investigation in different communities are required for such discussion. Meanwhile, the infection in pregnant women, may have effects on the pregnancy and fetuses, requires particular consideration. The present study found that the infection with T. vaginalis is a health problem and crucially important in pregnant women, correlated with some demographic variables such as age, parity and residential place, and might be considered as microbiological screening tests during pregnancy.