1. Background
Urinary tract infections (UTIs) are common in children around the world with chronic and recurrent infections resulting in a wide range of complications including end-stage kidney disease (1, 2). UTI occurs in about 3 - 5% of girls and 1% of boys, with most girls infected before 5 years; furthermore 60 - 80% of girls acquire a second infection at 18 months old after the 1st UTI (3). In adults, it is estimated that 40% of women and 12% of men will experience a symptomatic UTI, with increasing incidences in their early 20s or after age 85, respectively. About 25% of these women will infect again within 6 to 12 months.
The primary etiologic agent associated with UTIs is the strains of uropathogenic Escherichia coli (UPEC) (4). Although UPEC is an extracellular pathogen but can invade several types of bladder cell that compose the stratified layers of the bladder urothelium. Invasion to host cell simplifies both the establishment and persistence of UPEC in the urinary tract (5, 6). UPEC also persist inside host urothelial cells in a more quiescent state, sequestered within late endosomal compartments (7).
E. coli strains, present in the large intestine are categorized into 4 phylogenetic groups typing, A, B1, B2 and D; these microorganisms may be commensal, which do not harm the host or may be pathogenic, belong to groups A and B1. On the other hand, pathogenic extra intestinal E. coli isolates chiefly belong to phylogenetic group B2 and, to a lesser extent, group D, these isolates harbor specialized virulence factors that aid their successful colonization in the mammalian urinary tract and are responsible for intestinal and extra-intestinal disease (2, 5, 8).
Moreover, extra-intestinal E.coli isolates have some virulence factors which are infrequent among commensal E.coli isolates. Some of these virulence factors are usually encoded on pathogenicity islands (PAIs) (9). Hacker et al. first described the PAI in the late 1980s. (9, 10). These mobile genetic elements are composed of fragments of DNA (10-200 kb) adjacent to tRNA genes and contain insertion sequences, integrases and transposases, and have a G + C content that differs from the host bacterial genome.
2. Objectives
In this study, we compared the presence of various PAI markers and phylogenetic groups in isolated E.coli from the urine of children with UTI and E. coli isolated from healthy children stool samples.
3. Materials and Methods
3.1. Specimens
This is a retrospective study from September 2009 to August 2010 on urine samples collected from 2 - 12 years old children, suspected to UTI and admitted to the nephrology ward of Mofid Children Hospital. Fresh clean catch midstream urine samples from children with UTI were collected in the sterile containers and cultured onto 5% sheep blood agar (Merck, Germeny) and MacConkey agar (Merck, Germeny) by means of calibrated loop delivering 0.0l mL of the urine. Plates were incubated at 37°C overnight and were examined for the growth of microorganisms. All plates showing significant growth (> 105 CFU/mL) were further processed. Also, 50 E. coli isolated from stool samples from healthy children were cultured on MacConkey agar plates and incubated at 37°C overnight. Strains biochemically confirmed and the E. coli were stored in Luria-Bertani (LB) broth (Sigma Aldrich, Germeny) supplemented with sterilized 15% glycerol (Sigma Aldrich, Germeny) at -20 °C for further examination.
3.2. DNA Extraction
Three to five colonies from pure and overnight cultures were suspended in 0.5 mL sterile distilled water and lysed by heating at 95oC for 10 minutes and the supernatant was harvested by centrifugation at 8,000 rpm for 5 minutes. The supernatant was used as template DNA (11).
3.3. Phylogenetic Groups Typing
We used a simple and rapid PCR-based technique consisting of the combination of three DNA markers (chuA, yjaA and tspE4.C2), for phylogenetic groups typing of E. coli isolates (12). The expected fragment sizes were 279, 211 and 152 base pairs (bp), respectively. Multiplex-PCR procedure was performed using 3 pairs of primers in a single reaction. E. coli isolates fell into one of the four phylogenetic groups typing: A, B1, B2 or D. In this study the E. coli strain RS218 belonged to phylogenetic group B2, was used as a control in each PCR assay.
The PCR mixtures were performed in 25 µL volumes containing the following: 1 µL PCR buffer (20 mM Tris-HCl, pH 8.0, 100 mM KCl, 0.1 mM EDTA, 1 M dithiothreitol, 0.5% Tween 20, 0.5% Nonidet P-40; Promega Inc., Madison, Wis.), 200 µM of each deoxynucleoside triphosphates (New England Biolabs, Beverly, MA), 2.5 mM of MgCl2, 2.0 U of Taq DNA polymerase (Promega Inc. USA), and primers as specified in Table 1. Crude extract (2.5 µL) was used as the template DNA for each PCR in Eppendorf Master Cycler gradient PCR system. PCR conditions were as follow: Hot start:94˚C, 4 minutes; 30 cycle (94˚C in 5 seconds,59˚C in 10 seconds,72˚C in 10 seconds) final extension:72˚C in 5 minutes ( 13 ).
3.4. Detection of PAI Markers by Multiplex PCR
All isolates were screened for the presence of PAI ICFT073, PAI IICFT073, PAI I536, PAI II536, PAI III536, PAI IV536, PAI I J96, and PAI II J96 by using two multiplex PCR. Primer sequences of PAI markers in this study are shown Table 1. PCR conditions in A and B reaction were as follow: Hot start: 94˚C 5 minutes; 30 cycle (94˚C in 1 minute, 55˚C in 1 minute, 72˚C in 1 minute) final extension: 72˚C in 10 minute. The PCR products were analyzed by gel electrophoresis on 1.5% BIONEER agarose gels stained with ethidium bromide (Sigma Aldrich, Germeny) (0.5 mg/mL).
| Gene | Size, bp | Primer | Reference |
|---|---|---|---|
| chuA | 279 | F:GACGAACCAACGGTCAGGAT, R:TGCCGCCAGTACCAAAGAC | 20 |
| yjaA | 211 | F:TGAAGTGTCAGGAGACGCTG, R:ATGGAGAATGCGTTCCTCAA | 20 |
| TSPE4.C2 | 152 | F:GAGTAATGTCGGGGCATTCA, R:CGCGCCAACAAAGTATTACG | 20 |
| Multiplex PCR (A) PAI III536 | 200 | F:CGGGCATGCATCAATTATCTTTG, R:TGTGTAGATGCAGTCACTCCG | 2 |
| PAI IV536 | 300 | F:AAGGATTCGCTGTTACCGGAC, R:TCGTCGGGCAGCGTTTCTTCT | 2 |
| PAI IICFT073 | 400 | F:ATGGATGTTGTATCGCGCPS, R:ACGAGCATGTGGATCTGC | 2 |
| Multiplex PCR (B) PAI I536 | 1800 | F:TAATGCCGGAGATTCATTGTC, R:AGGATTTGTCTCAGGGCTTT | 2 |
| PAI II 536 | 1000 | F:CCATGTCCAAAGCTCGAGC, R:CTACGTCAGGCTGGCTTTG | 2 |
| PAI I J96 | 400 | F:TCGTGCTCAGGTCCGGAATTT, R:TGGCATCCCACATTATCG | 2 |
| PAI II J96 | 2300 | F:GGATCCATGAAAACATGGTTAATGGG, R:GATATTTTTGTTGCCATTGGTTACC | 2 |
| PAI ICFT073 | 930 | F:GGACATCCTGTTACAGCACGCA, R:TCGCCACCAATCACAGCCGAAC | 2 |
3.5. Statistical Analysis
The comparisons of proportions were tested using the McNemar test. A value of P < 0.05 was considered as significant.
4. Results
4.1. Phylogenetic Groups Typing
PCR results for three DNA markers (chuA, yjaA and tspE4.C2) were shown in Figure 1. The distribution of UPEC phylogenetic groups typing was as follow: 54 % B2, 34 % D, 8 % A and 4 % B1. The results showed that the distribution of B2 is more statistically significant than group D in UPEC strains (P < 0.05). In 50 fecal E. coli isolates, the distribution of phylogenetic groups was as follow: A; 48%, B1; 26%, D; 22 % and B2; 6%.
4.2. Pathogenicity Island Markers
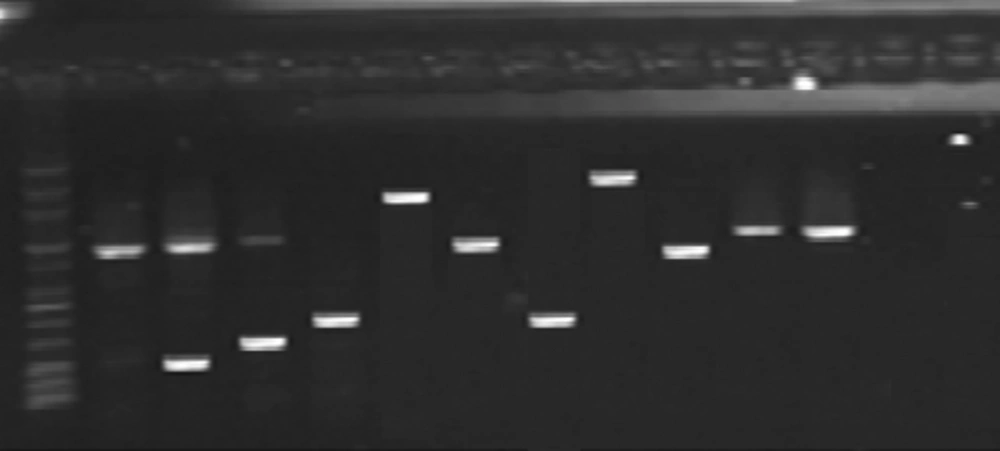
In total, 89% of UPEC isolates carried the PAIs. The distribution of various PAIs showed that the most prevalent PAI were PAI IV 536 (86%) and PAI I CFT073 (74%), respectively. The prevalence of other PAIs was as follow: PAI II CFT073 (37%), PAI II J96 (30%), PAI I 536 (36%) and PAI II536 (22%). PAI III 536 and PAI I J96 were detected only in 6% and 4% of UPEC, respectively. PAI IV 536 (18%) and PAI ICFT073 (14%) were predominant in fecal isolates. Note that some pathogenicity island markers were not seen in fecal strains. The percent of these virulence factors were more predominant in UPEC strains than fecal strains (Table 2). The PCR for detection of PAIs markers was shown in Figure 2.
| Pat hogenicity | UPEC (n = 50), No. (%) | Fecal E. coli (n = 50), No. (%) |
|---|---|---|
| Island genes | ||
| PAI III536 | 3 (6) | 1 (2) |
| PAI IV536 | 43 (86) | 9 (18) |
| PAI IICFT073 | 19 (37) | 3 (6) |
| PAI I536 | 18 (36) | 0 |
| PAI II 536 | 11 (22) | 0 |
| PAI I J96 | 2 (4) | 0 |
| PAI II J96 | 15 (30) | 2 (4) |
| PAI ICFT073 | 37 (74) | 7 (14) |
| Total | 148 (37) | 22 (5.5) |
4.3. Distribution of PAIs According to Phylogenetic Groups in E. coli Isolates
The phylogenetic group B2 containing PAI IV536 was the predominant group among UPEC (Table 3). The total number of PAIs in urinary isolates belonging to phylogenetic groups B2 (27.75%) and D (15%) were significant. In contrast, the number of PAI in fecal isolates collected from phylogenetic group A (1.5%) and D (3%) was the highest. (Table 3) Noteworthy, there was a positive association between phylogenetic group B2 and the presence of PAIs for UPEC (P < 0.001).
| PAI Markers | A | B1 | B2 | D |
|---|---|---|---|---|
| PAI III536 | ||||
| UPEC | 0 | 0 | 2 | 0 |
| Fecal | 0 | 0 | 1 | 0 |
| PAI IV536 | ||||
| UPEC | 0 | 0 | 26 | 32 |
| Fecal | 2 | 1 | 0 | 6 |
| PAI IICFT073 | ||||
| UPEC | 0 | 0 | 18 | 0 |
| Fecal | ||||
| 1 | 0 | 1 | 1 | |
| PAI I536 | ||||
| UPEC | 0 | 0 | 17 | 2 |
| Fecal | 0 | 0 | 0 | 1 |
| PAI II536 | ||||
| UPEC | 0 | 0 | 12 | 0 |
| Fecal | 0 | 0 | 0 | 0 |
| PAI I J96 | ||||
| UPEC | 0 | 0 | 2 | 0 |
| Fecal | 0 | 0 | 0 | 0 |
| PAI II J96 | ||||
| UPEC | 0 | 0 | 12 | 0 |
| Fecal | 1 | 0 | 1 | 0 |
| PAI ICFT073 | ||||
| UPEC | 0 | 1 | 22 | 26 |
| Fecal | 2 | 1 | 0 | 4 |
Lane 1: ladder mid range, lane 2: PAI II 536 (1000 bp) ,lane 3:PAI III536 (200 bp), PAI II 536 (1000 bp), lane 4: PAI IV536 (300 bp), lane 5: PAI IICFT073 (400 bp), lane 6:PAI I536 (1800 bp), lane 7:PAI II 536 (1000 bp), lane 8:PAI I J96 (400), lane 9:PAI II J96 (2300 bp), lane 10 : PAI ICFT073 (930 bp)
5. Discussion
About 70 to 95% of community-acquired and 50% of all hospital acquired infections is caused by E. coli. The molecular biology details of extra intestinal E. coli are poorly understood. Uropathogenic E. coli (UPEC) can grow extra intestinally and this enables them to cause a variety of diseases. It is now demonstrated that there are a subset of fecal E. coli containing some virulence factors which can colonize in periurethral area, enter to the urinary tract and cause symptomatic disease such as UTI. The mentioned pathotypes are named "UPEC" (14). We studied phylogenetic and pathotypic comparison of concurrent urine and fecal E. coli isolates from children in 2010. We analyzed the urine samples and found that the prevalence of phylogenetic group B2 was dominant (5). In our study, E. coli isolates from urine samples dramatically differed from fecal E. coli isolates with regards to some virulence factors such as specific pathogenicity island markers and phylogenetic group B2 and D (15-17). Similar observation has been made by Clermont et al. in 2000 (18). According to the Herzer et al. (19) reports and our study, the pathogenicity islands were enriched in E. coli isolates from urinary tract infections that mostly belong to phylogenetic group B2 and D.
Dobrindt et al. (20) in 2002 studied the genetic structure and distribution of four pathogenicity islands (PAI I536 to PAI IV536) in UPECstrain 536. They also suggested that PAIs were detectable in pathogenic E. coli isolates than fecal ones. Our results showed that the mean number of PAIs per isolate was high in UPEC; however, E. coli isolates belong to groups A and B1 appeared to have fewer pathogenicity island markers than the pathogenic isolates.
We noted that phylogenetic group B2 was uncommon in fecal isolates. This phylogenetic group is highly virulent and when colonize in intestine, may cause of UTI (2).
We can conclude that genomic differences between UPEC and fecal E. coli strains were mainly restricted to phylogenetic groups and large pathogenicity islands.